If you want to watch this content on YouTube, click here.
Let’s talk about food and reflux
You may have heard about standard trigger foods for GERD, avoiding fats, fried and spicy foods, citrus fruits, tomatoes, onions, garlic, chocolate, coffee, alcohol, and carbonated beverages. But will avoiding these foods work?
The science is conflicting. This approach is no longer supported by the American Medical Associations, Continuing Medical Education program.
Here’s a quote, “routine global elimination of foods that can trigger reflux is not recommended for the treatment of GERD.”
But here’s my point. The fact that trigger food diets didn’t work doesn’t mean that dietary intervention won’t work. It does mean: however, going back to the drawing board. That’s what I’ve done.
I’m here to share a different approach that stopped my own chronic reflux and led to a new way of looking at this condition.
What is acid reflux?
About 60 million people in the US alone regularly suffer from painful symptoms of acid reflux. Typical symptoms of reflux include:
- Heartburn
- Belching
- Bloating
- Abdominal pain
- Cough
- Regurgitation
- Sour taste in the mouth
- Sore throat
- Hoarseness
- Laryngitis
- Asthma-like symptoms
- Sinus irritation
Smoking, hiatal hernia, obesity, pregnancy, and even tight-fitting clothes can worsen the symptoms.
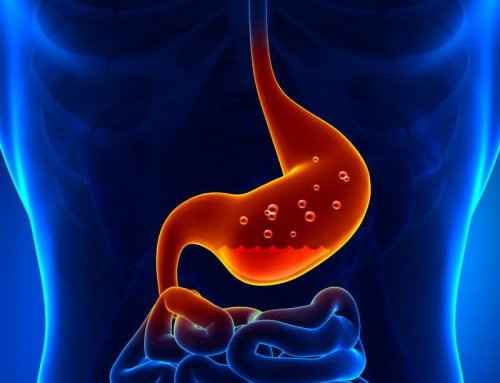
Acid reflux occurs when acid and other contents in the stomach escape into the esophagus and beyond.
Chronic acid reflux often leads to damage because the esophagus and other effective tissues are not protected by the same thick mucus layer that coats the inside of the esophagus. And the result is painful irritation, which can lead to esophagitis, Barrett’s esophagus, and even esophageal cancer.
Persistent damaging reflux is referred to as gastroesophageal reflux disease. Reflux may also cause severe irritation of the throat and vocal cords; a condition referred to as laryngopharyngeal reflux or LPR.
The most rational approach for treating GERD is to stop the reflux, so acid and other stomach contents stay in the stomach they belong.
How do we stop reflux?
You may have heard that reflux occurs when the lower esophageal sphincter or LES (a group of muscles that sits at the top of the stomach and is supposed to keep it closed) becomes weak or inappropriately relaxes.
But does this really happen?
Is this really the cause of GERD?
Or have we been looking at this the wrong way?
Let me share a story about my own chronic reflux and how I resolved it.
I ended up writing two books (Heartburn Cured and Fast Tract Diet Heartburn), proposing a new and different underlying cause of reflux that better fits the facts and does not depend on a weakened or inappropriately relaxed LES.
My story
For 15 years, I suffered from GERD and occasional IBS symptoms.
I took PPIs or proton pump inhibitors and H2 blockers, but they didn’t give me adequate relief.
One thing I did notice was a strong connection between my symptoms and carbohydrates in my diet. In other words, my symptoms improved dramatically when I cut carbs, and I found myself wondering why.
My aha moment
Being a microbiologist, I knew that we have a hundred trillion microbes in our intestines. These microbes get most of their energy by fermenting foods that we don’t digest and absorb.
There are only three food groups, carbohydrates, fats, and proteins, and most of our gut bacteria prefer carbohydrates as the primary fuel source. When they ferment carbs, they can produce a lot of gas.
Only 30 grams of unabsorbed carbohydrates allow bacteria to produce more than 10 liters of hydrogen and other gases.
There is so much flammable gas in our intestines at times that there have been well-documented cases of explosions during intestinal surgery.
New mechanism of reflux
The basic idea I had is that some of us may lose the ability to efficiently digest and absorb carbohydrates in our diet, thus overfeeding these gas-producing microbes. This leads to excessive intestinal gas, which creates a lot of pressure in the intestines.
The gas pressure works its way into the stomach, which is well known to occur. GERD patients have higher intragastric pressure, which is also well-documented.
This gas pressure drives reflux. It pushes the LES, a little like dropping a Mentos candy into a bottle of Coke. This is a very different idea than weakened or an LES that relaxes at the wrong time.
If my theory stands, there is a lot of evidence for this in my books, we have been going about things all wrong. So instead, we need to focus on reducing hard-to-digest but fermentable carbohydrates in our diet. In other words, we need to put microbes on a diet resulting in less gas.
How do we translate this idea?
What should we not eat for GERD, and what should we eat?
The simplest and best way to address reflux is to reduce but not necessarily eliminate hard-to-digest fermentable carbohydrates in our diet. An easy way to do this is to use the Fast Tract Diet system.
The Fast Tract Diet is based on a three-pillar approach
The first one is dietary, limiting these hard-to-digest but fermentable carbohydrates including:
- Lactose
- Fructose and polymers of fructose
- Fiber
- Resistant starch
- Sugar alcohols, except erythritol, which has one gut-friendly sugar, alcohol
But knowing the amounts of these carb types in a given food or drink is almost impossible.
The Fast Tract Diet solved this challenge. Each food or drink is rated based on a fermentation potential or FP point system I created. The lower the FP value for a given food and serving size, the lower the symptom potential. It’s that simple.
The second pillar or second part of the diet is identifying and addressing underlying causes specific to you. There are at least 25 or 30 of these.
The third part or the third pillar is focusing on pro-digestion behaviors and practices that will help you improve your digestion, even when your diet isn’t perfect.
Back to the trigger foods for GERD
When you look at things through this new lens, you may notice that many of these trigger foods contain these hard-to-digest fermentable carbohydrates.
Fats:
Fats often get the blame, but fats themselves, don’t trigger reflux.* However, many fats are linked to high-carb foods.
For instance, French fries are considered fatty, but they are made from potatoes. Depending on the potato, it can have a lot of resistant starch.
Fried Foods:
Fried fish or chicken is considered fatty, but these foods are often with a batter made from corn or wheat, which has a higher amount of fiber and resistant starch.
Fruits and Certain Vegetables:
Citrus is high in sugar and fibers.
Tomatoes, particularly tomato sauces, contain added sugar and other carbs.
Onions and garlic, this family of vegetables is relatively lower in carbs, but those carbohydrates are composed of fructose oligosaccharide, which is like fiber, hard to digest, and very fermentable.
Chocolate and Coffee:
Chocolate is high in sugar and high in fiber.
Coffee contains some fiber, and many people add sugar and sweetened creamers to their coffee.
Alcohol is not a trigger, but beer, sweet wines, and sweetened drink mixes are much higher in sugar and carbs. Likewise, carbonated beverages are often high in carbohydrates.
Grains, Legumes, Sugar, and other carbohydrates:
Limiting these higher-carb versions of trigger foods make sense, but here’s the problem. The trigger food diet doesn’t go far enough.
Other foods high in fermentable carbs include various grains, legumes, bread, and desserts, not necessarily on the trigger food list.
Next step
For more information on the Fast Tract Diet, you can download my free ebook on the home page. For questions and support, you can join the Fast Track Diet Facebook group.
For individualized help, contact me through our form or call (844) 495-1151 US Mon – Fri from 8:30 am to 5 pm ET.
* Refer to 2, 3, and 4 references in the GERD diet that works without drugs article.




Leave A Comment
You must be logged in to post a comment.