If you want to watch this content on YouTube, click here.
If you have the following symptoms, you may suffer from low stomach acid:
- Gas
- Heartburn
- Bloating
- Burping
- Diarrhea
- Constipation
- Nausea
- Feeling fullness
- Fatigue
Another name for low stomach acid is hypochlorhydria. But some people don’t make any stomach acid, and a condition referred to as achlorhydria.
We need our stomach acid, and a lack of it can cause a variety of health issues, including:
- Poor digestion
- Nutritional deficiencies
- Poor absorption of vitamins and minerals, vitamin C, D, B12, folic acid, iron calcium, zinc, and magnesium
You are more susceptible to bacterial overgrowth if you do not have enough stomach acid. For example, bacteria from your intestines more easily overgrow in the small intestines known as SIBO (Small Intestinal Bacterial Overgrowth). In some cases, bacteria are able to grow in the stomach when there is insufficient acidity to prevent it.
You are also more susceptible to gastrointestinal infections, Clostridium difficile (D-diff), and Salmonella, for example.
Stomach acid is a two-way block, both pathogens coming in with food and water, but also bacteria from your intestines refluxing and getting into your lungs, linking to increased rates of pneumonia and asthma. You can also suffer from weight loss, anemia, and your risk of stomach cancer goes up.
But here’s the problem.
Many other issues can cause these symptoms and health conditions. So how do you know if you have low stomach acid?
6 Common Causes of Low Stomach Acid
These are 6 common causes. Let’s go through them one by one:
1. Acid-reducing drugs
If you are taking PPIs or H2 blockers or a combination of both, you are most certainly to have low stomach acid. This is because PPI binds to the parietal cells’ acid pumps and permanently blocks acid production. And the only way your stomach can produce acid is if these parietal cells produce new acid pumps. So it’s no surprise that PPIs are linked to an increased risk of death and serious health problems.
H2 blockers, on the other hand, block histamine by binding to H2 receptors on the parietal cells that turn on stomach acid. So you’re blocking the release of acid. However, you can still shut down the acid pretty well for six to eight hours.
The Fast Tract Diet addresses heartburn, acid reflux, GERD, and LPR without drugs. For more information, please read the Fast Tract Digestion Heartburn book.
2. Chronic H pylori infection
Helicobacter pylori is a bacterium shaped like a corkscrew that burrows through the mucus and sticks to the lining of your stomach.
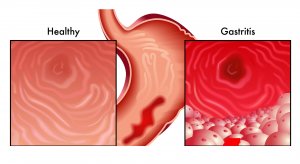
Over time, H. pylori infectious colonies damage the stomach leading to gastritis which is inflammation of the stomach lining. Eventually, it can lead to atrophic gastritis, a loss of functionality wherever these colonies form in your stomach, and even ulcers.
You can get low stomach acid from a chronic H pylori infection. But just a quick note, depending on where these H pylori infectious colonies are in your stomach, you can also have hyperchlorhydria, too much stomach acid, which puts at risk for ulcers.
3. Pernicious anemia (autoimmune atrophic gastritis)
It occurs when your immune response – antibodies attack your parietal cells, and they can lose functionality including the ability to produce stomach acid.
Your parietal cells can also lose the ability to produce intrinsic factors to absorb vitamin B12. Hence the name pernicious anemia, low B12, and you can become anemic.
People with autoimmune conditions, particularly Hashimoto’s, but also type one diabetes, celiac disease, ankylosing spondylitis, and Sjogren’s, etc., are at a greater risk for autoimmune atrophic gastritis.
4. Frequent use of non-steroidal anti-inflammatory pain medicines (NSAIDs)
NSAIDs (aspirin and ibuprofen, for example) irritate and damage the stomach over time. And they can cause atrophic gastritis, loss of stomach acid.
NSAIDs can also lead to ulcers.
Another reason to avoid NSAIDs is that they can cause tiny tears in your small intestine called NSAID enteropathy. If you need a painkiller, Tylenol might be a better choice.
5. Deficiency in minerals or electrolytes, zinc, sodium, and other electrolytes
These are required to produce stomach acid. So looking at them through an expanded blood test, you can get a read-on this.
This is an important idea, but you’d need to be careful not to over supplement either. For instance, many people take large amounts of zinc, and though you do need enough zinc to produce stomach acid, too much may shut down stomach acid.
Staying within the RDA for zinc – eight milligrams a day for women and 11 milligrams for men might be best unless you check your levels first.
6. Gastritis
As many as half of the people on the planet may have chronic gastritis.
If you’ve had an endoscopy, and the doctor tells you, it’s very red and inflamed down there. You have gastritis. Regardless of what’s causing it, it’s important to follow up.
Rare Causes of Low Stomach Acid
Some of the rare causes of low stomach acid include:
- Prolonged HIV infection
- Stomach surgery bypass
- Tumors of cancer of the stomach and radiation treatment
What now?
If you don’t know the status of any or some of the 6 common causes, it would be a good idea to get tested. If you are positive for one or more causes, the best test for low stomach acid is the Heidelberg acid test.
The Heidelberg acid test is often provided by functional medicine practitioners who have the device.
To begin the test, you will swallow an electronic capsule on a string that dangles in your stomach. The capsule radios out your pH to a laptop. Once the capsule determines baseline pH (hopefully below 2), you will be challenged with bicarbonate drinks several times, which will raise the pH to near neutrality (pH 7 or so).
Each time the practitioner will determine how long it takes your stomach to reacidify back to a pH between 1 and 2. If your stomach takes too long to reacidify (30 – 50 minutes for example), you will likely be diagnosed with hypochlorhydria. If it doesn’t reacidify at all after several trials, you may be diagnosed with achlorhydria.
Take-Home Message
Stomach acid is essential for our digestive and overall health. Therefore, it’s critical to understand your underlying causes of low or no stomach acid.
As a consulting microbiologist, one of the first things I do when working with my clients is to find out if they’re at risk for hypochlorhydria. If they’re not, we move on to the next 25 or 30 causes of functional gastrointestinal disorders, gut dysbiosis, and related health issues and dig each one deeper.









Leave A Comment
You must be logged in to post a comment.