What is Resistant Starch?
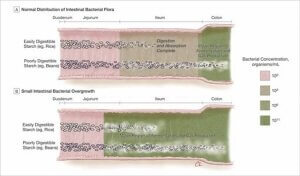
Resistant starch is a type of starch that resists digestion. Starch in general is a large complex carbohydrate used by plants such as oats, corn, potatoes, wheat, rice, nuts, legumes and some fruits such as bananas to store energy. Foods that contain starch make up a large part of many people’s diet. For many years it was believed that starch was completely digested and absorbed in the small intestine. But studies published in the 1980s, based on hydrogen breath testing, showed that oats, wheat, potatoes, corn, and beans contained 10 to 20% malabsorbed, fermentable material. Resistant starch (RS) has been assigned to four groups based on the properties that allow it to resist digestion:[3] RS1 – Physically resists digestion because of a protective matrix or coating surrounding the granules found in whole grains, legumes and seeds. RS2 – Is intrinsically resistant to digestion before cooking. RS2 includes unripe bananas, uncooked potatoes, along with many other foods. RS3 – Retrograded starch is formed when starchy foods are cooked and then cooled. RS4 – Refers to starch that is chemically modified to resist digestion and absorption. RS4 starches are often developed for use in processed foods. Several factors contribute to the formation of resistant starch, and, the relative amount of resistant starch in foods influences the level of malabsorption. The most important, yet often overlooked, factor is the ratio of the two molecular types of starch, amylose and amylopectin. Each type of starch possesses a unique structure and different properties that affect how easily they can be digested and absorbed. Amylopectin starch, which is easy to digest and absorb, is a much larger molecule, containing 10,000 to 100,000 glucose units. At the molecular level amylopectin is highly branched. The large size and branching forms starch granules that are less dense and gelatinize (absorb water) easily when heated in water. Gelatinized starch is easier to digest. The branched, less dense structure also allows the digestive enzyme amylase to work more efficiently, breaking amylopectin down quickly into glucose, which is absorbed rapidly. Amylose starch, which is more difficult to digest and absorb, is both smaller, containing only 100 to 10,000 glucose units, and less heavily branched compared to amylopectin. This linear shape allows amylose to pack more tightly into the less accessible regions of starch granules where it’s more difficult to digest.[4] A high ratio of amylose in starch granules also makes it more difficult to gelatinize (it gelatinizes at a higher temperature), making digestion by amylase enzyme even more difficult. In general, foods that contain more amylopectin (higher glycemic index), such as jasmine rice, short grain sticky rice (also known as glutinous or sushi rice) as well as some varieties of potatoes, such as Russet Burbank, are much easier to digest and absorb than foods containing more amylose (lower glycemic index), such as basmati rice, most long grain rice (except for jasmine), pasta, most wheat, corn, oat and barley products, most potatoes and bananas. Resistant starch escapes digestion and absorption yet is fermentable by certain bacteria common to the large intestine, such as Bifidobacterium, Clostridium and Bacteriodes species. These bacteria contain efficient starch-degrading enzymes and most can break down both amylopectin and amylose starch.[5] Moderate levels of resistant starch are generally well tolerated by most healthy people and, along with other indigestible or poorly digestible carbohydrates such as fiber, fructose, disaccharides, oligosaccharidies and undigested proteins feed our gut bacteria. The main function of bacteria in our large intestine is to salvage energy from these undigested, but energy –rich substances by producing short chain fatty acids (SCFAs) that we can burn, thus improving our food mileage by 30%. But harboring a diverse population of commensal microorganisms in our large and small intestine (referred to as gut microbiome) provides many other benefits including: Reported health benefits of resistant starch linked to fermentation by gut microbes have fostered an interest in using resistant starch for improving overall health and for preventing and treating diseases. Some of the specific health benefits reportedly linked to resistant starch includes: Note: There are a huge number of published studies on resistant starch. I acknowledge that readers may find additional studies to support or refute points made in this post. Please feel free to post these in the comment section, especially hypothesis testing studies in humans. Though positive effects on glucose / insulin modulation have been associated with consumption of resistant starch with fiber or other indigestible carbohydrates,[6],[7] low carbohydrate dieting led to greater improvements in glycemic control, and more frequent medication reduction/elimination than a low glycemic index diet (by definition has more resistant starch) in diabetics.[8] As for lowering cholesterol, I know there are a handful of studies in rats, but I am not aware of similar studies in people. But the bigger question is whether or not lowering cholesterol levels matters since no one can seem to agree on the significance of cholesterol levels in cardiovascular disease. Also, I don’t know of studies in people showing triglycerides are lowered by resistant starch, but I do know resistant starch stimulates the production of SCFAs which are also a form of fat. As for improving satiation, it’s true that rats fed a diet high in resistant starch did not consume more food even though resistant starch is not broken down into glucose. But as Dr. Mike Eades mentions in his blog on resistant starch, the fatty acids produced by bacteria fermenting resistant starch still add calories to our diet, so the real question becomes does resistant starch help people lose weight? Again, I have not seen evidence for this though it may exist. The claim that resistant starch reduces colon cancer risk is based on observational studies suggesting there may be a link between low fiber or high meat consumption and colon cancer,[9],[10] possibly due to the buildup of secondary bile acids such as deoxycholic acid (DOC), believed to be carcinogenic.[11],[12] Another idea is that fermentation of resistant starch produces more butyrate thought to be protective for cancer.[13] Observational study findings however, often turn out to be wrong. Ironically, two species of bifidobacterium (B. longum and B. angulatum) were “significantly associated with high risk of colon cancer”.[14] The researchers determined that total concentrations of bifidobacteria (promoted by RS consumption and partially responsible, via cross feeding, for butyrate production) increased with higher risk of colon cancer. A study that specifically looked at the protective effect of resistant starch in carriers of hereditary colorectal cancer found that resistant starch had no detectable effect on cancer development.[15] While I’m not dismissing possible cancer-protective roles for resistant starch and fiber, I am interested in seeing more definitive studies relating cancer risk to resistant starch and fiber in humans, if they exist. Clearly there is evidence that we and our resident microbes derive benefit from some level of resistant starch and / or other indigestible fibers in our diet. Whether or not we need to supplement our diet beyond what we receive from simply eating some fiber rich green leafy vegetables, avocados, nuts, and some fruit (recommended in the Fast Tract Digestion book series) is an open question. But for most healthy people, there is little down side as long as the amounts are not excessive. Excessive amounts of resistant starch (or any other indigestible carbohydrate) may backfire. Excess fermentable carbohydrates may foster potential harmful properties of gut microbes which may include: My biggest concern is that resistant starch has the potential to cause or perpetuate digestive problems if and when excessive fermentation occurs in the wrong place, mainly the small intestine. To be on the safe side, people with Small Intestinal Bacterial Overgrowth (SIBO)-related digestive illnesses such as GERD, IBS and Celiac disease, to name a few, would be best served by consuming lower levels of resistant starch because it behaves much like fermentable fiber. If you have read my three part article on fiber, you know where I am coming from. Also find out more about SIBO on this site. There is clear evidence in the scientific literature (summarized in the Fast Tract Digestion books) that lactose, fructose, fiber and sugar alcohols are subject to various degrees of malabsorption similar to the malabsorption of resistant starch and can promote SIBO-related digestive illness, such as IBS, GERD, Celiac disease and other functional GI conditions. SIBO can cause diarrhea, constipation, bloating, excessive gas, belching, acid reflux, vitamin and mineral malabsorption and damage the critical digestive machinery of the small intestine. Keep in mind that (overgrowing) gut bacteria produce more than butyrate and other SCFAs. They also produce a large amount of gas in the form of hydrogen, carbon dioxide and methane in some cases. That’s enough gas to cause well documented explosions during intestinal surgery.[16] It’s these gases that are responsible for bloating, acid reflux (read about my original theory connecting SIBO with GERD in Heartburn Cured), abdominal pain, cramping, respiratory problems and other symptoms of IBS, GERD, asthma and other SIBO-related conditions. But the idea that fructose, lactose, fiber and sugar alcohol can feed SIBO but resistant starch can’t, makes little sense to me. Here is some evidence (excerpted from the Fast Tract Digestion books) that led me to conclude that resistant starch should be avoided by people with SIBO-related illness until SIBO and symptoms are under control. Bacterial overgrowth and Starch Digestion.[19] The Fast Tract Diet for SIBO-related conditions allows up to 45 grams of difficult-to-digest carbohydrates per day, including resistant starch. The quantity of these resistant carbs per serving is available for hundreds of foods in the appendices of the Fast Tract Digestion books and can also be calculated by the Fermentation Potential (FP) formula provided in each of the Books. Promoting a state of fermentable substrate limitation in the gut is, in my view, healthier than promoting a state of fermentable substrate excess and more consistent with Paleo diet concepts. A lean diet for our gut microbes fosters healthy competition in the gut that will favor the survival of well adapted organisms best suited to be our partners in digestion and health. We know that excess malabsorbed carbohydrates are linked to conditions associated with SIBO and there is reason to believe that resistant starch may contribute to imbalances is the gut microbiome including SIBO in susceptible people. OK, take a break. Then you can read RS Part 2: Resistant Starch Friend, Foe or Lover. [1] Anderson IH, Lavine AS, Levitt MD. Incomplete absorption of carbohydrate in all-purpose wheat flour. N Engl J Med. 1981 Apr 9;304(15):891-2. Levitt MD, Hirsh P, Fetzer CA, Sheahan M, Levine AS. H2 excretion after ingestion of complex carbohydrates. Gastroenterology. 1987 Feb;92(2):383-9. [2] Hallfrisch J, Behall KM. Breath hydrogen and methane responses of men and women to breads made with white flour or whole wheat flours of different particle sizes. J Am Coll Nutr. 1999 Aug;18(4):296-302. [3] Englyst HN, Trowell H, Southgate DA, Cummings JH. Dietary fiber and resistant starch. Am J Clin Nutr. 1987 Dec;46(6):873-4. Bird AR, Brown IL, Topping DL. Starches, resistant starches, the gut microflora and human health. Curr Issues Intest Microbiol. 2000 Mar;1(1):25-37. [4] Bird AR, Brown IL, Topping DL. Starches, resistant starches, the gut microflora and human health. Curr Issues Intest Microbiol. 2000 Mar;1(1):25-37. [5] Macfarlane GT, Englyst HN. Starch utilization by the human large intestinal microflora. J Appl Bacteriol. 1986 Mar;60(3):195-201. A A Salyers, J R Vercellotti, S E West, and T D Wilkins Fermentation of mucin and plant polysaccharides by strains of Bacteroides from the human colon. Appl Environ Microbiol. 1977 February; 33(2): 319–322. Wang X, Conway PL, Brown IL, Evans AJ. In vitro utilization of amylopectin and high-amylose maize (Amylomaize) starch granules by human colonic bacteria. Appl Environ Microbiol. 1999 Nov;65(11):4848-54. [6] Nilsson AC, Ostman EM, Holst JJ, Björck IM. Including indigestible carbohydrates in the evening meal of healthy subjects improves glucose tolerance, lowers inflammatory markers, and increases satiety after a subsequent standardized breakfast. J Nutr. 2008 Apr;138(4):732-9. [7] Behall KM, Scholfield DJ, Hallfrisch JG, Liljeberg-Elmstahl HG (2006) Consumption of both resistant starch and beta-glucan improves postprandial plasma glucose and insulin in women. Diabetes Care 29: 976–981. [8] Westman EC, Yancy WS Jr, Mavropoulos JC, Marquart M, McDuffie JR.The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab (Lond). 2008 Dec 19;5:36. doi: 10.1186/1743-7075-5-36. [9] Armstrong B, Doll R. Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int J Cancer. 1975 Apr 15;15(4):617-31. [10] A. Cassidy, S. A. Bingham, and J. H. Cummings. Starch intake and colorectal cancer risk: an international comparison. Br J Cancer. 1994 May; 69(5): 937–942. [11] Nagengast FM, Grubben MJ, van Munster IP. Role of bile acids in colorectal carcinogenesis. Eur J Cancer. 1995 Jul-Aug;31A(7-8):1067-70. [12] Bernstein C, Holubec H, Bhattacharyya AK, Nguyen H, Payne CM, Zaitlin B, Bernstein H. Carcinogenicity of deoxycholate, a secondary bile acid. Arch Toxicol. 2011 Aug;85(8):863-71. doi: 10.1007/s00204-011-0648-7. [13] Pryde SE, Duncan SH, Hold GL, Stewart CS, Flint HJ. The microbiology of butyrate formation in the human colon. FEMS Microbiol Lett. 2002 Dec 17;217(2):133-9. [14] Moore WE1, Moore LH. Intestinal floras of populations that have a high risk of colon cancer. Appl Environ Microbiol. 1995 Sep;61(9):3202-7. [15] Mathers JC, Movahedi M, Macrae F, Mecklin JP, et.al. Long-term effect of resistant starch on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet Oncol. 2012 Dec;13(12):1242-9. [16] Dener IA, Demirci C. Explosion during diathermy gastrotomy in a patient with carcinoma of the antrum. Int J Clin Pract. 2003 Oct; 57(8):737-8. Bigard M-A, Gaucher P, Lassalle C. Fatal colonic explosion during colonoscopic polypectomy. Gastroenterology 1979; 77: 1307-1310. [17] Macfarlane GT, Englyst HN. Starch utilization by the human large intestinal microflora. J Appl Bacteriol. 1986 Mar;60(3):195-201. Wang X, Conway PL, Brown IL, Evans AJ. In vitro utilization of amylopectin and high-amylose maize (Amylomaize) starch granules by human colonic bacteria. Appl Environ Microbiol. 1999 Nov;65(11):4848-54. [18] Bouhnik Y, Alain S, Attar A, Flourié B, Raskine L, Sanson-Le Pors MJ, Rambaud JC. Bacterial populations contaminating the upper gut in patients with small intestinal bacterial overgrowth syndrome. Am J Gastroenterol. 1999 May;94(5):1327-31). Ghoshal U, Ghoshal UC, Ranjan P, Naik SR, Ayyagari A. Spectrum and antibiotic sensitivity of bacteria contaminating the upper gut in patients with malabsorption syndrome from the tropics. BMC Gastroenterol. 2003 May 24;3:9. [19] Lin HC. Small intestinal bacterial overgrowth: a framework for understanding irritable bowel syndrome. JAMA. 2004 Aug 18;292(7):852-8. [20] Hallfrisch J, Behall KM. Breath hydrogen and methane responses of men and women to breads made with white flour or whole wheat flours of different particle sizes. J Am Coll Nutr. 1999 Aug;18(4):296-302. [21] Biesiekierski JR, Newnham ED, Irving PM, Barrett JS, Haines M, Doecke JD, Shepherd SJ, Muir JG, Gibson PR. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 2011 Mar;106(3):508-14; quiz 515. [22] Boivin M, Zinsmeister AR, Go VL, DiMagno EP. Effect of a purified amylase inhibitor on carbohydrate metabolism after a mixed meal in healthy humans. Mayo Clin Proc. 1987 Apr;62(4):249-55. [23] https://www.webmd.com/diet/features/the-truth-about-starch-blockers. [24] Mitchell, Richard Sheppard; Kumar, Vinay; Robbins, Stanley L.; Abbas, Abul K.; Fausto, Nelson (2007). Robbins basic pathology. Saunders/Elsevier. ISBN 1-4160-2973-7. [25] Fridge JL, Conrad C, Gerson L, Castillo RO, Cox K. Risk factors for small bowel bacterial overgrowth in cystic fibrosis. J Pediatr Gastroenterol Nutr. 2007 Feb;44(2):212-8. [26] Austin GL, Dalton CB, Hu Y, Morris CB, Hankins J, Weinland SR, Westman EC, Yancy WS Jr, Drossman DA. A very low-carbohydrate diet improves symptoms and quality of life in diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009 Jun;7(6):706-708. Yancy WS Jr, Provenzale D, Westman EC. Improvement of gastroesophageal reflux disease after initiation of a low-carbohydrate diet: five brief cased reports. Altern Ther health med. 2001. Nov-Dec; 7(6):120,116-119. Austin GL, Thiny MT, Westman EC, Yancy WS Jr, Shaheen NJ. A very low-carbohydrate diet improves gastroesophageal reflux and its symptoms. Dig Dis Sci. 2006 Aug;51(8):1307-12. General Health Aspects of Resistant Starch
Caution for People with GI Issues


Norm thanks for bringing clarity to the latest paleo bandwagon!
Here’s my issue.
People keep commenting on this issue who HAVEN’T TESTED IT THEMSELVES.
On Richard Nikoley’s blog is a guy named Tatertot, who has assembled pretty massive amounts of knowledge on RS. It has been tested EXTENSIVELY.
You have to get the right amount. In humans, this is 30 to 50 grams per day.
Also, I’d love to see the same experiment done above with food that obviously is going to be problematic for someone with SIBO (bread products) be done with Unmodified Potato Starch. I mix mine with Kefir.
Also, Tatertot saw his blood glucose levels stabilize nicely with RS. His meal after the meal containing RS, even if high glycemic, did not cause a huge spike in blood glucose, and it came back down to baseline much faster.
I would recommend folks try it out themselves. You can get Bob’s Red Mill unmodified potato starch for about $5 for 24 ounces. Take 4 TB per day.
It’s not a miracle. There are no silver bullets to health and obesity. However, we KNOW that health is directly tied to the gut. And we KNOW that RS increases beneficial bacteria SIGNIFICANTLY.
Hit up https://freetheanimal.com/2013/04/resistant-assimilation-resistance.html.
Cody, I appreciate your perspective as no problem can be solved without an open discussion on the pros and cons and the science. I have read Richard’s and Tatertot’s posts and I state clearly in the article that there are many positive aspects of feeding our gut microbes with indigestible carbohydrates including resistant starch. I also believe that these same molecules that can be beneficial can also be detrimental when consumed in excess, particularly with people who have conditions caused by SIBO. By the way, I am not playing favorites. My books recommend limiting fiber and sugar alcohols, staples of some low carb diets.
I don’t recall Tatertot saying he suffers from GERD, IBS or celiac disease, but many people do. I suffered from chronic acid reflux for many years until I realized that limiting carbohydrates, including lactose, fructose, fiber, sugar alcohols and resistant starch controlled my symptoms. We should continue to tease this apart as you mentioned but some of that work has already been done. Not everyone has lactose intolerance or fructose intolerance, but many do. My books on Heartburn, IBS and SIBO have as a goal reaching a symptom-free baseline by limiting all five types of carbs mentioned above. Using the fermentation potential calculation (or reference tables), I recommend keeping total difficult-to-digest carbs to under 40 grams per day. Once symptom free, people with a tendency to develop SIBO are in a perfect position to do exactly as you say – try it for themselves. But until they have a symptom-free baseline, how can they tell whether it’s helping or hurting?
Chris Kresser, a well-respected health care practitioner and researcher (and paleo-template advocate) has written that autoimmune thyroiditis and SIBO are linked. Yet, curiously, he actually advocates increasing the amount of RS to treat Hashimoto’s. This really confuses things, but my instincts tell me that low RS is the way to go. Any thoughts on this?
You can see his article here:
https://chriskresser.com/your-gut-microbes-and-your-thyroid-whats-the-connection/?mc_cid=1d68c91e26&mc_eid=6aa4705a90
Thanks!
It’s about perspective, isn’t it?
I worry a bit that a lot of people will read Mark Sisson’s 30 second consideration of RS or Mike Eades dismissive hand wave of RS and not at least consider it.
For people with intestinal issues, there are loads of potential problems with so many things.
My mom got a nasty C Diff infection. She thought yogurt would be helpful (and frankly, without knowing better, so did I). It made things much, much worse.
I bet some RS in the form of raw potato starch would have really helped her good critters come back and potentially overtake C Diff rather than have the standard 3 month trial and tribulations of some seriously awful antibiotics.
So to your point, (and I’m not real familiar with some of these gut maladies, because I’ve been blessed to this point to not suffer in this way), it’s all about context.
Something that people with religious like zeal towards diets tend to lack.
For me, I suffer with chronic obesity. Something that has been made worse by things like extreme stress, lack of sleep, and artificial sweeteners. All things none to all but destroy healthy gut bacteria. RS seems like a nice way to help heal my particular gut issues.
We shall see.
Cody, I understand that adding resistant starch to your diet is working for you and that’s really great. As for Dr Mike Eades and Mark Sisson not giving this particular subject all the attention you believe it deserves, you may have a point, but I know both of these individuals and their writings over the years have earned them my respect. Both possess a deep understanding of paleolithic diets. Mark’s Primal Law #1 in The Primal Blueprint is: “Eat lots of plants and animals” and Protein Power recommends an ample supply of “green leafy vegetables tomatoes, peppers, avocados, broccoli, eggplant, zucchini, green beans, asparagus, celery, cucumber, mushrooms and salads” – not exactly devoid of indigestible carbohydrates.
I agree with your point about balance. The fact that we evolved a gut microbiome along with the capability to gain nourishment from indigestible plant matter argues for a role of fibrous (including resistant starch) plants in our ancestral diet. But, to Danny’s point, there is an argument to be made that plant eating was more about survival between kills with protein and fat representing our main diet. Here is a blog article with archeological references supporting this notion.
Not to beat a dead horse, but my main concern is helping people with digestive problems involving SIBO get better. After that, I feel like my job is done.
I don’t know Norm. I think that we need to pay attention to butyrate production (along with K2 production) by fermentation of some of these plant materials. Resistant starch is one of the highest (along with pectin) for butyrate production via fermentation in the colon, at least according to this article:
https://huntgatherlove.com/content/human-colon-evolution-part-4-secrets-butyrate
Along with pectin, RS seems to be needed by the critters in our colons to create butyrate, and with butyrate production in the colon, it sounds like quite a few intestinal/digestive issues go away.
Some people say just eat butter to get butyrate, but butter doesn’t make it to the colon, now does it?
What about a butter enema? I’m only half kidding. I’m thinking that if these critters need RS, Pectin, and other forms of soluble fiber to do their jobs and some folks simply cannot eat those foods because it makes their conditions worse, than what about a suppository made of RS, Pectin, and inulin? Along with good bacteria?
I do get that you, Mark, and Mike are helping people. And for that I’m EXTREMELY grateful. Plus, I appreciate that you are open to discussion and rubbing elbows with random strangers on the internet. It’s pretty awesome.
Good conversation Cody. We agree on more than we disagree on for sure. How much resistant starch is best for health and disease is a topic that deserves more attention. And interesting ideas on Butt, Butter and Butyrate.
On probiotics, I take a cautious position. The more we learn about the vast complexity of the gut microbiome, the more I stress avoiding anything that upsets that including antibiotics but also swamping the intestines with high numbers of simple mixtures of two – five different organisms. Fecal transplants, properly controlled is perhaps one of the most exciting fields in digestive science today.
I did protein power/atkins for many years. Initially it afforded me quite a bit of weight loss but eventually it didn’t work anymore no matter how low carb I went. I had IBS/colitis and the low carb no starches helped keep that at bay but anytime I ate starches sugar it came back. I discovered the specific carb diet and this made a lot of sense and fit my symptoms. I suspected a screwed up gut microbiome at fault for a lot of my problems. I didn’t realize the low carb diet might be exacerbating it. But I had no choice because I got colitis symptoms if I ate starches. Then I discovered berberine. Berberine and berberine containing herbs are in a class called mucous membrane alternatives or tonics. The science on them has shown that they are not antibiotic but that they heal and alter toward normal the immunity in the gut by normalizing immunoglobulins, phagocytes and other immune cell function and mucous secretion. This in turn allows the gut mucosa to overcome infections. I started taking berberine 1/2 capsule per day gradually building to 1 1/2 capsule daily. Within less than a week I could eat anything with no problems with perfectly formed normal stools. I waited a few months to allow complete healing. Now I am using resistant starch along with a few probiotics with very good results. I am sleeping way better my metabolism is improved I feel warmer and seem to be having subclinical hypothyroidism resolving as I’m having to cut down on thyroid else I feel hyper. I don’t believe in low carb anymore. I think it is nothing more than a band aid that is jerry rigging but not really fixing the cause of the problems people have and that long term it has negative consequences. There are so many people who tend toward leanness on the globe who eat a lot of carbs that the whole carbs are the villain mentality is rather absurd. It makes much more sense that there is something amiss that us keeping people from handling carbs or food in general properly causing weight gain and other problems. I believe the gut microbiota is a large part of this. Think about it. In the industrialized countries we are often not breast fed or minimally breast fed pumped full of antibiotics and other gut altering drugs eat junk food etc. in less developed countries we don’t see all the obesity no matter how much carbs they eat but they tend to extensively breast feed and don’t take antibiotics like candy or other drugs and junk food.
Hi… I hope you still read my comment. I am having the same experience as you regarding thyroid. I also started with resistant starch (along with sodium butyrate, fermented foods and a clostridium butyricum supplement) recently and it made me feel very hyper. I cut down my thyroid hormone dosage substantially but I still feel hot all the time. I am now not so sure anymore if my body is using the thyroid hormones more effectively now or if this is a direct effect of too much butyrate in the system. Did your hyper symptoms disappear after reducing your thyroid meds?
Dear Lisa, I know it is years ago, but I just read your response about taking berberine. Are you still using it? Has it helped. I suffer with GERD and wonder if it may be helpful? Just wondering how you are doing now? Please email me at sandylevine@aol.com, I really would appreciate it.
What a fabulous post, Norm! I for one am really grateful! Gluten free or not, there are certain whole grains, beans and fruits that cause horrible acid reflux. If I follow your protocol and eat low on the FP chart, I have no problems. By the way, it helped my young nephew, too. He had terrible reflux until I gave him your book, Fast Tract Digestion – Heartburn!
Hi Alana! Nice to hear from you and thanks for sharing the book with our nephew. How old his he?
Norm,
My nephew is 25 years old (OK! That’s young to me!) He, like so many others in my family, has suffered terribly with acid reflux. He lives and works in Japan and came back to the U.S. a couple of months ago to see the doctors here for treatment. But quite frankly, it was to no avail. I gave him my copy of your book, we looked over your website, he took the book back to Japan and has reported (several times) that he no longer has acid reflux. My sister tells me he read the book and carried it with him until he had to pack it for his trip back to Asia! I only wish I had known what I know now. I could have helped my mother and my uncle (who died of esophageal cancer), and even my grandfather. Your work has done the greatest service for those of us facing these sorts of gut issues. I tell my clients about your book and your work; I want everybody to know!
That’s young to me too! So happy to hear that your nephew was helped by the book. The Japanese had very little heartburn until introducing more Western foods into their diet. Sorry to hear that your mom, uncle and grandfather suffered with esophageal cancer. Unfortunately, PPIs have not helped reduce the number of these cancers because they don’t actually stop the reflux itself. That’s one of the key benefits of the Fast Tract program.
Thanks Norm! Actually, it was my uncle who died from esophageal cancer. He sucked on Rolaids all day long! My Mom and my grandfather had reflux but not cancer of the esophagus. Still, I remember my mom took Tagamet daily! I refuse to do that!
Take a read of how not to die. There is the sollution to acid reflux and all the other things that await anyone eating in a modern way. Sure acid reflux is bad. But the acid reflux inducing diet kills in many other ways that dont give a warning. Introduce slowly more and more greens in your diet and feel great! Had acid reflux on high fat sweet foods. Fiber is the way to stop these and without side effects except you having to eat more bulk and move to a fresh market often. RS in the form of fiber or starches is feeding your gut microbiome and is important. Fibers are turned into SCFA that power your body in a nuce way. give some time for your gut flora to adjust by introducing more whole plant foods.
Norm – What a great article! This kind of exposure is exactly what I was hoping for in working with Richard Nickoley on his RS series: https://freetheanimal.com/2013/05/resistant-starch-4-letter-word-nope-goal-create-mashed-potatoes-a-diabetic-can-eat-every-day.html
It makes me very happy that you read them and took the time to put together this magnificent post!
You are correct in your assumptions that I have no digestive issues. I had full-blown ‘metabolic syndrome’ from 1999-2010 when I was 35-45 years old, I ballooned up to 250lbs, had fatty liver disease, pre-diabetic, high chol, trigs, and bp, hypothyrod, sleep apnea, and gout. 1 year of Mark Sisson’s Primal Blueprint had me down to 170 pounds and over all my big troubles.
Eating a low carb paleo diet for the past 3 years has kept me healthy and looking into ways to increase health even more. I began following Paul Jaminet’s Perfect Health Diet recommendations by adding a few servings of potatoes and rice a day. I also started reading all I could on Resistant Starch.
Most of the studies on RS showed the highest benefits with 20-50g of RS per day. I tried to get that from foods, but found the best I could do with paleo foods/safe starches was about 10g/day. I thought, ‘why not just use potato starch?’ as was done in so many studies. I got to checking–it seemed perfectly safe.
I have been eating 4TBS of potato starch per day, which is approximately 32g RS, for the last 6 weeks. Other than a bit more flatulence from certain high-fructose foods, I feel great. My FBG has dropped from the 110-130 range to the 85-95 range. My cholesterol numbers have improved since last fall greatly, and I feel a satiety like never before.
The biggest issue I see, there are NO compendiums of anecdotal evidence on people who have specifically increased RS in their diet! It ALL studies. This is especially true of people eating RS on a a paleo diet–no studies even address that.
Usually, there is a pile of anecdotal evidence on things like paleo eating, low-carbing, using vinegar for health, etc… then the studies follow. With RS it’s the exact opposite.
Thanks for your time!
Tatertot
Tatertot,
So glad you joined in and congratulations on your personal success. I really enjoyed your article. Somewhere I saved the link to all the reference material you collected and graciously shared. People like yourself who read, think and experiment can change the direction of science by stimulating debate and reflection. I still remember how excited I was when my own experimentation on my acid reflux and carbs led to a new theory on the etiology of this disease. The previous idea “transient lower esophageal sphincter relaxations” prevailed in the scientific literature for over 50 years. I will be presenting this novel theory for the first time next week to gastroenterologists at the Digestive Disease Weekly meeting in Orlando.
Keep at it and please update us on your progress.
Richard is working on a new post with lots of really good links that should satisfy everyone.
One paper in particular I found very enlightening, as you may, too: https://physrev.physiology.org/content/81/3/1031.full
I was particularly intrigued by Figure 3, and this blurb in the text: “The distal large colon and rectum are the regions of the large bowel with the most limited supply of SCFA and are the site of most pathology.”
Study after study show that populations with the most limited intakes of RS have large intestinal disease throughout the large intestine. As RS increases, pathology moves distally. In countries with medium RS intakes, problems are seen only in the transverse and descending colon, countries with high RS intakes generally see very, very little colon problems and then only at the distal end of the descending colon.
I look forward to reading it. Thanks.
Norm:
Fabulous work and I think you’ve really advanced the discussion, giving a perspective that says: this RS deal may not work for everyone and here’s why. On my two posts on the issue, some people trying this have already reported in about massive gas issues (I’ve had that intermittently). That led me to begin searching, led me to SIBO from various clues and now you’ve just confirmed for me that those suspicions were correct.
I was a lifelong GERD sufferer who was on PPIs for years and got off them via paleo. Over the last 6 years of varying adherence, here’s my general take, for me:
1. Pure paleo, low, moderate or high carb (tubers, potatoes) knocks out GERD.
2. Cheats with processed food brings on GERD.
3. IF 1-2x per week, 24-30 hrs gives lots of headroom, such that moderate #2 will not bring on GERD.
4. Alcohol beyond very moderate use will bring on GERD (and combined with too much #2 makes it nuclear—think: getting drunk & eating pizza), but #3 provides headroom in that as well.
To sum it up, good adherence to paleo + IF affords leeway in terms of #2 OR #3, but generally not both at once, unless very moderate.
Make sense?
OK, now about my own RS experience and gas. For the first couple of weeks, 4 T of Bob’s Red Mill Potato Starch per day, usually 2T 2x per day, stirred into either milk or kefir. No problems. Sometimes the whole 4T at once. No problems. Then one evening I did 4T in kefir and within an hour experience the most hilarious gas experience of my life. I’m talking enough energy to light a small neighborhood, delivered in intervals of like a 1-3 minutes apart and for like 24 hours. Zero pain, little gurgling, no discomfort, as though they come out of nowhere. Like one second you’re completely normal and a second later have the most massive fart it’s unbelievable.
And here’s the other thing: they are either completely not malodorous, or only slightly so (this helps quite a lot, if other people happen to be anywhere around because a full 10-second firing can really create quite a cloud of despair over a significant radius :).
So I can’t put my finger on it. Sometimes gas, sometimes no. Doesn’t seem to matter whether taken with kefir, milk, or water. I haven’t tried enough variables to determine whether dose at one time is a big factor and how close to a meal.
Fasting may have an impact. Last Wed beginning at 1pm, I initiated a full 30 hr fast (1st time in a long time). Water, coffe, tea only—unsweetened. At the end of the fast I hit the gym for a hard workout, came back, took 10g of BCAAs and 4T potato starch in water, then went for dinner. Huge plate of roast beef au jus, mashed taters & butter au jus, big salad with restaurant blue cheese dressing. No issues. No gas, no GERD.
So, I’m perplexed a bit.
Given the above, particularly the non odor of the gas, might you be inclined to think it’s too much PS in one dose getting fermented in the colon, or SIBO?
Thanks for any clues you can offer.
Hi Richard,
Glad you could join and with your similar experiences with GERD, I look forward to hearing more about your ideas. Also, thanks for your excellent blog. Mike Eades got me started on this by pointing out your article. The most important thing is that you have found out how to control your reflux with diet and stopped the PPIs saving yourself from potential long term health risks. Farting won’t kill you.
There are a couple of things that stand out in the recent experiences you related. The lack of odor is explained most easily because the odorous gas comes from sulfur present in proteins. So gas from starch and fiber will be less unpleasant for sure – some good news. As for why you get gas sometimes and not others, the answer is a bit more complex. There are a number of things going on all at once. Some bacteria are what they call homolactic (they ferment carbs and produce mostly lactic acid and no gas). Other bacteria (more common to colon) are heterolactic (ferment carbs and produce SCFAs and gases H2, CO2, and sometimes CH4). At the same time, much of the gas, particularly CO2 is being rapidly absorbed into the blood stream and exhaled from the lungs. The third factor is the presence of bacteria (mostly archaebacteria) that use H2 as an energy source and produce methane. Add to that bacteria than can use H2 as an energy source and synthesize carbohydrates from C02. Interestingly enough, C.diff has that capability.
It sounds like we have some general agreement that diet effects health and many of those effects involve intestinal bacterial fermentation. Finding the optimal diet for maintaining good health and for treating health problems – so often linked to digestive issues is a worthy goal. Let’s get at it!
Keep up the good work on your incredible and funny blog,
Norm
No Disease That Can Be Treat-
ed By diet Should Be Treated
With any Other Means.”
-Maimonides
Richard, Sorry, should have asked earlier. What does this statement mean ” IF 1-2x per week, 24-30 hrs gives lots of headroom, such that moderate #2 will not bring on GERD” ? What is “IF”?
IF stands for Intermittent Fasting. There are several popular protocols, including LeanGains, Fast 5, and Eat Stop Eat.
Norm – I’m probably being a bit parochial with my interest in RS, but getting good discussion going was my real intent.
In a LC paleo diet, the only fermentable substrate reaching the colon are the limited bits of oligosaccahrides from certain veggies, probably amounting to 1-3g/day.
A SAD diet provides 3-8g/day from most estimates, and it seems to be woefully inadequate to stimulate SCFA production required to feed approximately 5 feet of colonocytes.
Almost every author and blogger who sees this connection jumps to the conclusion that we should eat more RS containing foods like cold potatoes and rice, or grains in the case of SAD authors. Unfortunately, it is nearly impossible to get more than 10g/day of combined RS and fermentable carbs (NSP, OS, FOS, etc…). This article demonstrates my point: https://www.colorectal-cancer.ca/en/news-and-resources/cooked-cooled-starch/
I made the leap to using raw potato starch because it is well-defined as being approx 78% RS by weight, cheap, and readily available. Also because it produced the results they were looking for in the studies, often better than Hi-Maize or Type 4 man-made RS.
I wonder if lack of sufficient SCFA substrate could be the cause of things like SIBO and other gut related illnesses, even if contraindicated for ones with that condition.
We should compare notes one of these days because my calculations using the Fermentation Potential (FP) formula I created based on the glycemic index, shows that a typical Western diet contains approximately 150 grams of undigested, unabsorbed (I stopped using the word malabsorption out of respect for this audience : )) but fermentable carbohydrate. Most of those grams are resistant starch. I had to work hard to design a diet (that people would enjoy) that averaged 30 grams per day with a daily max of 45 grams.
I just posted a comment with a link that probably caused it to end up in your spam folder, could you check?
done and posted.
Norm – I’m wondering if you’ve ever heard of the term “Carbohydrate Gap” and if it’s valid? If it is valid, it may make the use of an isolated RS like potato starch or banana flour a good solution.
“Carbohydrate Gap”, as described here:
https://physrev.physiology.org/content/81/3/1031.full
“Although NSP resist digestion by intrinsic human intestinal digestive enzymes completely, their intakes do not account for calculated human SCFA production (the “carbohydrate gap”). Some of the deficit may be filled by oligosaccharides (OS), but starch and products of small intestinal starch digestion are thought to contribute the most. This fraction is termed resistant starch (RS). This review aims to examine the relative contributions of RS and NSP to SCFA production in the context of the epidemiological and other data linking complex carbohydrates to improved colon function and lowered disease risk.”
And here:
https://physrev.physiology.org/content/81/3/1031.full
“The “carbohydrate gap” is the discrepancy between NSP intakes and calculations of bacterial activity of the large bowel microflora and supports a significant contribution by RS. Individuals in affluent westernized countries may consume up to 28 g NSP/day. However, much larger quantities, possibly as much as 80 g, of fermentable carbohydrate are needed to sustain the biomass and account for SCFA production, and NSP may only provide 25% of that requirement”
“In humans, RS and OS could close the carbohydrate gap, but consumption of OS appears to be self-limiting due to osmotic effects and may contribute only 5–10 g/day.”
I’ll have to check it out.
I am amused by this conversation, much of it quite funny and would like to add my 2 cents: No two people are 100% alike of course, and certainly not in terms of the bacteria that we harbor in our guts. For some people, RS is healthy and continues to promote good health. For others, like me, if the results of eating it are bad, then I believe I can personally assume it is bad (for my system). I doubt science will ever come to a conclusion of what is exactly right for masses of people. Not possible!
For years I struggled to keep myself on a low carb diet. I even put myself into ketosis and did not lose even one ounce! Why? Fast forward to present day, and I have even gone so far as to swab the inside of my cheeks and send it off to a lab, so the lab could come back and tell me that my DNA says I need a high carbohydrate, lower fat diet to be at my best…just the opposite of the same test my friend did. Her DNA showed she needed a low carb diet, with plenty of meat and animal fat. It’s an interesting discussion – I think the answer is yes, RS is good, and no, RS is not good, and maybe RS is good. Or not! (LOL)
Funny, you may have a point, but what else would we do all day Alana – and don’t say job.
I am curious about the testing for carb requirement. I haven’t heard of this before.
Hi Norm,
OK! So did you think I would tell you all to “get a real job”???
Too funny!
The testing I did was through Inherent Health. They do DNA testing to determine what sort of dietary needs (and exercise needs) individuals have. I have met several people who have done this and I spoke with their top genetic specialist over the phone. It was really interesting to hear her talk about the differences in people in terms of their carbohydrate and fat needs, genetically speaking. So far, they have determined there are 3 possibilities: 1. Carb Reducer. These people need a low carb, higher meat/fat diet with less starch and grain. 2. Fat Reducer. That’s me. We need a lot of starches and grains with less protein and fat. 3. Better Balancer. These people do best with about equal amounts of carbs and fats in their diet, but they don’t do well with saturated fats at all. In fact, the specialist I spoke to told me these people are really damaged at the cellular level by saturated fats. For the Carb and Fat Reducers, saturated fats are not bad. This is still very “young” and of course the future holds tremendous possibilities for further exploration, but a person’s DNA can tell them quite a bit about their dietary needs.
Interesting.
Hello, I too am a good carb burner! But I have been ketogenic for the last 2 mnths and do not feel my best. I think my adrenals are suffering, but I just do not know what to eat due to sibo and ibs -c. What kind of carbs do you eat that do not cause bad things? I can not eat very many veggies at all! the usual low carb veggies are completly out except cucumber. I would like to get out of this ketosis, I do not loose weight on keto either. Thanks for your time.
Angela
Hi Angela,
That’s what the Fast Tract books are all about. The FP system makes it easy to avoid the most difficult to digest carbs (lactose, fructose, resistant starch and sugar alcohols), but still enjoy the gut friendly ones like glucose, maltose, amylopectin, etc., at least until you get SIBO under control.
@Alana Sugar – I hear you loud and clear! There never will be a ‘one-size-fits-all’ solution to modern health woes.
I find anything gut-related very interesting and think the key to our health may lie in the trillions of microbes inhabiting our intestines.
Take for instance, this passage from the article:
“Resistant starch escapes digestion and absorption yet is fermentable by the bacteria common to the large intestine, including Bifidobacterium, Clostridium, Bacteroides, Fusobacterium and Butyrivibrio.”
To the casual reader, this doesn’t say much.
Clostridium, for instance is a family responsible for C. Diff, botulism, gangrene, and tetanus. There is another species, Clostridium butyricum, that is widely used as a probiotic and one of the main ‘good guys’ in our guts. Its usefulness stems primarily from its ability to interfere with the growth of highly pathogenic C. Diff by interfering with it’s replication.
What I have read concerning RS and gut microbes is that in all cases it provides an environment which favors the growth of ‘good’ microbes and allows them to out-pace the ‘bad’. This is much more favorable than antibiotics which kill everything. Some species of microbes, though harmful in large numbers and in the wrong places, play an important role in overall health–H. Pylori for instance. People who have it totally removed are more susceptible to obesity and allergies. When allowed to grow in a suitable environment it is thought to be a ‘good’ bacteria.
Great points Tater. I agree and want to understand more as well. But it’s a rabbit whole once you enter. The complexity is immense. Genomic probe studies backed by massive amounts of DNA sequence data is already providing so much data for analysis. And, as you noted names can be misleading. Each genus has mostly good guys and a few bad guys.
Bacillus subtilis ferments soy beans to make the Japanese probiotic health food Natto, but Bacillus anthracis (which I studied in grad school) can ruin your day. C diff, C botulinum and C tetani, aside, Clostridia in general are one of the most important and metabolically versatile groups of friendly bacteria in the gut along with Bacteroides species. But Bacteriodes fragilis (studied this in post doc studies) can cause terrible infections out side of the GI tract. One of the most interesting bacteria in the gut is E. coli strains that produce these structures called pili which help them adhere to the intestinal surface creating a basis for biofilms. The same structures can pass genes back and forth even between different genera via a process called conjugation. All of the genetic studies I did with Bacteroides and E.coli were via this natural conjugation method. Very efficient and they are particularly good at transferring antibiotic resistant genes this way which is a concern. And then you have E coli 017:H7, a terrible pathogen.
Given the complexity of the microbiome, your statement ‘in all cases it provides an environment which favors the growth of ‘good’ microbes and allows them to out-pace the ‘bad’” is difficult to answer and not necessarily correct. I think the argument for limiting (not eliminating) fermentable material has more merits and clinical backing for people with SIBO – mediated digestive health conditions.
I won’t even pretend to be an expert in gut microbes!
As to the amounts of RS in the SAD, I think this is the source document:
https://www.valemaisalimentos.com.br/material/2.pdf
But this is also good and compares many diets:
https://211.76.170.15/server/APJCN/Volume19/vol19.2/Finished/18_1223_274-282.pdf
This won’t transfer well, but from second link:
“Table 3.
Resistant starch intake in different areas of the world
(g/day)
Africa 20-30
Europe 3
Ten European countries 3.2-5.7
Italy 8.5
Sweden 3.2
Global intake 3-10
America 3-8
China 14.9
Thanks for the links on RS levels in US and other countries. Looks like a good subject for a new blog piece because these levels look extremely low to me. Now when to find the time……
A topic I have been trying to tackle is the estimated amount of combined RS/OS in the ancestral diet. I believe it was quite high while the general consensus is that it was quite low.
Two food sources lead me to believe it was high: Potatoes and Plantains. I realize potatoes came later in the game, but the sophistication with which they were eaten tells me that ancient man was a bit more creative than we give him credit for.
Potato starch and plantain flour are the two highest sources of RS available today (78% and 56%), higher even than Hi-Maize at 54%.
From the book 1493 by Charles C. Mann:
““Andean Indians ate potatoes boiled, baked and mashed as people in Europe and North America do. But they also consumed them in forms still little known outside the highlands. Potatoes were boiled, peeled, choppedand dried to make papas secas; fermented for months in stagnant water to create a sticky, odoriferous toqosh; ground to pulp, soaked in a jug, and filtered to produce almidón de papa (potato starch). The most ubiquitous concoction was chuno, made by spreading potatoes outside to freeze on cold nights. As it expands the ice inside potato cell walls ruptures cel walls. The potatoes are thawed by morning sun, then frozen again the next night. Repeated freeze-thaw cycles transform the spuds into soft, juicy blobs. Farmers squeeze out the water and produce chuno: stiff styrofoam like nodules about two-thirds smaller than the original tubers. Long exposure to the sun turns them gray-black; cooked into a spicy Andean stew, they resemble gnocchi, the potato-flour dumplings favored in central Italy. Chuno can be kept for years without refrigeration, meaning that it can be stored as insurance against bad harvests. It was the food that sustained the conquering Inca armies.”
And on focus paper on plantains: https://www.musalit.org/pdf/IN020267_en.pdf
“n the African continent a hundred or more
different cultivars of Plantain grow deep in
the rainforest. In the countries bordering
the Great Lakes region in Africa, more than
sixty different cultivars of the Highland
Bananas – also called “Mutika/Lujugira”
group, can be found (INIBAP, 1995).
Cultural history and tradition point to the
presence of the crop in these areas since
time immemorial.”
Tater, Interesting research. There is not doubt, that paleolithic people consumed all versions of indigestible or poorly digestible carbohydrates. Otherwise, we would not have evolved this relationship to help us turn it into fatty acids we could burn. The question in my mind is this: If food was not easy to find, over consumption and gut reactions including SIBO would have been rare. (also note, in the pre-antibiotic era, we had a more diverse complement of gut microbes, another problem of modern living). If it did occur, a natural fast not by choice, would straighten that right out. Contact me off line if you want to compare notes on how these calculations should best be done.
And, when you get ready to write this blog piece (tomorrow?) here are a few good references:
Thesis by Dr. Li Li:
https://lib.dr.iastate.edu/cgi/viewcontent.cgi?article=2638&context=etd&sei-redir=1&referer=http%253A%252F%252Fwww.google.com%252Furl%253Fsa%253Dt%2526rct%253Dj%2526q%253Dresistant%252520starch%252520not%252520necessary%252520for%252520gut%252520health%2526source%253Dweb%2526cd%253D20%2526ved%253D0CGAQFjAJOAo%2526url%253Dhttp%25253A%25252F%25252Flib.dr.iastate.edu%25252Fcgi%25252Fviewcontent.cgi%25253Farticle%25253D2638%252526context%25253Detd%2526ei%253DgeL6UMH5JYuI0QHUnICoBQ%2526usg%253DAFQjCNH6YHMIgUpq8TCenTTyiSlqu_YVbw%2526sig2%253DLLYwwGLx0lEM5vW3WUC88A%2526bvm%253Dbv.41248874%252Cd.dmQ#search=%2522resistant%2520starch%2520not%2520necessary%2520gut%2520health%2522
Stale Maize Porridge theory: https://www.nature.com/ajg/journal/v95/n4/abs/ajg2000259a.html
A potato/banana/wheat/corn RS comparison: https://www.ncbi.nlm.nih.gov/pubmed/8695600
A banana flour/RS Ileostomy study: https://ajcn.nutrition.org/content/75/1/104.full.pdf
And finally, a study of specific gut microbes in response to prolonged RS feeds: https://www.plosone.org/article/info%253Adoi%252F10.1371%252Fjournal.pone.0015046
Happy reading!
Ha, now I see the strategy. Bury me in papers!
What’s funny is a Google search for Resistant Starch usually just turns up all the National Starch studies, a bit more inventive search terms yields much better results. Some of these I found, some were sent to me, but all worth perusing and gleaning good data.
Related to last post: In the first link (https://www.valemaisalimentos.com.br/material/2.pdf) look at the sources of RS in the SAD: Bread, cereal, snacks, chips, cookies, crackers, legumes, pasta, etc…very few paleo sources of RS, especially if one adopts low carb, then it’s almost zero.
Hi Norm:
Thought you and other readers might be interested in these two anecdotes from a couple of people giving potato starch a try:
https://freetheanimal.com/2013/05/resistant-starch-4-letter-word-nope-goal-create-mashed-potatoes-a-diabetic-can-eat-every-day.html#comment-488104
Woodwose, and then Phil Parsons immediately after, who’s incidentally a T1. Both are reporting significant positive changes.
Thanks Richard, Interesting story, though I would prefer to read about more less anecdotal, better controlled interventions. Your poster indicates he is supplementing with L-glutamine, kefir and eating whole canned anchovies, as well as intermittent fasting. When you try to change more than one thing at a time, it’s often difficult to determine what affected what. JMHO
Norm – I had an a-ha moment recently…
I was reading about a supplement put out by the Shaklee company, called Opti-Flora. It supposedly contains a pre and pro-biotic using the ‘power of RS technology’.
In reality, each serving contains 1 teaspoon (4g) of a mix of fructo-oligosaccharides and inulin. It is taken alongside a standard probiotic pill. https://hugheswholehealth.myshaklee.com/us/en/products.php?sku=80638
Studying up a bit on FOS and Inulin, I find a recurring theme that they are also fermented by bacterial species in the intestine, such as klesiella, e. coli, and many harmful Clostridium species. These are the ones responsible for unwanted hydrogen, sulfer, and CO2 production.
Everything I read about RS, it acts completely different than OS/FOS in the gut.
RS is fermented almost exclusively by bifidobacterium and the butyrate-forming species of colstridium–not the harmful species.
Could this be where the discrepancy lies? What if RS is not exactly like OS/FOS? Every argument I hear against RS is actually an argument against OS/FOS.
RS and OS/FOS are completely different when found in nature. Almost everyone who eats raw Inulin/OS/FOS gets immediate and smelly gas. This rarely if ever happens with RS. Another clue may be the modulatory effect on blood glucose regulation. RS is well-studied for it’s actions in this area, while inulin/OS/FOS don’t have this quality.
Maybe there’s your next blog topic!
Interesting idea, but many other types of bacteria other than bifidobacteria and select Clostridia can metabolize resistant starch including Bacteroides, Fusobacterium, and Butyrivibrio (Macfarlane GT, Englyst HN. Starch utilization by the human large intestinal microflora. J Appl Bacteriol. 1986 Mar;60(3):195-201.). The list is pretty extensive.
Norm – First off, let me say ‘thanks’ for entertaining us here.
I hope I can persuade you to take a look at this study and comment, because I think it says exactly what I have been saying, “RS does a better job of changing the composition of gut flora than other fermentable carbohydrates”.
https://www.nature.com/ismej/journal/v5/n2/full/ismej2010118a.html
This study used a low-carb weightloss platform to compare the differences on individual populations of gut microflora when fed either high RS, high NSP, or a low carb control diet in humans, over 10 weeks. I think this study shows that a high-fiber diet does very little in altering the composition of gut flora, while a high RS diet makes immediate changes, favoring butyrate producers, and creating an environment hostile to pathogenic species.
I will try to pick out a few statements from the study in the hopes I can get your interest:
– ‘blooms’ in specific bacterial groups occurred rapidly after a dietary change. These were rapidly reversed by the subsequent diet.
– Relatives of Ruminococcus bromii (R-ruminococci) increased in most volunteers on the RS diet
– Relatives of Eubacterium rectale increased on RS (to mean 10.1%) but decreased, along with Collinsella aerofaciens, on [low carb control] diet.
— Members of the E. rectale group are…major producers of butyrate in the large intestine, and may therefore contribute to the butyrogenic effect of RS
– In contrast to these responses to RS, there was little evidence that the high NSP diet resulted in major alterations in the composition of the faecal microbiota.
Tater, Let me say, I admire your persistence. You remind me of someone, oh ya – me. I appreciate all the links and will likely revisit some if I haven’t read them before. On changing microbe populations with diet here are a few thoughts I keep in mind:
1. Given the huge numbers of these microbes (10e9 – 10e12), percentages are less meaningful. 90 percent of a trillion is still a lot.
2. Diet absolutely modulates the types and number of microbes, even with polysaccharides that don’t appear to be metabolized immediately. Give your gut a chance and something will bloom that can eat it. – Haven’t heard of one that can break down Splenda yet.
3. The real question is what does it mean? That piece needs to be clear and well supported to make rational dieting decisions on.
4. And those recommended actions will likely look different for healthy people vs. people with dysbiosis or SIBO.
Keep up your great work!
OK, this is getting good! Maybe we need RS to act in concert with fiber in order to fully flood the large intestine with the protective SCFAs. This would make a good case for the need to supplement with a bit of RS and get lots of natural fiber from foods.
From https://jn.nutrition.org/content/129/11/2081.full
“Cummings et al…. indicated in human studies that an interaction between dietary [resistant] starch and fiber occurred in large bowel fermentation and that [RS] was fermented in preference to fiber, suggesting that [RS] might exert a sparing effect on certain dietary fibers. Also, the present study clearly showed the interactive effects of RS and [Fiber] on large bowel SCFA and suggests that it is possible to maintain relatively high butyrate concentration in the distal large bowel by dietary manipulation. The amounts of RS and [Fiber] used in the present study were conservative … 25 g RS and 7.5 g Fiber intake/d, within the range recommended for adults to consume in a healthy diet. These findings might have an important implication for large bowel physiology since there [are] strong inverse associations between the incidence of colorectal cancer and starch intake or the sum of dietary fiber and RS intake, while dietary fiber alone did not show any significant relationships. Given that fermentation in the colon is the mechanism for achieving colorectal cancer protection, via the specific contribution of n-butyrate to reduction of proliferation and induction of differentiation of the mucosal cells (Cummings 1981), it is probable that dietary manipulations which slow the fermentation rate of [RS] and dietary fiber would be of benefit in cancer protection in the distal colon and rectum. “
Interesting link on the fiber / starch combo altering fermentation location. Don’t know why they just don’t do the study in people – more relevant.
Also, the cancer protection thing is interesting, however, when I looked into this for fiber I found the evidence just wasn’t there – but that didn’t stop decades of promotion.
In this case, I would be interested in the actual evidence for this statement: “since there [are] strong inverse associations between the incidence of colorectal cancer and starch intake or the sum of dietary fiber and RS intake” and that “butyrate is responsible”
All I’m saying is that every brick in these theories need to be checked and re-checked to make sure they are sound and we’re not just wasting our time.
Agreed, Norm.
My approach basically is to have all that stuff up there, good with bad with confounders and people then decide for themselves: is this worth a try?
…Because, even the most tightly controlled intervention in the world says nothing about whether it works for you (either technically of in terms of hassle/benefit).
Of course, I’m a sh*t stitting blogger and you’re a scientist. A bit of room for both, I suppose. :)
No issue with that. Just saying I love the scientific method – trying your best to control variables. By the way, being a scientist doesn’t automatically give you the power to be right. And you know you deserve a lot more credit – look at your blog traffic! You’re reaching people through the market hype that is the internet.
Just a short PS report. I have been ketogenic for 3 years and the last two years I have seen my 12 hr FBG go from mid 80s to 105-135. My PCP thinks it is being driven by my poor sleep. I think perhaps a calcified pineal gland not making enough seratonin to be converted to melatonin may be the problem. Flouride, Bromide, Chloride, & Aluminum seem to be implicated.
For 5 days now, I have been using PS, 2 TBS in the AM and 2 TBS in the PM. Morning fasting BGG still in the 110 to 125 range.
I have talked to my PCP about using Cycloset (bromocritine) to reduce FBG and reset my circadian rhythms…the latter being an off label use. He is hesitant to prescribe because of causing problems with the pituitary gland.
I was hoping the potato starch would reduce the FBG and get me to a better sleep pattern as others have reported.
I will continue with the PS hoping for some improvement
Norm, Thanks for the work you are doing.
Dexter
Interesting Dexter. Keep us posted.
Dexter – Try this for a couple days: 4TBS of potato starch right after dinner, then no snacks until bedtime. If I do it any other way, by FBG will be 100-120, doing it exactly like I said gives me a good night’s sleep and FBG in the 79-95 range.
Mix the potato starch with a bit of plain yogurt, milk, or water. I usually eat dinner at 6 and have the PS by 7, then to bed between 10-11. Up at 6am.
Tater, Thanks.
Since ketogenic, I have always satisfied my ghrelin with two meals with no snacks.
PS it is at 7pm tonight.
I don’t know whether you’re still checking this thread, but have you considered that your elevated FBG might be physiologic insulin resistance, rather than pathologic? That has to do with palmitate causing insulin resistance in skeletal muscle to spare limited glucose for the tissues that actually need it, that can’t run well on fatty acids and ketones. At least that’s my (limited) understanding of the issue. You might try two things: a post-prandial blood sugar curve, rather than fasting, to see if that whole system is still working well, and going out of ketosis for a while to see if the FBG drops promptly down to 70s or 80s.
subscribing.
I have done a few experiments at lunch with potato starch this week.
Monday and Wednesday, my lunch was exactly the same: 1 baked potato, no skin; 1 can of sardines packed in water; 2TBS of sour cream. I checked my BG before and 1 hour after. Mon – 79 before, 135 after. Wed – 97 before, 142 after.
Tuesday and Thursday (today), my lunch was exactly the same, but I mixed 1 TBS of potato starch in with the sour cream: Tue – 96 before, 96 after. Today – 94 before, 97 after.
If anybody else has a BG monitor, I’d love to see some others play with this.
Taking a sample at only the 1 hour point maybe misses some important readings, but I think the readings speak volumes for what is going on. There is a definite change in the way the cooked starch from the potato is being absorbed. Maybe at the end of the day it doesn’t make a hoot, but I think it’s pretty cool.
Tatertot, you should start a facebook page on RS, you can share articles, posts, research, etc. I’d subscribe in an instant.
No thanks! My wife already says I spend too much time on the computer…
Here’s a good article from yesterday’s NYT: https://mobile.nytimes.com/2013/05/19/magazine/say-hello-to-the-100-trillion-bacteria-that-make-up-your-microbiome.html
“His comment chimed with something a gastroenterologist at the University of Pittsburgh told me. “The big problem with the Western diet,” Stephen O’Keefe said, “is that it doesn’t feed the gut, only the upper G I. All the food has been processed to be readily absorbed, leaving nothing for the lower G I. But it turns out that one of the keys to health is fermentation in the large intestine.” And the key to feeding the fermentation in the large intestine is giving it lots of plants with their various types of fiber, including resistant starch (found in bananas, oats, beans); soluble fiber (in onions and other root vegetables, nuts); and insoluble fiber (in whole grains, especially bran, and avocados).”
Found a really neat website: https://humanfoodproject.com
For $99 they will map out your gut microflora. I wish i would have done it prior to my RS experiment. I did a search for ‘resistant starch’ on this site and found this in the comments:
“Norm Robillard / 25 July 2012
Excellent idea and informative article. As a microbiologist, I was thrilled that someone wanted to know what we think (next time include me please!). Just one word of caution regarding question 5. To much fiber and resistant starch, while it may be great for the microbiome, can drive acid reflux and IBS symptoms in many people susceptible to small intestinal bacterial overgrowth. ”
Glad to see you are still saying the same thing!
I try to be consistent once in a while.
Norm:
Question. Here’s the preface. I think I already mentioned that my dad and 3 younger brothers are lifelong GERD people. Way back in the 90s I always knew that Atkins fixed that. I was young then, too (20s). FF to early 200s and Im getting fatter, GERD all the time, so years on PPIs, which work. 2007, go LC Paleo, pretty strict, and also IF twice per week. GERD knocked dead without the meds. IFed 1-2 times per week for a good long time and even at times being less paleo than optimal when not fasting, had lots of headroom.
Anyway, last few months a lot of GERD even though tightening up the diet, I always used baking soda in water to kill it.
So, potentially some SIBO. But here’s the rub. Last couple of weeks if been going back to two 24-30 hour fasts per week and Only after two full sessions, I’m feeling like the GERD is getting under control again.
So, question is, does fasting have a favorable effect on stabilizing and rebalancing the gut?
Hi Richard,
Sounds like your good observations over the years helped you build a bit of a tool kit to manage your GERD symptoms. But as we age many of us need to tighten things up a bit more. We may have a bit less stomach acid (made much worse by PPIs) and our immune system may not be quite as sharp either. LC, paleo, FODMAP approach and others are positive approaches. In Fast Tract Digestion Heartburn I discuss these diets and compare them to the Fast Tract program that I feel has several advantages.
But to your question, yes intermittent fasting is helpful for several reasons. To start with, if you have reflux, you have some level of gas producing bacterial overgrowth. There is no question in my mind and I present the evidence in my book. Fasting removes the microbial fuel better than any diet. The purpose is not to punish the bacteria in the large intestine (they will be fine. Just compare a fast to taking antibiotics. No comparison which is the gut wrecker), but to give your body’s protective mechanisms time to catch up. You have stomach acid and bile to inhibit bacteria in the upper intestine, motility to keep things moving, a multilayered immune system to restore order from chaos, and normally efficient systems to remove the digestible material so the bugs are not overfed – think of putting out too much bird food in your back yard. Eventually you get squirrels and even rats. And lastly, when you have symptoms, lay off the resistant starch for a bit as well : ).
Dr Robillard,
I have acid reflux for 5 years, SIBO since last year. Since I lost a lot of weight using low carb diet to reduce my SIBO symptoms. I defintely need more carb. I searched and bought both of your Fast Tract Digestion books. They are so helpful for me. I started to eat Jasmine rice which does not bother my digestion system. I am very grateful. My only question is since I was diagnosed as prediabetic. How much (times and portion size) rice should I eat every day to be safe. My other foods are mainly meats and some vegetables. I only eat freshly cooked rice.
Could you give some advices.
Hi Dahjens,
I’m happy you liked the books. Thanks.
You likely read my comments on diabetes and SIBO diets. If you are prediabetic, I would recommendation that you significantly limit your overall carbohydrate intake to limit your blood sugar. That is the healthiest practice for pre and actual diabetes. That’s what my first book, Heartburn Cured focuses on. There is no truly “safe” amount in this case. However, having a 1/2 cup serving with dinner will certainly keep you well under the 120 g carbs per day that the ADA recommends, last I checked.
Four days now on 4TBS of PS mixed in water 1 hour after dinner. Results on FBG 103, 92, 108, 130. Not much different than pre PS. Very gassy the first day and then almost none since then.
Sleep has not improved but it has been poor for over 6-7 years. Am 70 years old and feel well with no aches or pains but I know my poor sleep is slowly shortening my telemeres. I could be functioning much better with better sleep.
It is maddening to one day see my FBG down into the 90s and then soar to mid 130s and everywhere inbetween the next and I have absolutely no idea why. And my PCP has no idea why either…except he thinks that poor sleep is driving my insulin resistance. My insulin resistance score on labs is always 6 or 7 and Quest says it should be less than 45.
When I fast for 24 to 30 hours I get my FBG to the low 90s but no lower.
I have read a little on NEFAs…Non-Esterified Fatty Acids….being implicated in pre diabetics but I get lost reading some of the data and just don’t understand.
One last thing…prior to PS, I was probably operating my body on ketones for fuel most of the time. Do ketones in older people play any role in diabetes? I think not but I thought I would ask.
Thanks to everyone. I know the road to optimal always goes through the gut…I wish I could figure out mine!
Dexter -consider parasites and liver flushing for blood glucose.
Thanks ilise, Twice a week I take Diatomateous Earth food grade to be sure I have no resident parasites.
As far as my liver goes, my GFR…liver function…is around 72. Quest says that number needs to be over 60. But I will take your suggestion.
What is the FP for chestnut flour? Is this ok to use?
I would say avoid or minimize this flour if you have any symptoms. Even though they have not been tested for glycemic index, they are high carb and based on peanuts (similar food that has been tested), you would want to estimate the GI around 20 to 30 that would give you a relatively high FP. Of course you can always experiment in a controlled fashion once symptoms are under control.
Do you know where arborio rice falls on the FP spectrum?
Hi Kate,
Arborio risotto rice is a higher FP starch (17 to 18 grams for a 5.3 ounce serving).
https://freetheanimal.com/2013/06/resistant-starch-now-were-getting-somewhere-and-talking-shit-too.html
New post on RS if anyone’s interested!
It’s a long time since I have seen in an article such a lack of bias and friendly, open handling of all points of view, studies and opinions. Like a breath of fresh air. Thank you.
Thanks Anthony. Glad you liked it!
Thank You Norm; great article and open discussion!
Thanks Mike!
Bacteria, bacteria, bacteria. What about fungi?
https://articles.latimes.com/2012/jun/08/science/la-sci-sn-fungus-irritable-bowel-20120608
Testing done by American Gut does not include fungi while Metametrix testing, both stool and urine, barely scratch the surface.
Has anyone considered resistant starch as antibiofilm? I’ve been wondering how fungi would react to RS in SIFO. Apparently, fungi would produce amylase as would some bacteria. Amylase busts biofilm. But would RS feed fungi? Or would amylase production be enough to keep populations in check?
https://link.springer.com/article/10.1007%2Fs12010-011-9526-2
https://benthamscience.com/open/openaccess.php?tomicroj/articles/V005/21TOMICROJ.htm
https://www.hindawi.com/journals/bmri/2013/150653/
https://synapse.koreamed.org/Synapse/Data/PDFData/0184MB/mb-34-128.pdf
https://pelagiaresearchlibrary.com/european-journal-of-experimental-biology/vol3-iss4/EJEB-2013-3-4-26-34.pdf
Fungi also produce lactic acid and ethanol from potato starch:
https://digital.library.adelaide.edu.au/dspace/handle/2440/47204
https://aem.asm.org/content/52/5/1055.full.pdf
https://link.springer.com/article/10.1007/s00449-005-0398-0#page-1
So, the basic hypothesis is that RS may be forcing microbes to produce enzymes, acids and alcohols which serve to clean up shop in the small intestine, right where they live in their slimy biofilm matrix communities. Of course, you can also take amylase supplement (also thought to degrade histamine), but the results may not be as well-targeted as with RS.
Yes, I wonder about fungi as well. After seeing Paul Stamets TED Talk a few years ago, and reading Colin Tudge on “The Secret Life of Trees”, it became apparent to me that fungi (who were here first) have insinuated themselves everywhere and are likely essential intermediaries between the food we eat and some of the nutrients we require.
I also wonder about viruses – Frank Ryan in his book “Virolution” suggests that many of the viruses that humans carry are not pathogens, but in fact symbiotic, even mixing with our RNA/DNA from time to time.
Then, in “An Epidemic of Absence”, Moises Velasquez-Manoff explores the idea that, actually, pathogens and parasites might be the evolutionary heritage of us all and excluding them with modern hygiene, sanitation and medicine exposes us to disregulated immune responses.
So, RS, fermented foods and SBO’s for healthy gut bacteria – bring it on – it makes intuitive sense, but what should we do to cultivate a healthy fungal, viral and parasite load?
https://www.ted.com/talks/paul_stamets_on_6_ways_mushrooms_can_save_the_world
https://www.amazon.com/Secret-Life-Trees-Penguin-Science/dp/0141012935
https://www.amazon.com/Virolution-Frank-Ryan/dp/0007315120
https://www.goodreads.com/book/show/13259821-an-epidemic-of-absence
Wow what a lot of comments.
Here’s a theory
Modern world = abundant food. Industrialization allows for year round starch consumption. That’s a relatively new deal historically speaking. I mean times were northern populations would have to endure low starch seasons no? So these sibo bacteria would have endured seasonal die off by virtue of winter. There’s a lot more going on here but start with that.
Also, I had an another theory/question
People have been told to reduce salt intake (the people saying this don’t have a compelling reason IMO). But we also know that salt isn’t just sodium but chloride which is needed for hcl. Could sibo result from chloride deficiency?
Interesting idea William. There was definitely a seasonality to starches that we have eliminated by shipping goods and improving storage techniques. But the idea that we introduced many more starches with the advent of farming grains (10K years ago) may be the most significant overall change.
I don’t have an answer to your second question, but let me know if you dig up some evidence for this.
This is SUCH a fascinating discussion. I have been trying to heal my family with food for a very long time, and lately, after nearly 4 years using a GAPS-type protocol (with very little fruit/nuts, and large amounts of many veggies, meats, fats, broths, etc.) I am venturing into the RS territory. :)
I am absolutely sure that my son (now ten) could never have handled this when he was younger – his gut was in really, really bad shape. I am so interested in the possibility of changing our internal “terrain,” especially after a period of time spent “starving” the microbial overgrowth. At least that’s part of the theory behind what we’ve been doing…
Anyhow, it’s also fascinating: the ways the a healing diet for people who are getting well after significant illness is likely to need to be a lot more careful/targeted than a “healthy” diet eaten by a generally strong individual. It’s interesting to me how so many people have suggested ideas to me over the years that were just not possible for my son to tolerate. And I often wondered: are these folks healthy _because_ of a certain aspect of their diets (say raw veganism), or _in spite_ of them?
I wonder a lot of things. What are the best carbohydrates to re-introduce after an extended period of time spent not eating them?
What are the differences between children’s and adults’ guts?
If stinky farts are the result of protein-fermenting bacteria, then what the heck does that mean one should do about it? (Sorry, I haven’t read your book yet, Norm – I only just found your site!) I have added in RS in the form of potato starch, and additional carbs in the form of sweet potato. Could it be the fructose in the latter?
What could cause this horrible symptom experienced by some in our family, otherwise known as an Intensely Itchy Butthole (only we call it IAH)?
My daughter had terrible reflux as an infant (she’s now 18 months), and I have been struggling to manage it with diet for many many months now. She seems to be doing great with sweet potato, and more carbohydrates in general, which I added in about a month ago. This is interesting to me. We never used the drugs for her reflux, because it made no sense to turn OFF her stomach acid production! But it also didn’t make much sense to me why she had it in the first place, even when she was drinking exclusively breastmilk (I had to pump for a year because she had severe feeding issues that prevented her from nursing normally. But that’s another long story). She seems to be allergic to dairy and/or eggs (severe skin rash which goes away when we stop feeding her these things, and I’m too tired to try to figure out which triggers the allergy!)
Anyway…I should stop typing now, but I really appreciated this post and the subsequent thoughtful, fascinating comments.
Regards,
Sarabeth
Hi Sarabeth,
Good you are interested in diet over drugs to address GI issues in your family. I would recommend Fast Tract Digestion IBS for a bit more general GI focus, but Fast Tract Digestion Heartburn if your daughter’s reflux returns. Sorry, I can’t be much help for IAH.
Subscribing. Never thought I had SIBO until I tried supplementing with potato starch and tapioca starch, which cause a lot of upper GI distress even in small doses.
Hi Annika,
I know you’re not alone. Most starches (except those low in fermentation potential) trigger my own heartburn symptoms after a few days. But there are some saying the opposite is true – RS, particularly RUMPS (raw unmodified potato starch) “carries away” bacteria (especially “bad bacteria”) from the small intestine like a bus going down the freeway. My concern is that bacteria are sticking to starch for one reason (TO EAT IT!). Someone with SIBO involving any of the many types of bacteria that degrade starch may have a problem, especially if they happen to have a motility issue -imagine the picnic lunch spoiling on the bus because it’s stuck in traffic.
My real goal is helping people with SIBO and dysbiosis, not being right about RS. So I plan on keeping an open mind about potato starch as we learn more. Also, I like Tim Steele and Richard Nikoley and respect their effort to raise awareness about RS. I just want to see clear evidence that this approach will help, not hurt people like you and me.
ps: Wonderful website!
Thanks for replying, Norm! I have been actively (obsessively?) following the goings-on over at Free the Animal for the past several weeks. I started experimenting with potato starch and did 4 trials, eventually reducing my dose from 1 TBS down to only 1/2 tsp. I then switched to tapioca starch. Each time I tried, I would feel fine for the first 2 or 3 days, then I would start to get bad dyspepsia and heartburn. I would then stop the starch, and the symptoms would persist for another few days.
I have read a lot over at Dr. BG’s site, AnimalPharm, as well as at Free the Animal, and I think I must have low-grade SIBO that normally doesn’t cause noticeable symptoms, but when fed with resistant starch, results in a bacteria orgy in my small intestine. Usually my GI system is pretty much fine, so I never considered that SIBO might be an issue for me. Food sources of starch has never seemed to bother me.
I’m going to follow Dr. BG’s advice and increase my intake of fermented foods and start taking SBO probiotics. I’d really like to be able to supplement with RS because people have been so enthusiastic about their results. I’m especially interested in getting my high LDL and fasting blood sugar down.
Good luck Annika. Let us know how you make out.
Norm:
You are a refreshingly honest man.
Annika came over from FTA because my “damn the torpedoes” approach didn’t work for her.
I think Tim shot her the link.
Anyway, I’m not going to but in, only wanted to acknowledge you back and assure that when someone falls out of what we’re normally seeing, it’s off to Grace and Norm.
Thanks Richard, You know your always welcome over here.
Norm.. curious if you have tried or considered the cabbage juice cure for GERD? Ive been researching it for few days now and have come across quite a few personal experiences from people who cleared GERD with daily regimine of cabbage juice for a number of days/weeks.
I dont have GERD but bloating and have been on cabbage juice for three days now. Can say that I feel it helps much and am hoping for further results as I continue. From what I understand cabbage juice can kill off unwanted bacteria.
Also would like to add… when I say “cleared GERD” I meant cure. After taking the cabbage juice the GERD did not reoccure and in the cases I did read that it came back after months or years they were able to use the cabbage juice once again and be rid of all symptoms.
Hi ing,
Never heard of it before – interesting. Cabbage is a low FP veggie, so it shouldn’t hurt to try. If you find more info, please share.
I havent been documenting my sources but here is one study..
https://www.researchgate.net/publication/51641463_Inhibition_of_growth_of_highly_resistant_bacterial_and_fungal_pathogens_by_a_natural_product
Inhibition of growth of highly resistant bacterial and fungal pathogens by a natural product.
ABSTRACT The continuous escalation of resistant bacteria against a wide range of antibiotics necessitates discovering novel unconventional sources of antibiotics. B. oleracea L (red cabbage) is health-promoting food with proven anticancer and anti-inflammatory activities. However, it has not been researched adequately for its antimicrobial activity on potential resistant pathogens. The methanol crude extract of B. oleracea L. was investigated for a possible anti-microbial activity. The screening method was conducted using disc diffusion assay against 22 pathogenic bacteria and fungi. It was followed by evaluation of the minimum inhibitory concentration (MIC). Moreover, the antibacterial and the antifungal activities were confirmed using the minimum bactericidal concentration (MBC) and the minimum fungicidal concentration (MFC), respectively. Remarkable, antibacterial activity was evident particularly against highly infectious microorganisms such as Methicillin-resistant Staphylococcus aureus, Escherichia coli O157:H7, Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus, and Salmonella enterica serovar Typhimurium as well as against human fungal pathogens, Trichophyton rubrum and Aspergillus terreus. Red cabbage is a rich source of phenolic compounds, anthocyanins being the most abundant class, which might explain its potent antimicrobial action. This extract is potentially novel for future antimicrobials, inexpensive, and readily available at a large scale for pharmaceutical companies for further investigation and processing.
Also forgot to mention that I have symptoms of fungal rash that are much less after taking cabbage juice. (raw potato juice has worked as well by the way). I have taken natural antifungals and when they work they usually cause me mild headaches before seeing results..the cabbage juice when taken on an empty stomach also causes these type of headaches. I am not prone to headaches so I know when an antifungal is working based on this alone.
Thanks for the info. Will have to check it out tonight. Interestingly, I saw this article on “fermented” cabbage. https://dailym.ai/1lrZsNe
New wonder drug?
I have experiemented multiple times with cultured sauerkraut (both organic homemade and raw organic brands) and did not find any results for either skin or digestive issues. I feel that the juice works on another plane other than providing good bacteria like fermented products. I have also tried over 50 probiotic supplements also to no avail. I assume I must have overgrowth of bacteria preventing these beneficial bacteria from implanting. The cabbage juice makes for very normal stools and digestion for me personally. I hope that my main concern -bloat- will be able to be resolved with the juice however after ten years of trying various methods I am not holding my breath. I am however optimistic because results are clearly visible.
Right, I would guess the cabbage juice would be more of a weak prebiotic whereas the fermented cabbage is a probiotic. Let us know if the bloating goes away while taking the cabbage juice.
Can u share more about when u drink this, how much, and other details?
Is it just red cabbage?
So it helps with Sibo, gerd, reflux, and gastritis?
Hi Beek,
I juice one medium sized head of green cabbage everyday which yeilds me around 10 ounces of juice. I find better results if I drink on an empty stomach and wait a few hours before drinking or eating. I believe studies indicated more ounces spaced throughout the day but I have found many personal testimonies stating around 7-10 ounces per day worked just as well.
Yes I have read that it worked for GERD, reflux, gastritis and peptic ulcers.
From what I have gathered there is not a concensus from the medical research on exactly how cabbage juice works for treating these ailments.
I plan to try red cabbage next week. One more thing I notice is that I no longer require my usual calcium supplement to relieve me of deficiency symptoms.
I had a look at the paper Ing. Antibacterial substances from cabbage is an interesting idea as is the tried and true general approach of identifying antibiotics from fungi, bacteria and other marine and land plants. Some of the these sources have resulted in spectacular finds, such as the streptomycin used in the study as a positive control. Of course you always want to know what the potency is. In this case it’s pretty low – about 1600 to 4000 times less than streptomycin based on the data on S. aureus. I wasn’t clear after reading the methods section what the yield was – how much active substance they get from what volume of cabbage, but clearly, you would need to consume quite a bit to get meaningful antimicrobial activity. Another issue arises when you do get meaningful activity – what healthy bacteria are being killed and how does that affect the diversity of my entire gut microbiota. It’s this last point that leads me to favor diet over antibiotics in general for controlling excessive gut microbe growth. But you never know. If it works for you what can I say?
https://ncsu.edu/foodscience/USDAARS/Acrobatpubs/P254-286/P264.pdf
https://www.ncsu.edu/foodscience/USDAARS/Acrobatpubs/P221-253/p247.pdf
Cabbage juice has a high success rate in studies for healing stomach ulcers which are also believed to have bacterial component.
Interesting studies on inhibitory compounds from cabbage Ing, especially the MIC results for MMTSO and AITC. Do you happen to have a reference for “high success rate in studies for healing stomach ulcers”? Thanks!
Fermented cabbage juice made my reflux (I have the silent type, probably LPR) explode in fury, also gave me serious heartburn, and a very sour stomach. In fact, my desperate attempts to recover from it is what led me to this site. Waiting now impatiently for my copy of Fast Track Digestion (Heartburn version) to arrive……
Hi there Susan Coe. I am curious as to how you are responding to the FT diet. I also suspect I have LPR and i have been trialling the diet for about a month, in conjunction with apple cider vinegar before meals. Over the last few days my reflux has really kicked back in. I have been eating sauerkraut, so maybe this is this is the trigger??
Curious as to why my links to studies were deleted? I came back to the site to retrieve them for my personal reference and they are now gone.
Is it possible you posted the links on the forum under the same name as this article? I suspect that is the case ing.
Weird, I now see my links and previous post that I thought was missing.
———–
Here are some studies that I know of for peptic ulcer/cabbage juice
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1643665/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1532869/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1521464/
I have chronic klebsiella pneumoniae, as well as Sibo…. Klebsiella is a starch eating bacteria that is linked to numerous autoimmune issues like ibd and alkalosing spondylosis.
Would rs be beneficial, or would it make the Klebsiella flare due to its love of starch?
I want to heal my gut and it’s felt like a losing battle for years…. Nothing seems to help.
Idk if rs would help or not… Any thoughts?
Hi Beek,
I would think that adding RS to your diet would be the last thing you would want to do. I recommend reading a recent review by Dr. Alan Ebringer on the subject. From there you can access the full body of his work on the topic if you haven’t read about his work before.
https://www.hindawi.com/journals/jir/2013/872632/
Eventually, I will release a volume of Fast Tract Digestion for autoimmune disease that will include AS, Crohns, Celiac and other AI conditions. But you could just try the diet following FTD IBS. The basic diet won’t be different.
Thanks so much for the quick reply. It’s hard to know what to do with so much conflicting info. It’s a fine line between starving the bad and feeding the good and vicr versa
I’m basically following an autoimmune paleo diet coupled with low fodmaps/no fruit/low histamine /low oxalate/anticandida lol
I also wanted to get your opinion on oxalates. It’s also been making buzz about how it is linked to autoimmune issues, pain, inflammation, leaky gut, etc. Doing a low oxalate diet is recommended…. What are your thoughts on this? Susan Owens is the lead researcher on this and has some really compelling insight. However, there are other whom debunk this and say it’s not necessary and cuts out beneficial foods. But it also seems that the healthier people try to eat, the sicker they get, which is usually when they start doing tons of juicing, smoothies, nuts, seeds, tubers,…. All high ox foods.
Anyways, if u have any thoughts on this stuff, I’d love to hear it. Oxalate issues are linked to a deficicncy in a strain of bacteria called oxalbacter (i killed the spelling, sorry), which helps degrade ox
Thanks for the article on klebsiella…. So Rs would be pretty bad, eh? What macronutrient ratio would be best for me? I suffer from bad constipation too
One thing that caught my eye was the talk on collagen in the article. I had recently tried great Lakes grassfed collagen and noticed it made my joints very sore and also caused symptoms of air hunger and Sob, and tachycardia. Here is the paraphragh I’m referring to from the link u gave me:
The types of cross-reactive antibodies produced following Klebsiella infections will determine the anatomical location of the pathological lesions, especially in AS. Some antibodies are reacting with HLA-B27, an antigen which is expressed in most articular tissues inside the synovial joints, whilst other antibodies are reacting with types I, III, and IV of collagen, which form an important component of the spinal tissues where the pathological lesions are located. The binding of these Klebsiella cross-reactive antibodies, when present in high titres, triggers inflammatory cascades such as the complement system together with the production of various cytokines resulting in the pathological changes with consequent fibrosis, calcification, and new bone formation leading to the development of classical AS. Moreover, the raised level of HLA-B27 antigen expressions on the targeted tissues in patients with AS [68] will make these molecules more accessible and hence will increase the chance of their binding to anti-Klebsiella cross-reactive antibodies.”
Does this mean that klebsiella also reacts with collagen supplements? I’m a bit confused. I was hoping taking collagen would help my joints and pain, not inflame it
Thanks so much for the help… Am I “doomed” to follow a low carb diet for life? And do I also need to avoid the nonfermentable carbs listed in your Bok as to not feed the klebsiella? (I don’t eat them atm, but I do eat Butternut squash in small amounts)
Sorry for the length of my posts…. Its hard to find an expert so keen on gut and flora such as yourself!
Beek,
Don’t know that much about oxylates. There seems to be a wealth of blog articles on the topic, but considerably less in the scientific literature which tends to make me uneasy on any topic. Please feel free to post any papers you have found on the topic.
As for autoimmune responses, based on Klebsiella molecular mimicry, to collagen supplements, it would theoretically be possible if the collagen in the supplements had the same binding domains as structural collagen. Theoretically, it might be possible for collagen supplements to exacerbate that reaction as well, but I am not sure this really happens. I just don’t know.
Beek,
I would recommend cabbage juice for Klebsiella pneumoniae, I have read of fasting plus cabbage juice to rid various gut infections. Here is study with red cabbage
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3171003/
” Remarkable, antibacterial activity was evident particularly against highly infectious microorganisms such as Methicillin-resistant Staphylococcus aureus, Escherichia coli O157:H7, Pseudomonas aeruginosa, Klebsiella pneumoniae, Staphylococcus aureus, and Salmonella enterica serovar.”
Please define “easier to digest” when you use that phrase. “Digests more immediately” when reaching the first part of the gut? “Digests more slowly, not in the first part of the gut”? And doesn’t “easier to digest” depend not only in which part of the gut this digesting is happening, but also on whether the person’s bacteria in that part of the gut is correct?
Easier to digest? Meaning…
Hi Mary,
Your first statement is more indicative of what I mean. “Digests more immediately when reaching the first part of the gut” meaning the proximal end of the small intestine. And I am only talking about human digestion and absorption. I am interested in knowing the amount of fermentable material that persists beyond the early part of the small intestine where bacterial counts begin to increase, particularly in the case of SIBO. The reason I use the term “fermentation potential” is to describe carbs that have the “potential” to be fermented. That doesn’t mean all of them “will” be fermented.
Thank you Norm for your IBS book. It made sense to me as I had already put several of the pieces together through others work. I started with GAPS, to full blown IBS-D for many years, to SCD, to FODMAPS & FTD. From each of them I learned another piece about what was taking place in my gut/and what wasn’t taking place in my gut that should have been. Do you or anyone know what affect lactofermenting the rice and vegs starch, the fructose in fruits and (prefermenting) the fiber in vegs and fruit or nuts has on the FTD foods FP wise? Am eating meat and fat and have lost too much because of the D. I need the next puzzle piece to transition and have been thinking about the lactofermentation that I do in an airlocked vessel. (I had formerly done open/wild fermentation for a while before the IBS-D kicked in.) So if SIBO & FTD is about limiting fermenting potential, how about beating it to the punch/prefermenting before eatting and getting more foods back in my diet? Was thinking of leaving the food matter and drinking the juice but after reading scads more conversations, I believe I would do better on limiting the potent good bacteria and begin consuming the plant matter, not so potent. I am interested in it’s workability. Anyone? Also, I read in FTD FP chart that buckwheat is 50GI but in pancakes is 102GI. Why? Thanks.
Good thoughts Mormor. I have been doing lacto-fermentation myself this summer. I agree, wild fermentation is asking for trouble. I also use a modified mason jar cover with a fermentation lock. I have made enough beer and wine over the years, to appreciate the importance of keeping the process completely anaerobic. Oxygen is the enemy. I also avoid opening the ferment until it’s done to avoid letting air in.
You are correct suggesting that fermentable carbs can be removed / reduced via fermentaion. Letting the fermentation proceed to completely is the key. I am currently fermenting pickles and cauliflower with garlic and other herbs. I have not fermented starches including rice, but there are recipes for fermenting just about anything. And you will end up with much less fermentation potential. Good luck and keep us informed about your experience and lessons.
hello everyone,
what this article is saying about RS is completely true. and believe me i just got big relief from the helpful knowledge in this article, which has helped me understand more of my problems. to make it shot: when i realized i had gut issues i started eating clean. i cut out all PROCESSED FOODS AND SUGARS. And immediately i felt like i was experiencing the best feelings and moments of my life. Then few months later I could not digest corn, potatoes, basmati rice which i had been digesting when i started eating clean. then i became most confused ever as to how on earth i digested these foods when i was eating unhealthy and now am eating healthy i couldn’t. then i left those foods including all carbs and all my problems including brain fog, unclear sight, fermentation, bloating, constipation- just to mention few- went away. for five months now whenever i ate my stomach is just flat in minutes, with a clear head, sight and breathing. but guess what brought me to this sight? i just ate basmati rice and bloating, stinky gas and brain fog came as a result and i had to locate this site by luck- almost like God sent. now i understand why i ate some starch and no bloating , brain fog or whatever; and i ate others and there was bloating, brain fog, etc. its because of this RS theory. this article is correct. IF YOU HAVE SIBO RS IS YOUR WORST ENMEY
Hi Alvin, I got on this page for the same problem… I’d really love to speak to you, please answer here if you read my message…
Hi Norm…its all been a very interesting read. I was hoping you can advise me with my uncommon problem, well at least I think its uncommon. I have been dealing with my candida for many years now, I have been Paleo for over 16 months, I obviously leave the fruit out completely, along with the nuts and seeds and all tubers. I have taken every anti fungal out there, and I follow the diet religiously, then once a year I re-test with a stool sample to be told I still have Candida!! During these 6/7 years I’m always trying to re-populate my gut with the beneficial bacteria. I have tried numerous brands including, 11 Strain, Prescript-Assist and Probiotic-3 and all that seems to happen is they cause my skin to react as in the same way it does when I used to eat the problematic foods IE sugars, carbs, nuts and seeds to mention a few. It looks like a major case of thrush all between my legs, so I cease taking the probiotics and within a couple of days its all cleared up, and its not sore or irritable. This happens with homemade Kefir (made with coconut milk) sauerkraut and other fermented foods! This is most annoying as I know I need to populate my gut as to stand a chance of winning my battle with Candida, even the stool analysis results always indicate zero beneficial bacteria levels. Have you come across this problem before? if so what am I to do about it? Any advice you give I will be most grateful for…thanks.
Hi there,
I have both fructose malabsortion and lactose intolerant. Also have hemorrhoids. Just wondering, if it would be beneficial to take water kefir?
Many thanks
Hi T,
I haven’t made this myself, but commercial kefir (3 1/2 ounce serving) I looked had 5 grams of sugar and 1 grams of fiber. The FP would be about 3 grams. Not too bad.
This is such a good post, I have come back to it many times, as layers of symptoms and understanding unfold. In your book, you mention the need to have pasta, for instance…hot, not cold…or it is a source of fermentation carbs. Would the same hold true for potatoes and especially oatmeal???
Thanks so much!!
Susan
Thanks Susan. Absolutely, consume these foods well heated (but not overcooked). Thanks for adding this clarification.
Thanks so much, Norm…but now YOU raise another question: When you say, ‘but not overcooked’…I am guessing that is important because overcooking would bring out even more starch? Or just because it would diminish the quality of the food?
thanks again!! Best,
Susan
Yes, overcooking can increase resistant starch. It gets a little complicated (not sure I fully understand all the details). I can reach out to Tatertot AKA Tim Steele if you are really curious. In the interim, here’s a link to a good paper. https://onlinelibrary.wiley.com/doi/10.1111/j.1541-4337.2006.tb00076.x/pdf. Search Linearization of amylopectin. Also see the next section on “heat and moisture”. My recommendation is to use some caution about overheating. For instance with fried rice, you might limit the amount of time and heat when you add the rice to the pan. Avoid repeated heat / moisture treatment also.
Still subscribed to this thread!
The subject of RS creation during cooking is made easy when you think of it in terms of ‘staling.’
To increase RS in bread, let it get stale. To increase RS in rice or potatoes, overcook in a dry manner.
So, to best prepare foods with little formation of RS, think fresh, hot mashed potatoes or rice right out of the rice cooker. The more moisture in the finished product, the less chance of excess RS.
I had an a-ha moment the other day in the question, ‘Does RS feed pathogens?’
I made some potato starch using my Jack Lalanne Power Juicer. It was not fully dried when it went into a storage container. The next day, I opened the container to get a scoop for my smoothie, and it looked like bleu cheese! Completely speckled with mold throughout. So, obviously this stuff is not anti-fungal.
Potato juice, however, as found in a whole potato, does seem to have anti-fungal properties. It must, eh? To protect the potato for 6-8 months or longer until the next growing season?
So, when eating RUMPS, and a yeast (or bacterial) overgrowth is in play, I believe you would be fueling this overgrowth substantially.
However, in the non-SIBO/SIFO, immunocompetent person, RUMPS should pose no problem.
To recommend RUMPS to every person equally is as wrong as saying it is harmful to every person.
Nearly everything we eat is also food for yeast and fungi. What food can you spritz with water that will not become moldy soon?
I can think of a few: Fresh, intact fruits, vegetables, and mushrooms. However, given enough time and moisture, these, too, will get moldy.
Is there a lesson there for people with significant overgrowths? Would eating otherwise ‘off-limits’ foods with a generous portion of an anti-fungal food limit the fermentation potential? Say, garlic, for instance? Or some carrot juice? Or a big serving of any fresh veggies?
Cheers!
Tim
Hey Tim,
I seem to recall a conversation we had about excess heating/cooking leading to an increase in RS. I remember thinking, it might be best not to over cook fried rice. Do you recall the process that results in increased RS when cooking at higher heats, baking, frying etc.?
Tim,
Here is another question. There is lots in the literature about how fats interact with amylose to form a complex resistant to digestion. But what about amylopectin interaction with fats? Could the GI lowering affects of fats be dependent on amylose. In other words, perhaps fats don’t affect high amylopectin carbs as much. I seem to recall a paper addressing this point.
It is all strictly a matter of drying, which allows a crystal pattern to begin forming in the starch granule structures. Overcooking fried rice, ie. cooking until some of the rice is crispy, would result in the formation of more RS.
As to the second question, it gets a bit more complex! From a
“The enzyme hydrolysis of the starch is affected by the extrinsic and intrinsic factors of starch. The presence of protein matrix and cell wall material surrounding starch granules can prevent the accessibility of enzyme to hydrolyze the starch. The susceptibility of the starch granules are also greatly ffected by their amylose content, starch polymorphism, structure of amylopectin, and the presence of amylose-lipid complex in the starch granules. Amylose negatively correlates with the
susceptibility of starch to amylase hydrolysis because it intertwines with amylopectin, and holds the integrity of the starch granules. Amylopectin of the A-type starch has larger
proportions of short branch-chains, which result in more open space (weak points) in the granule for amylase to penetrate and hydrolyze the starch. Thus, the A-type polymorphic starch is more digestible than the B- and C-type polymorphic starches.”
From the same thesis:
“A novel technology to produce starch with high enzyme resistance was developed by introducing amylose-lipid complex to high-amylose maize starch VII (HA7). HA7, a B-type
polymorphic starch with amylose content of about 70%, contained 42% resistant starch (RS) determined using AOAC Method 991.43 for dietary fiber. The RS content of the HA7
increased up to 75% when the HA7 starch was complexed with fatty acid (FA). Pre-swelling and debranching of the HA7 starch granules was used to enhance the amylose-lipid complex
formation. The greatest RS content (75%) was produced when the HA7 starch was heated at 80°C, debranched with isoamylase (ISO), and complexed with stearic acid (SA).”
So, you can see, food scientists are looking at ways to make RS more resistant, too, and using fat as a way to prevent enzyme degradation.
In a real-world eating situation, what I think this all implies: retrograded amylose is able to withstand heating more than retragraded amylopectin. And amylose retrogrades faster than amylopectin.
For those looking to INCREASE RS, this just means cook and cool your starches and eat cold or minimally reheated for maximum RS content.
For those looking to decrease RS, it would mean choosing foods higher in amylopectin and eating them freshly cooked and still warm, and not using leftovers.
As to using fat to manipulate the RS content…not sure how it would work with eating real foods. Fat does effect the enzyme degradation of starch, fat added to starchy meals lowers the GI, so presumably increases FP.
So, probably eating freshly cooked rice with your vegetables and meat stirred-in as opposed to stir-fried in hot oil should result in higher GI and less RS formation of all kinds.
For your protocol, it would probably make more sense to recommend casseroles over pan-fried cooking techniques.
Sorry if formatting doesn’t come through!
Here is link where those quotes came from:
https://lib.dr.iastate.edu/cgi/viewcontent.cgi?article=2334&context=etd
Thank you so much for this article Norm!!! I have been wondering if the prebiotic I have taken contributed to the development of my SIBO. This article brings clarity and confirmation to my condition.
I have a question for you if you don’t mind. I have recently enrolled a gut healing program to treat my SIBO. However, there is a bottle of fiber in the supplements. It’s meant to use after the pathogen purge. I’m wondering if it would help or not. I would love to hear your thoughts on this.
Thanks.
Thank you so much for this article Norm!!! I have been wondering if the prebiotic I have taken contributed to the development of my SIBO. This article brings clarity and confirmation to my condition.
I have a question for you if you don’t mind. I have recently enrolled a gut healing program to treat my SIBO. However, there is a bottle of fiber in the supplements. It’s meant to use after the pathogen purge. I’m wondering if it would help or not. I would love to hear your thoughts on this.
Thanks. (oh sorry for the duplicate, I forgot to click the notification button)
I’d have to evaluate the nutritional facts for the supplement for a definitive answer, but in general, I view fiber supplements as part of the problem, not the solution.
It contains Quinoa Sprout, Millet Sprout, Buckwheat Sprout, Fenugreek Sprout, Carrot Fiber, Dried Prune Fiber, Barley Juice, Apple Fiber and Cranberry. It is recommend to take 1/4 teaspoon to start.
Taking 1/4 teaspoon of this supplement shouldn’t be much of a problem, but look at the amounts of each fiber in grams and add to daily FP levels to be sure.
Thank you so very much!!! I’ll check the FP content to be sure.
I have been on the Low Fodmap diet for 2 years. It really helped but something was still missing so i finally conceded to spend the money on the MRT Leap food sensitivity test and that did help more but……still something was missing. I wondered why according to the food sensitivity test and the Low Fodmap diet I could eat things like corn, maltodextrin, modified food starches etc. but yet they seemed to be problematic. Well I just ran across you and your info and bingo it sounds like, and hopefully, I might have more of the answer if not all. I have ordered your book but have some questions meanwhile. I have some probiotics that have cellulose, Leucine and silica but no dairy. Is the Cellulose anything that might cause a problem? Does soaking, sprouting lessen the affect of the resistant starch in nuts, grain? Does eating the whole grain flour form lessen the effects? I have been on this journey along time refusing any invasive techniques from the medical profession including pharmaceuticals just because I knew that they would do more harm than good but the kinds of food that I can eat has become increasingly, exorbitantly, stringently limited. I have hopes that I eventually will be able to start adding foods back but as of now I would not know where to start. Thank you
Hi Joy,
Sounds like you’re on the right track. I would not worry about a bit of cellulose in the probiotics. This research paper on soaking beans suggests that soaking can reduce certain fibers as well as sugars and starch content. Be sure to remove and dispose of the water after soaking. https://www.ncbi.nlm.nih.gov/pubmed/12489819
As you will see when you read the book, whole grain flours should be avoided.
Hi Norm,
I discovered your page last night, it was nearly 5 AM and I was in my bed awaken looking for answer with my phone because I cannot sleep due to my gut issues…
After I read it all I was totally crying, for joy, for relief, for frustration…
Let me explain:
I’ve started having severe gas problems some 3 years ago. At first I thought that gas was coming soon after I finished eating. Not knowing the cause, and being very hard to control especiallyat night, being also a bit over weight, I decided to go on diet with a low carb/high protein diet (Dukan)
Immediately my problems went away and I almost forgot them.
After more or less one year I’ve finished the path, and I could go back reintroducing amylacea food which was forbidden during the diet.
After some weeks I started feeling uncomfortable again, at first I thought it was just my body rearranging at the new food, then I realized it was the very same issue I had before, as the symptoms grew stronger and had so much gas I could hardly keep it in public. I spent last year and half doing experiment to understand what was causing my problem. I started understanding that gas started pretty much always after 7 to 9 hours after the “dangerous” meal, but couldn’t understand what was the problem. Couldn’t be gluten, as I ate lot of seitan while on diet.
Couldn’t be milk, I had it on diet as well as cottage cheese and yoghurt.
In Italy Doctors and gastroenterologist don’t seem to care about my problem, someone told me “you’re lucky, if there’s gas it means the bowel’s working!” Some other told me it’s just in my mind and it’s psychosomatic, the gastro ordered a lactose breath test and a liver scan… So I gave up on docs and kept on doing my researches.
Long story short after one year and a half I started again with my trials and removed wheat. It went better, but then I had huge issues with polenta. Removed corn. Had massive symptoms with hummus. It seemed I could have french fries in pubs but couldn’t have instant mashed potatoes or potato salad. Ok, must be carbs. But wait: there’s something wrong: when I’m at “all you can eat” japanese I’m always fine with tons of rice unless I get Udon or Soba… And even at the chinese, where I usually only take “rice cakes” I can sleep tight and peacefully… So how could this be? ( I know I ate a lot of junk food but It was for testing every different type)
I started looking what was in japanese rice and chinese cake that was different than other amylacea, and I’ve found it: No amylose, just amylopectin. So no “difficult to digest” starch, just the easy one.
I spent some more night on the web looking for people with similar issues and finally arrived here, where every single thing described is the analysis of my last year and a half. Even why I could have hot fried potatoes but not cold ones. Why once I had hot pasta and the same pasta the next day made me miserable. Why few days ago I rinced my rice after cooking and I had gas all night long.
That’s why I cried for like half an hour in my bed: my symptoms were real, there was a cause, it wasn’t in my mind and now I had something on which investigate more accurately. So THANK YOU for sharing and for being so detailed, it really saved my lately miserable existence. At least now I’m sure about what to avoid.
The question now is – and I’d like to ask you because this is the most complete page and you seem the most knowledgeable person I’ve found on the web about this – is what should I do now? Why I suddenly couldn’t digest anymore, 3 years ago, all those food I’ve always being eating? And how do I go back to before this happened? Is it because of a deficiency in alpha-amylase? Is it even possible to have or investigate such deficiency? Or is it just about a wrong gut flora and I need to improve it?
Could it be SIBO? No single doctor out of 4 told me about SIBO but when I discovered what it was I talked to my family doctor and he – without testing with breath test – told me to take rifaximina: if I was doing better it was SIBO, otherwise it was not. And I felt better for the first days but then I started having gas again, so I just gave up and thought it couldn’t be SIBO.
I’m sorry to ask all of these questions, but I’m pretty sure doctors here won’t talke me seriously about my discovery and if I search online other sitest to understand why I’m having issues with RS I only find pages about how good it is and its benefits, It feels like this is the only place for me now where to get some help…
Thanks a lot, again, I now know at least that it IS real and that there’s a scientific explaination for my condition.
Best regards, keep on doing this great service,
C.
(sorry again, I forgot, about SIBO, that I don’t have any issues with lactose, alcohol or other sugars…)
Hi Claire,
Thanks for posting and sharing your own observations that are consistent with some of the ideas in the article and Fast Tract Diet approach. Amylase deficiency can be a factor as some people make more amylase than others (amylase gene copy number is highly variable person to person). People who have less to begin with will be more susceptible to things that impact enzymes level – pancreas issues, dietary inhibitors, etc. SIBO and other gut microbiota imbalances can certainly play a role as well. All of these issues can be investigated, and limiting fermentable carbohydrates in the mean time is a good idea. All of these things are discussed in detail in the Fast Tract Digestion books.
Subscribed. Excellent info, hope it continues!
Perhaps this is premature since I have read neither book, but I have a question. First of all, one book addresses heartburn, the second IBS, and this website refers to a book by Dr. Robillard on SIBO, which I have not found. The question is this: is the information and therapeutic approach significantly different between the books, or does the concept of limiting daily FP apply across all three entities? Concretely, if I have both GERD and IBS (many people do), does the information in each overlap to such a degree that one can read either one and still get started?
Thank you,
Arnold Ronning
Hey Arnold, Fast Tract Digestion is a book series. There are two volumes out, one on heartburn and one on IBS. Both books feature the Fast Tract Diet. The diet and FP tables in the appendix are the same. There are many differences between the heartburn and IBS book however, including different recipes and most of the early chapters which are specific to each condition. There is no compelling reason to read both books. I recommend picking the book representing the most troublesome condition. Some people may refer to each of books as “SIBO books” because SIBO is the underlying theme in both books. The Fast Tract Diet is all about treating SIBO and dysbiosis, but there is not book I have written with SIBO as the title. I hope that helps.
Thank you, Norm. Where can I read part 2?
Also, it seems that all of the RS containing foods cause me to suffer from extreme fatigue. Is there somewhere I can find a list of other RS containing foods?
Would you have recommendations for me: cut out RS, get tested for SIBO, etc?
Hi B, Thanks for writing. I noticed the link at the end of the article had been lost. I replaced it, so it should work now.
Based on your own account linking your symptoms of fatigue to RS-containing foods, along with the evidence I present in the FTD books, it seems prudent to limit these foods. Getting tested for SIBO is a personal choice for people who want more information about what’s going on, but others are satisfied with limiting fermentable carbs and feeling better. As for a list of food that are high in RS, the best bet might be to focus on starches that don’t have much RS such as Jasmine or sushi rice as well as several varieties of potatoes discussed in the Fast Tract Digestion book and the FTD Mobile app. Or just look at the tables, that list overall FP points. In the case of starchy foods, most of the points come from RS and in some cases fiber.
Glad I found out about this. I’ve been following a low FODMAP diet for IBS and yet I still get a lot of bloating. Turns out it must be all of the long-grain white rice I’ve been consuming. I just assumed that all white rice was kind of the same and would be easy to digest.