What is the most effective SIBO diet?
Since releasing my first book in the Fast Tract Digestion book series on Heartburn which linked chronic acid reflux to Small Intestinal Bacterial Overgrowth (SIBO), I have received many inquiries about using the Fast Tract Diet to treat other SIBO-related conditions such as IBS (update: Fast Tract Digestion IBS / Fast Tract Diet App now available) and celiac disease. To answer this question, I am going to review several other diets that may be applicable to treating SIBO along with the Fast Tract Diet.
What is SIBO?
In healthy people, the small intestine contains low levels of friendly bacteria such as Lactobacillus acidophilus, especially in the upper part of the small intestine where our own critical digestion takes place. SIBO involves the invasion of the small intestine with much greater numbers of bacteria from the large intestine.
The official definition of SIBO is “the presence of an abnormally high number of bacteria (more than 100,000 bacteria per milliliter) in the upper part of the small intestine”. At this level, the normally harmless bacteria that live in our gut can become harmful. They produce toxins, enzymes, and intestinal gases, including hydrogen, methane, and carbon dioxide that can disrupt digestion, cause intense physical discomfort and even damage the small intestine.
The symptoms of SIBO include abdominal pain or cramps, diarrhea, constipation, gas, bloating, acid reflux, flatulence, nausea, dehydration, and fatigue. More severe symptoms related to SIBO can include weight loss and “failure to thrive,” steatorrhea (the body’s failure to digest fats), anemia, bleeding or bruising, night blindness, bone pain and fractures, leaky gut syndrome, autoimmune reactions, and among others.
There is an abundance of scientific research linking SIBO to a growing number of digestive (and even systemic) conditions. The list continues to grow but already includes:
- Irritable bowel syndrome (IBS)
- Gastroesophageal reflux disease (GERD)
- Celiac disease
- Crohn’s disease
- Diverticulitis
- Fibromyalgia
- Chronic fatigue syndrome
- Asthma
- Rosacea
- Interstitial cystitis
- Autoimmune disorders
- Cystic fibrosis
SIBO has many underlying causes, but here some that stand out:
- Slowed motility (how well food moves through the intestine)
- Low stomach acidity
- Immune deficiency
- Antibiotic usage
- Pancreatic insufficiency
- Low ileocecal valve pressure (separates the large from the small intestine)
- Damage to intestinal villi (finger-like projections for absorbing nutrients)
- Food poisoning or gastroenteritis
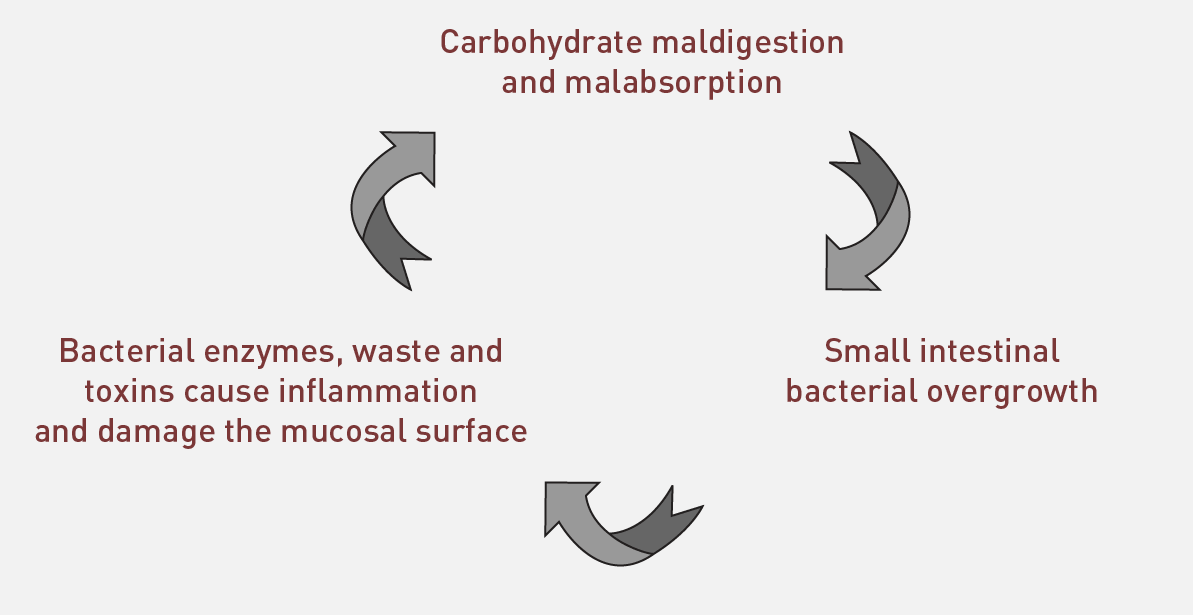
- Carbohydrate malabsorption (key for dietary control)
Though each of these issues could increase your chances of having SIBO and should be identified and addressed where possible, the driving force behind SIBO is always poorly absorbed carbohydrates. That’s because gut bacteria consume mostly carbs for energy.
For this reason, the best way to control SIBO is to deny gut bacteria the fuel they need to overrun the small intestine by limiting the consumption of certain carbohydrates. The worst offenders are the hard-to-digest carbohydrates including:
- Lactose
- Fructose
- Resistant starch
- Fiber
- Sugar alcohols
The Fast Tract Diet considers these hard-to-digest carbs as having “Fermentation Potential” (FP). Limiting FP, as opposed to limiting overall carbs, is the secret of lasting symptom relief. Fast Tract Digestion uses an FP point system to control hard-to-digest carbs.
SIBO Diets
Back to the question, “Can the Fast Tract Diet be used to treat other SIBO-related conditions?” The answer is yes, although specific conditions may have additional requirements. For instance, any diet for celiac disease would require all gluten (even small amounts) to be removed. With this in mind, the Fast Tract Diet is specifically designed to treat SIBO by limiting the carbohydrates listed above that drive bacterial overgrowth.
Other diets have also been used to treat SIBO-related conditions. These include:
- Paleo Diet
- Elemental Diet
- Specific Carbohydrate Diet (GAPS Diet)
- Low Starch Diet
- Low Carb Diet
- FODMAP approach
These diets all limit carbohydrate malabsorption to varying degrees. Let’s take a closer look at each.
The Paleo Diet
Paleo diet experts make a rational case that eating as our ancestors ate is healthier. The reason is, our bodies evolved in balance with the foods that were available before we learned to cultivate grains. You hear different opinions on the details as no one knows for sure what paleolithic humans ate or what their diets were like locally. More fruits would be available in tropical areas. People near lakes, rivers, or the ocean relied more heavily on aquatic foods. Hunting was a common thread as supported by fossil records. Foods tended to be uncooked and many foods we tend to dismiss in the modern Western world (i.e. insects) were likely part of the caveman diet.
I have gained a general view of Paleo diet foods from reading some great books including, The Paleo Solution, by Rob Wolf, The Primal Blueprint by Mark Sisson, and Perfect Health Diet by Paul snd Shu-Ching Jaminet. Other excellent sources of information on Paleo eating include Danny Alber’s Blog, Primal North (for real deal, hardcore Paleo – not live at this time) and the website, Paleohacks.com. I also attended the two most recent Ancestral Health Symposia (you can see my ASH2013 presentation here).
My takeaway message is this.
“Modern Paleo diets are based on food types that were available and consumed during our evolution.”
Included:
- Fish, meats; including organs, fowl, and eggs
- Green vegetables, fruits, nuts, seeds, and herbs
- Insects
Limited:
- Cassava, Sweet Potatoes, Yams, Wild rice, Taro
Off Limits:
- Most grains (though Mark’s plan allows some wild rice and Paul Jaminet’s Perfect Health Diet allows more starch including white rice)
- Beans and pulses
- Dairy and foods containing dairy
- PUFA-containing oils except olive and coconut oil
- Processed foods containing sugars and trans fats, nitrates, and other additives.
Clearly, this diet is a big step in the right direction for gut health! The Paleo diet removes or limits many difficult-to-digest carbohydrates that are tied to SIBO. Let’s take a closer look at Paleo diet foods to see if some might give Mark’s caveman, Grok, a little indigestion.
Removing most grains, beans, pulses, dairy, and processed sugars should make a big improvement in reducing SIBO-related symptoms. But, I would advise caution on some of the other “acceptable” food choices when experiencing symptoms.
Some white rice (basmati and Uncle Ben’s for example) are known to contain significant amounts of resistant starch and should be limited. Wild rice likely contains significant amounts of resistant starch, though I can’t confirm this as a fact without a GI value and I don’t believe wild rice has been tested.
I would recommend jasmine rice with a known Fermentation Potential (FP) value of zero. But, don’t eat too much if you have high blood sugar or insulin resistance.
How about fruit? Many fruits contain high amounts of fructose. Because fructose is a single sugar, it requires no digestion, but it’s absorbed slowly into the bloodstream. This makes it more available for excessive fermentation in the gut. There are many studies liking fructose consumption to gut problems, especially IBS symptoms. Apples, pears, cherries, grapes, plums, are examples of fruits containing a lot of fructose.
Another fruit that can create issues is bananas. Bananas have a lot of resistant starch, especially under-ripe bananas. Resistant starch, like all difficult to digest carbs, hangs around providing gas-producing bacteria fuel.
What about dairy? Dairy is restricted on the Paleo diet because it wasn’t an available food source throughout our evolution. For gut health, the major issue is lactose. I agree that high lactose dairy such as milk and ice cream (there is lactose-free ice cream available) should be avoided. I don’t see the benefit of excluding a number of other low-lactose or fermented dairy foods discussed in my book. I personally can’t imagine life without them.
Of particular interest are tubers and root vegetables, which are allowed on most Paleo diets. These include potatoes, sweet potatoes, parsnips, celery root, carrots, beets, daikon, yams, and turnip. Some contain significant amounts of resistant starch and should be limited. See my recommendations at the end of the article for safe choices.
The Elemental Diet
The Elemental diet consists of foods that are essentially “predigested.” The foods contain fatty acids rather than fats, amino acids rather than proteins, and glucose instead of carbohydrates. The diet formula also includes water and micronutrients — vitamins and minerals.
Elemental diet products such as Nestle’s Vivonex can be delivered orally or enterally (by tube). Elemental diets are designed to ensure full absorption and have been used to treat a broad range of digestive conditions including Crohn’s and celiac disease, lactose intolerance, malabsorption, diarrhea, constipation, diabetes, cystic fibrosis, abdominal distention, and short bowel syndrome.
Note that all of these conditions have a connection to SIBO. Some limitations of the elemental diet approach include high cost, unappealing (predigested) food products, and the need for medical supervision.
The Specific Carbohydrate Diet
The book Breaking the Vicious Cycle by Elaine Gottschall describes her experiences with Drs. Sidney and Merrill Haas, who successfully treated celiac disease with a diet that allowed only specific sugars and starches. The Specific Carbohydrate Diet limits disaccharide or double sugars as well as grains and starch but allows simple sugars like glucose.
In general, this dietary approach is on the right track, but some carbohydrates potentially contributing to SIBO-related illness are not limited. For example, honey is used extensively in the recipes even though honey has just as much fructose as table sugar (sucrose is made of equal parts glucose and fructose). And the diet allows a large variety of fruits and fruit juices that also contain large quantities of fructose, which is now recognized as a major contributor to the development of SIBO.
Finally, the SCD does not allow any grains or foods containing starch. It identifies amylose starch as easy to digest and amylopectin starch as difficult to digest. In other words, the diet suggests that amylopectin is more likely to cause problems. But, the reverse is actually true.
Uncle Ben’s rice, for example, contains both amylose and amylopectin starch and it has a high FP / symptom potential, while sushi rice which contains no amylose (only amylopectin) has a very low FP / symptom potential.
Note: The GAPS Diet (Gut and Psychology Syndrome) created by Dr. Natasha Campbell-McBride is based on the Specific Carbohydrate Diet but also includes detoxification and supplementation.
The Low Starch Diet
Carol Sinclair popularized the Low Starch Diet in her book The IBS Low-Starch Diet. Sinclair discovered that reducing starch in her diet improved her IBS symptoms. She also collaborated with Dr. Alan Ebringer, a professor of immunology at Kings College in London, UK, who found that the diet could improve painful symptoms of ankylosing spondylitis (AS).
Dr. Ebringer has made the connection between the autoimmune disease AS, intestinal overgrowth of the bacterium Klebsiella pneumonia, and controlling the bacteria’s growth through a low-starch diet. Sinclair’s book limits all starches as well as sucrose, lactose, and maltose.
Like the Specific Carbohydrate Diet, the Low Starch Diet unnecessarily limits all starch, yet does not limit fructose, thus limiting the effectiveness in treating SIBO.
The Low Carb Diet
The book Protein Power by Drs. Mike and Mary Dan Eades documented how low-carb dieting helped people with heartburn. Clinical studies have also shown that strict (ketogenic) low-carb dieting can improve IBS and GERD, two conditions associated with SIBO [i] Despite impressive results (as documented in my first book, Heartburn Cured), not everyone gets complete symptom relief from a low carb diet.
One possible explanation for the variations in results is that the low-carb diets don’t specifically restrict fiber (though limiting high carb foods also limits fiber) or sugar alcohols — known contributors to SIBO-related digestive illness. Another reason might be a simple failure to stick with the diet.
The FODMAP Approach
Susan Shepherd and Peter Gibson developed the FODMAP Diet at Monash University in Victoria, Australia.[ii] The acronym FODMAP represents four classes of fermentable sugars/sugar alcohols: Fermentable Oligo-, Di-, and Monosaccharides, And Polyols.[iii] The FODMAP approach limits fructose, fructans, lactose, galactans, and sugar alcohols.
While the approach makes sense and has helped people with IBS and other SIBO-related conditions, the FODMAP diet includes sucrose in many low FODMAP recipes and does not restrict resistant starch and fiber found in sweet potatoes, certain kinds of rice, corn, gluten-free pasta, gluten-free bread, cereals and bananas for example.
Sucrose, because it’s half fructose, and resistant starch are both significant contributors to malabsorption and excessive fermentation. The FODMAP diet actually calls for adding more resistant starch. As a recent article on the diet stated, “Part of dietary counseling is to ensure continuing adequate intake of resistant starch.”[iv]
The Fast Tract Diet – New Way to Treat SIBO
The Fast Tract Diet limits all difficult-to-digest carbohydrates including:
- Fructose
- Lactose
- Fiber
- Resistant starch
- Sugar alcohols
And the diet uses a special method called Fermentation Potential (FP) to calculate the potential for any food containing carbohydrates to cause symptoms. Mathematically derived FP values (they are listed in 15-16 tables in the books but can also be calculated) for each food help identify and restrict difficult-to-digest carbohydrates without having to know what specific carb types are in each food. So you don’t need the help of a medical professional or dietician.
The Fast Tract Digestion book series also explains and addresses the other underlying problems listed above that can contribute to SIBO.
In addition to the overall recommendations in the books, here are 5 recommendations that are missing in some of the other diets to control SIBO and limit symptoms:
Limit high amylose rices
High amylose kinds of rice are high FP. There are lower amylose kinds of rice available that are safe for gut issues.
Limit high amylose tubers or root vegetables
High amylose tubers and root vegetables are also high FP. There are other low FP choices such as parsnips, and several potato varieties available.
Limit sucrose and high fructose fruits
Sucrose and high fructose fruits are high FP. These can be substituted with many Low FP fruits such as strawberries, cantaloupe, and others. Consume other (high FP) fruits, such as apples and bananas as small wedges or single slices. Switch out high FP sucrose with Low FP sweeteners such as dextrose, erythritol (the one safe sugar alcohol), etc.
Limit dairy with excess lactose (high FP)
Acceptable alternatives include cream and a variety of fermented dairy products.
Limit fiber and sugar alcohols (except erythritol)
They are poorly digested and fermentable potentially driving SIBO and symptoms.
Note: Some low FP starchy vegetables, while gut-friendly, are higher in carbs. Use your judgment and limit your overall carb levels to avoid metabolic complications from high blood sugar, such as metabolic syndrome, diabetes, obesity, and cardiovascular health.
How to get started with the Fast Tract Diet for SIBO
 1. Read the Fast Tract Digestion IBS book
1. Read the Fast Tract Digestion IBS book
2. Get the Fast Tract Diet Mobile App for Android or iPhone/iPad
3. Take the On-demand SIBO Masterclasses (2 classes and Q&A sessions for the price of 1)
Need Individualized help for SIBO and/or other digestive health issues? Call for consultation at 844-495-1151 US or contact via this online form.
If you liked this article, you may want to read:
SIBO Treatment: Antibiotics or Diet?
[i]Yancy WS Jr, Provenzale D, Westman EC. Improvement of gastroesophageal reflux disease after initiation of a low-carbohydrate diet: five brief cased reports. Altern Ther health med. 2001. Nov-Dec; 7(6):120,116-119. Austin GL, Thiny MT, Westman EC, Yancy WS Jr, Shaheen NJ. A very low-carbohydrate diet improves gastroesophageal reflux and its symptoms. Dig Dis Sci. 2006 Aug;51(8):1307-12. Austin GL, Dalton CB, Hu Y, Morris CB, Hankins J, Weinland SR, Westman EC, Yancy WS Jr, Drossman DA. A very low-carbohydrate diet improves symptoms and quality of life in diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009 Jun;7(6):706-708.
[ii] Shepherd S, Gibson P. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J Am Diet Assoc. 2006 Oct ;106 (10):1631-9.
[iii] Gibson, P, Shepherd, S. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb ;25 (2):252-8 20136989.
[iv] Peter R Gibson, Susan J Shepherd. Evidence-based Dietary Management of Functional Gastrointestinal Symptoms: The FODMAP Approach. J Gastroenterol Hepatol. 2010;25(2):252-258.

 1. Read the
1. Read the 




Hi Norm, love your work! I am one of the folks that while on a low carb diet my heartburn/reflux gets worse. I have SIBO and know to stay away from fiber, sugar alcohols, etc. What do you think about Paul Jaminet’s (Perfect Health Diet) suggestion that the bacteria feed not just on excess carbs, but also on ketones when on a low carb diet? Would love your opinion!
Hi Sarah,
Thanks for writing and for your kind remarks. I had not heard of this diet, so thanks for bringing it to my attention. First off, Paul lumps together all rice and potatoes. This is wrong for people with SIBO as some rice and potato varieties have lots of resistant starch, others have little or none.
On the idea of gut bacteria using ketones, I have never heard of this concept before. Let me dig into this and get back to you.
Update 11/25/18: Since posting this comment, I wrote a blog on Candida and fermentable carbs which includes a mini debate with Paul at the end of the article about ketones and Candida. https://bit.ly/2d0NjnT
Wonderful, thank you!
Hi Norm, just checking in!
I think Paul was talking more about ketones feed fungi (eukaryotic?) organisms.
Thanks Tom. That makes more sense. One testimonial in the book from someone with Crohn’s advocating a ketogenic version of the diet that is low in fiber notes that bacteria don’t feed on ketones, but I don’t see mention of fungi in this context.
Hi Norm, I went through your book it is a wonderful book that gave me a lot of new informations regarding SIBO. Before reading this book I was planning to go absolute cereal free which I thought would be the toughest thing to do, but now I have some options thanks to you. Well I have a few questions for you.
1. as I have read in Breaking the vicious cycle, apple and banana are listed in legal foods. what is your view?
2. can I drink pure glucose as a substitute for cereals?
3. what is your opinion on taking pysallium husk?
Hi Kripal,
Thanks for writing and your positive remarks.
As for your questions:
1. As I discuss in Fast Tract Digestion, Breaking the Vicious Cycle does not limit fructose and there is lots of fructose in apples and bananas. Bananas also have quite a bit of resistant starch. I would go by the Fermentation Potential tables. A 120 gram serving (4.2 Oz) of apple has an FP equal to 12 grams. A whole apple is about 180 grams for a total FP equal to 15 grams. That’s considered high – having significant symptom potential. You might consider having a one quarter of an apple and evaluate your symptoms. Bananas have an FP of 15 (ripe) to 18 (green) grams which is high. Again, you could try 1/3 of a banana once your symptoms are under control.
2. Glucose drinks should be avoided for a couple of days as you start the diet. Once SIBO and symptoms are reduced, glucose drinks should not trigger symptoms. Just keep in mind that foods that raise blood sugar quickly and significantly, in the absence of exercise, are not particularly healthy and can lead to other problems like obesity, diabetes, etc. over time.
3. I don’t think fiber, above what you get from green stalked and leafy vegetables, is needed. In many people, fiber supplements make symptoms worse. Also, some fiber supplements contain lots of sugar which contains lots of fructose which can also lead to symptoms. Lastly the FDA has warned of choking and intestinal blockage risks associated with fiber supplements. I don’t recommend these supplements, but if you try them, drink lots of water.
You might be interested in the three part article I wrote called “I thought fiber was good for me“.
Thanks, great information.
Hello, Norm,
A year ago, I was diagnosed with SIBO at Cedars-Sinai. I also have gastritis/esophagitis and asthma. Five years ago, I started on PPIs (before gut symptoms and worsening asthma). My husband and I have been reading about bacteriotherapy and its successful use in treating IBS, Crohn’s, etc. I mentioned this to my gastro doc and he said, “No, no, only for C-Diff.” Yet you, too, mention the possibility in your new book. 1) Can you recommend a gastroenterologist who might be more open to such therapy? 2) Do you recommend Apple Cider Vinegar or baking soda for reflux? (I’m reducing the PPIs.)
Hi Cecilia,
Your doctor is right – The primary use of this procedure currently is C diff infection. However, some work has been done on IBS.
You might try writing to the master of this technique, Thomas Borody (thomas.borody@cdd.com.au) to see who he recommends in the US. Dr. Pimentel may have a suggestion as well. Also check out Brorody’s excellent review (Borody TJ, Khoruts A. Fecal microbiota transplantation and emerging applications. Nat Rev Gastroenterol Hepatol. 2011 Dec 20;9(2):88-96. doi: 10.1038/nrgastro.2011.244.). Specifically, look at references 46 and 47.
Many people swear by cider vinegar for low stomach acid, but the most important way to improve acidity is to work with your doctor to wean yourself off the PPIs. Of course, if you’re still refluxing, you will experience heartburn and other symptoms. I recommend the Fast Tract Digestion Diet as your are reducing the PPIs. Using antacids can help with breakthrough symptoms. At least you will only be reducing acidity on a temporary basis which is better than 24/7.
Thank you very much for getting back to me so rapidly. I’ll follow up on the links you sent re: bacteriotherapy.
Have you, perchance, read Gary Taubes’ books, Why We Get Fat and Good Calories, Bad Calories? (I am thin — 108 pounds, 5’5″, but find an echoing theme of yours — carbs reduction. His prescribed diet, though, is draconian, in that he eliminates all carbohydrates.) I’m wondering what your opinion of either his books or Wheat Belly, by William Davis is.
I have read Gary’s book Good Calories Bad Calories and agree with Gary on the health benefits of low carb dieting. I personally restrict carbs though not generally on the very low carb end. Low carb generally works well for gut / SIBO issues as well. But there are some unrestricted food types on low carb such as fiber and sugar alcohols that can cause gut problems. I am reading Wheat Belly currently after meeting William earlier this year. I find his research fascinating, though, its very clear to me that wheat alone is not responsible for digestive issues.
Again, thank you for getting back to me.
I’m wondering if I might BUY hard copies of your book. I’d like to give one to my Primary Doctor and another to my brother-in-law, Garrison Bliss, M.D., a well-known internist in Seattle who pioneered affordable concierge medical care. He still sees many patients and would undoubtedly be fascinated by your own research.
Thanks for your interest in sharing the book. You can find it on the “buy books” tab on this site. I was just reading your brother in law’s blog on Direct primary care medical homes on the Huffington Post. He has some great ideas. Please let him know that I would very much enjoy receiving his thoughts on the ideas in the book.
FYI. I wanted to let you know that the Oct. 22 edition of the New Yorker has a fascinating article called “Germs Are Us” by Michael Specter. A point it makes is that antibiotics are herbicides for humans. That while medically necessary, they change the ecology of our bodies in unimaginable and unhappy ways.
But you already know that.
Thanks Cecilia,
I read what I could but don’t have a subscription to read the whole article, but looks very interesting.
By the way, thanks for sending the article Cecilia. Fantastic read!
Hi, I have just ordered the Fast Tract Digestion Heartburn book and was wondering if the diet is safe during pregnancy? I am 9 weeks pregnant and having a terrible time with GERD, which I have had for 20 years ( I had Barrett’s oesophagus when I was 21). I have been on a PPI for the past 10 years but I went off it when I found out I was pregnant. Now I can’t eat without getting terrible reflux and I have trouble sleeping due to bad stomach pains. I eat a small meal and feel like I have eaten a 5 course banquet. I have cut out acidic foods but it doesn’t make much difference, I still get reflux all the time. I’m really worried about how I’m going to cope with the increased intra-abdominal pressure that will come later in my pregnancy…
Hi Mandy,
I feel for you as the PPI rebound effect can be quite considerable when you first stop. The diet will help minimize this temporary problem. Also, the Fast Tract Diet is based on whole healthy foods and should be fine for pregnancy. Just don’t overdue it with the carbs as gestational diabetes can sometimes arise half way into your pregnancy. But that shouldn’t be too much trouble as the daily carb count of the Fast Tract Diet meal plans is approximately 75 grams per day.
Thanks very much Norm, I think I’ll try going paleo with the inclusion of your 4 recommendations above, hopefully thst will give me some relief until I understand more. Thanks again :)
Mandy,
Check with your doctor first, but you sound like you might benefit from supplementing stomach acid, as discussed here: https://scdlifestyle.com/2012/03/how-to-supplement-with-betaine-hcl-for-low-stomach-acid/
It’s helped me a lot–I was also on Prevacid and decided to voluntarily stop taking it because of the risks and side effects. I had horrible reflux at first, but more or less following the SCD/paleo diet and supplementing HCL has helped a lot. You might also check out DGL and zinc carnosine.
Dr. Robillard:
I have been researching Gerd for about 5,000 hours over the last 2 and a half years. I just ordered fast tract digestion and am thrilled to receive it soon. I weaned myself off proton pump inhibitors and adopted a low carbohydrate lifestyle. I am happy to say that I have experienced almost zero reflux in the past 2 weeks. 1 question for you: Although I am experiencing little to no reflux symptoms anymore, I feel very confident that your method works. My LES valve is still open 24/7. I believe the valve to be controlled autonomically, and am curious if the valve will eventually close on it’s own? Should I consider taking HCL tablets? I feel I have cured the reflux, but not the low acid/and LES valve problem. Thank you for all of your work. I can’t thank you enough.
-Joey in Portland, OR
I apologize for the grammatical errors above. I should have opted for a full computer screen instead of a smart phone haha. One thing I think would be pertinent to mention is that I was using 20 mg of omeprazole for 2.5 months. Prior to that, I was using organic apple cider vinegar before each meal and felt the valve close. My belching sounds hollow now. It’s quite strange. Thanks again!
Hi Joey,
Didn’t notice any grammar errors. Probably why I need an editor for my own writings. In a nutshell, if your reflux is under control and your off PPIs, I would say congratulations, you’re done. I would not recommend any other changes such as supplementing with vinegar or HCL. Now that your refluxing is controlled, the tone of your LES should improve over the coming months.
Brilliant! That makes sense. My fingers are crossed. I really hope my acid levels return, and that valve closes. Patience I guess :) I have been on aspirin therapy for an acute stroke I had about 10 years ago. It is also enteric coated. From my understanding, the aspirin dissolves in the small intestine when enteric coated. I’m not sure if you have come across anything about the harmful long term side effects of aspirin therapy in your work? I have not found conclusive evidence that it will prevent or stop another stoke/heart attack from occuring. I plan on working with some naturopaths to implement other herbs and fish oil to keep my blood from clotting instead of using aspirin. I feel that perhaps this could be a factor in my issues as well? Thank you again for all of your work. You’re my hero! I can’t wait to show your book to my gastro and the surgeons I was speaking to.
Thanks Joey. If you were talking about statins for cholesterol, I might agree. But if I was in your situation and my doctor told me to take enteric coated aspirin, I would do it. You can have a discussion about long term risks of aspirin therapy (likely dose related) with your doctor, but I think the benefit of aspirin for preventing stroke is pretty solid.
I came across your website during my search for an answer regarding SIBO and diet. I am glad you made the differences in the prevalent diets clear. I am definitely going to get your book. There is one remaining question I have. I’d love to use cream, dairy and yoghurt but I tested positive for lactose intolerance first (taking Lactase now). When that didn’t help with my symptoms, I had a test for SIBO and tested positive. Now, the question is: what comes first: SIBO causing lactose intolerance or lactose intolerance causing SIBO. How will I deal with the dairy etc. that you suggest using in your recipes?
I definitely want to use your diet to help ease and hopefully correct my digestive tract problems. I have been on and off antibiotics since December 2009 for various reasons.
I am looking forward to your response.
Hi Marlis,
Great question. This is absolutely a classic “chicken and egg” question. The truth is both. Lactose intolerance can lead to SIBO and conditions involving SIBO can lead to lactose intolerance. The evidence is clear and described in the book. Lactose is included in the fermentation potential formula (because of its effect on the glycemic index of lactose-containing foods). Following the diet program should take care of symptoms as it significantly limits lactose. If you have severe lactose intolerance and continue to consume too much lactose, you might benefit from continuing lactase supplements. Lactose intolerance is the easiest to treat because you have the option – limit lactose or take lactase. You don’t get that choice with fructose intolerance, for example.
Thank you for your quick response. I am now waiting for your book to arrive – which should be on it’s way from Amazon.
Hello,
Thanks so much for a great article explaining current trends in SIBO treatment and comparing the pros and cons. I was wondering if you could elaborate a little bit on this statement: “Finally, the SCD does not allow any grains or foods containing starch. It wrongly identifies amylose starch as easy to digest and amylopectin starch as difficult to digest, suggesting that amylopectin and not amylose is more likely to cause problems. The reverse is actually true.”
Could you explain a bit more about what this means? What foods are high in amylopectin, and yet still safe to eat, and which would you say contain a lot of amylose and should be avoided?
Thanks in advance for your help.
Hi Christina,
The book has several examples but here are a couple. Basmati rice is higher in amylose and more likely to cause symptoms than short grain glutinous (nothing to do with gluten) or sushi rice which is 100 percent amylopectin with no amylose and least likely to cause gut symptoms.
Thank you very much for replying. I am planning on buying your book today.
I was curious, where does coconut flour fit in (if at all) in the Fast Tract plan? I have read that it is high in fiber and protein. Do you know if it has a high FP? It’s something of a staple in Paleo cooking and is permitted on SCD, which is why I ask.
Thanks again!
Great question CM. I have actually been looking into coconut flour. The numbers vary quite a bit as to the amount of fiber in coconut flour but range as high as 60 g fiber per 100 grams of flour. Coconut fiber is also fermentable by gut microbes, but the question is how fermentable? If it’s fermentability is closer to the toughest fiber, cellulose, it might not be too bad, but the amount of fiber is cause for caution. In the absence of more research, I would recommend first getting your symptoms under control with the Fast Tract Low FP approach. Then in a more controlled fashion, try consuming some foods made with coconut flour to see how much you can eat before getting symptoms. Then report back to us!
Thanks again for responding so faithfully. I ordered your book today and am going to follow the recommendations. I appreciated hearing your thoughts on coconut flour—I suspect it may be pretty fermentable b/c I seem to have symptoms after eating it in breakfast items.
I’ll report back and let you know how things are going after following the plan in your book.
I hear you CM. I have yet to try foods made with coconut flour, but too many macaroons (made with unsweetened coconut flakes and Splenda) leads to some gut growls for me.
I look forward to hearing from you.
Still waiting on the book to arrive, so I hope you don’t mind another question. I was doing some reading about resistant starches and came upon this article saying that some food’s resistant starch content is increased by chilling: https://www.livestrong.com/article/307427-list-of-foods-that-are-a-resistant-starch/
I haven’t heard much about how chilling affects how food is digested except in the case of Dreamfields pasta, which apparently loses its “special” properties (lower glycemic index/less impact on blood sugar levels) when it has been refrigerated.
Could you comment on whether those of us battling GERD need to worry about refrigerating and eating leftovers of foods that are otherwise low FP. For example, is jasmine rice that has been chilled and reheated more problematic than freshly cooked? Likewise, or maybe conversely, does cooking foods that contain a lot of resistant starch (such as bananas) make them at all easier/harder to digest?
Interested to hear your thoughts. Thanks!
This issue is fully addressed in Fast Tract Digestion CM. I won’t ruin the surprise!
OK, no problem. Can’t have you giving away all your secrets.
I’ll go check the mail again :)
Funny CM. No secrets, just trying to be efficient.
Dear Norm, I came across the reference to your book from Michael Eades site, and what a great find! I have been struggling to get ulcerative proctitis under control for 6 years and I have tried most of the diets that you mention above. I started with paleo 12 months ago, as described by Loren Cordain, but found that I was often tired. I do crossfit and play a lot of golf. I thought perhaps I should get more carbs, so I tried the SCD with no change to symptoms or feelings of tiredness, and then the FODMAPS, which also seemed to make no difference. I also upped the fat content, mainly through increased dairy, although no milk, and I also ate quite a bit of 85% chocolate. The increased fat did seem to make a difference to my experience of tiredness, but not much in terms of UP symptoms. Since I have stopped the chocolate and nuts, as well as many of the fruits you mention (I live in Brisbane, Australia so tropcial fruits tended to be a staple) I find that my symptoms have been negligible. I hope eventually that I will be able to stop also the small dose of mercaptopurine I take daily. Thanks for a diet that seems to work and a wonderful book – I’ve recommended it to my friends who have GERD and I look forward to the future additions on digestive disorders.
Regards, Ruth
Thanks for your story and comments Ruth. Sounds like you are going in a positive direction, just don’t overdue it on the chocolate or tropical fruit.
Hi, I had Roux-en-y gastric bypass in Sept 2004, everything went fine and I have continued to keep the weight off (100 lbs). I’m 5’9″ and 165 lbs (sz 8 or 10) and exercise 4 days a week. About 2 years ago (2011) all the sudden I noticed I was lactose intolerant, I would bloat up like a balloon and have terrible gas if I drank 1 glass of milk. So I gave up lactose for the most part, still would notice terrible bloating and gas a lot so went to surgeon who said it was most likely SIBO as result of surgery and not uncommon. Had breath test at GI and sure enough it was positive so about every 3 months I go on a 2x per day 550mg 10 days of xifaxan which usually bloats me more by day 8 but than it get’s better. My questions are: do you recommend probiotics after xifaxan, if so what kind? New ailment as of 5 months ago is nighttime acid reflux, especially if I’m laying on my stomach, the burning will wake me up – uncomfortable but not painful and not every night. Dr put me on Omeprazole 20 mg to take 1 every morning and I’ve done this for a month and it hasn’t changed anything so I hate to take something everyday if it’s not doing anything, thoughts? Also, considering my gastric bypass my intestines system is different than everyone elses, what diet do you think would work best for me? One more thing, do you believe in having an internal yeast problem? I get frequent UTI’s lately too and on top of all that gyno says I have mild case of Lichen sclerosus, kept thinking I had yeast infection but it’s LS. For 6 years after surgery I was fine, no issue at all with the exception of anemia, now since I have SIBO, all kinds of weird things happening to me…thinning hair, brain fog, extreme bloating, gas, lactose intolerent, rosacea, insomnia, hypothyroid (I’m on 1/2 grain armour) wet cough in the morning for an hour, hands fall asleep easily at night if laying wrong, feet fall asleep if sit to long or especially on fit ball, body odor, increased calluses on my feet, and I smell a weird odor sometimes like stale smoke (like what you used to smell like after going out before the smoking ban), meralgia paraesthetica in right thigh (could be due to Pilates). Feel like a hypercondriac last 2 years when before I went to dr for my yearly physical and that’s it! I just want to have 1 size of clothes cuz when I’m bloated I’m a whole size bigger and it’s depressing. I should keep a food journal and try to determine what bloats me but it’s so inconsistent. Thanks!
Hi,
I can’t speak to all your symptoms but I sure feel for you. The good news is that this condition can absolutely be reversed. An overgrowth of yeast can arise from treating SIBO with antibiotics. The best approach might be to deal with the confirmed issue of SIBO which has connections to so many other problems, some of which you mention like rosacea. I think it would be helpful for you to read Fast Tract Digestion Heartburn which addresses many of the issues you raise including probiotics, antibiotics and specific intolerances. Another good source of information is the next book in the Fast Tract series on IBS coming out soon. This book has a whole chapter on antibiotics. Both books have an extensive chapter on other factors that can promote SIBO. To sum it up, I would recommend the low FP diet in Fast Tract and drop the antibiotics and PPI drugs (consult your own doctor on this) as a first course of action. The Fast Tract Diet approach deprives microbes of fuel they need for overgrowth so it should be just as effective for yeast as it is for bacteria. This is one big advantage over antibiotics. There are many more.
hi, I understand what you’re going through, I have had all of the symptoms that you have mentioned. to naturally treat SIBO you can buy GSE which is Grapefruit Seed Extract, its worth a try. you can buy it on amazon.com for about 15 dollars which includes the shipping. I hope that helps :)
I’ve been on the low FP diet for several weeks now, and although I’ve had a great improvement in GERD symptoms, have stopped using PPIs, and no longer feel the need for antacids, I’m still not feeling well all of the time. I still burp quite often (although they sound more like croaks now).
I have calculated that my FP consumption is only about 25-30g/ day — well within the limits suggested in Fast Tract Digestion. My diet includes: chicken, eggs, lactose-free milk, homemade yogurt, corn flakes, pineapples, cantaloupe, strawberries, jasmine rice, and a few sorts of cooked vegetables — usually potatoes (Russet variety), eggplant, or zucchini.
I’ve noticed that even though I stay within FP guidelines, several of the foods I eat do violate the following guidelines:
Is it possible that these low-FP foods — Russet potatoes, corn flakes, pineapples, and cantaloupe — could still cause me burping and unease? How can they be considered gut-friendly foods if they still contain lots of amylose (in the case of the Russet potato and corn flakes) or lots of fructose (in the case of pineapple and cantaloupe)?
Hi Robert,
Good to hear you are getting into the diet. You might consider cutting back a bit on the lactose-free milk (milk also contains oligosaccharides), corn flakes, potatoes and pineapple. As for potatoes, some have less amylose than others. That’s why I identify some varieties with low amylose and low FP. For fruits, just stick to the FP limits and consume less when in doubt or if you still have symptoms.
Are red and Yukon potatoes ok to eat? I didn’t see them listed in your book but these types, and along with russet, are the only ones available here.
It excites me to have starch again…. With candida and klebsiella, and starch is basicallya big no. Are u sure it is ok with these strains?
Potatoes other than those with solid references for GI results can be tricky. I saw a reference for red skin potatoes having a GI of 58 but haven’t confirmed the result, nor am I sure they are what you are referring to, but if so, that would give a relatively high FP. I can’t find a reference for Yukons. One work around is to get your symptoms under control with foods that have known GIs and FPs and then experiment using the techniques outlined in the book (cooking ripe potatoes well and eating slowly and chewing well, etc.). See if you get symptoms from then while limiting other changes in your diet. Let us know what you learn!
Sorry to be asking so many questions (still waiting for my book to arrive—hopefully Monday!). Could you tell me where rutabagas fall in terms of FP? Are they high, low, medium? I was thinking of making a gratin with parsnips, butternut squash, and rutabaga.
Thanks!
A 2.8 ounce serving of rutabagas has an FP of only 3 grams, so enjoy. Your dish sounds delicious!
Perfect, thanks! Assuming the diet works…let’s collaborate on a cookbook!
I’m only somewhat kidding.
Sounds good Christina – assuming the diet works : )
Dr. Robillard, I recently downloaded your book and found it very interesting. I have been doing an SCD-type of diet for the past year or so. This helped me clear my IBS symptoms (..I had suffered with it for several years). Clearing an H. pylori infection was instrumental too. Yet about two years ago I started to suffer with acid reflux (burning throat, mouth). HCL tablets and TUMS made it survivable but it was hardly an optimal solution. About a month ago I went a low-ish carb diet (perhaps 50 grams/day), mostly by cutting back on fructose, and it has worked wonders. Yet I have been denying myself rice and potatoes for so long I am tempted to reintroduce them into my diet, using the low FP varieties you list in your book.
However, and maybe I’m just too stuck into the SCD mindset, is a chance rice/potatoes could reignite my IBS? That would be nightmare worth avoiding. I would hope the carbs in the low FP rice/potatoes would be digested before any mischief would develop in the lower part of my intestines.
Oh and if I may, one more question. I understand having both IBS and acid reflux is not at all uncommon, especially for someone my age (56). Yet I have seemingly been cured of one problem but not the other. Might this be because bacterial/fungal issues in the lower part of my intestines been cleared out courtesy of SCD and H. pylori eradication but the upper part still has SIBO? Or might the case be we are talking about different bacteria, one that causes IBS and another acid reflux??
Thanks for your help!
Hi Lazza,
Thanks for a couple of great questions. I see your concern with reintroducing rice and potatoes. I would start with the low FP rice varies mentioned in the book as they are more of a sure bet for the absence of resistant starch – amylose. The potatoes are perhaps a bit less black and white as there are so many varieties and all contain some level of resistant starch. You can try them a bit later when you feel your symptoms are fully under control.
Your thoughts on IBS/GERD (SIBO in lower small intestine and even the large intestine – LIBO- might be more likely to bring on IBS symptoms while SIBO in upper small intestine might be more likely to increase GERD symptoms) make sense to me, though I am not aware of proof in this matter.
The best bet is to try the diet for a while keeping FP really low and, based on symptoms improvement, gradually increase FP.
Dr. Roubillard:
Thank you for such a fast and informative response. Yeah, I think trying out low FP rice might be best (I love sticky Asian rice). I can easily be satisfied with rice for a LONG time before attempting potatoes.
And yes, I forgot about LIBO. I suppose years of eating resistant starch is the perfect recipe for LIBO. However it’s somewhat curious that I developed IBS some five years before developing SIBO. But what might have happened is that in my attempt to control IBS my carb intake swung from starchy veggies/grains to fruit, and I can see where I over-indulged on fruit (.. I just love bananas). As your book points out overeating high FP fruit can fuel small intestinal bacteria into a frenzy.
Thanks again. Although I would LOVE to go back to the good old days and eat anything and everything, and maybe that day will come, at least your book points out that one can overcome SIBO and still enjoy some good food. One just has to be mindful FP.
_Lazza
I hear you Lazza. I wish I could eat like I used to too. But I don’t care for the side effects – overweight with chronic heartburn.
How low carb do u recommend to “starve” bad gut bugs? (like percent of cals)?
This is covered in my books Shelby. Putting the bad bugs on a diet can be done with the low FP approach (Fast Tract Digestion) where the number of total daily carbs is irrelevant or by controlling total carbs (Heartburn Cured). On the later approach, a good starting point is less than 25 grams per day then follow the plan.
Dr. Robillard
Thank you again for all of your research and saving me from a Nissen Fundoplication! I was experiencing some strange sounding belches like the individual that commented above. I stuck to the diet, and my belching sounds normal now. I can’t believe it! It took about a month and a half, but sticking to the diet really worked. I sincerely appreciate what you are doing and have recommended your book to several family, friends, and co-workers. Your book should be mandatory reading for anyone suffering from digestive illness. I am not overweight, but have suffered from chronic acid reflux for 2 and a half years. I am 32 years old. My reflux has now completely disappeared. After changing my diet I realized I had been bloated after eating certain carbohydrates for the last 10 years or so. I thought it was normal! Boy was I wrong! haha. My girlfriend first brought it to my attention about 2 years ago when I looked 4 months pregnant after dinner. I am skinny enough that most people never noticed it. I would usually just throw a sweatshirt on after I ate out. I feel stupid for not recognizing the symptoms sooner! I want to tell everyone I know how I feel now. I have read many forums where people are borderline suicidal dealing with reflux and ibs. It really saddens me. I hope more and more people discover your book before they allow doctors to just cut them open. I hope your book changes their lives too. Now that reflux is a thing of the past for me :) I started researching if there is a cure for SIBO. The only symptom I have now is bloating if I stray from my diet. Most websites say there is no cure, while some have indicated a 1 to 3 year period until a person can eat normal again. I was also humoring the idea of only getting my carbs through jasmine rice each day instead of specific, ripe fruit and lactose free ice cream, vegetables etc(because of it’s negative fermentative potential)? I wonder if any research has been done to see how long it would take to starve the bacteria off near completely? Maybe a silly thought…could be that I missed that section in the book, or it could just be that I’m Polish (haha) but…If there isn’t a way to completely cure this condition today, I bet we can’t be that far off?!?!
Hi Joseph,
I am happy to see that the Fast Tract approach gave you such positive results. I don’t think you need to worry about wiping out all your bugs. They’re healthy and useful for digestion as long as they are kept in check in the small intestine. It sounds like yours are.
I typed a “w” instead of an “e”. oops. It’s Joey haha.
I accidentally erased my last comment somehow, so I will give it another shot. Your diet absolutely cured my reflux! I also experienced strange sounding belching as the gentleman described above. I never though it would stop. I stuck with the diet for a month and a half, and now I am back to normal! I am so grateful for my restored health! I have recommended your book to coworkers, friends, and family. I can’t stop talking about it. This book should be mandatory reading from anyone suffering from any digestive problems. I am 32 years old, and not overweight. Chronic reflux started 2 and a half years ago. I researched daily for a cure. Your book saved me from a Nissen Fundoplication. I can’t thank you enough. It saddens me to see people in forums suffering from reflux and ibs sounding near suicidal. I hope they all learn of your book.
2 years ago my girlfriend said I looked 4 months pregnant. I always thought it was normal because I could usually just suck my gut it in or throw on a sweatshirt. Boy, was I wrong. I was skinny enough that no one seemed to notice. Completely cured of my reflux these days :) I only get bloated if I stray from the diet. I get my carbs from green leaf lettuce, some greek yogurt, ripe fruit, and lactose free ice cream, etc. I also really enjoy the jasmine rice. Gastroenterologists feed us pills to treat our symptoms, but don’t address the cause. Your diet truly addresses the cause. I have researched a lot more trying to find out if I will ever be able to eat the same way again. I should say…at least eat some of the things(carbs). Most people say there is no cure, while others say it can take 1 to 3 years to cure this. I have also read that probiotics can help make symptoms better or worse. I have been using Dr. Ohhira’s and think they help. Curious if anyone has ever tried to near-completely starve out the not so friendly gut inhabitants? For example, getting your carbohydrate intake specifically from jasmine rice each day(because of it’s negative fermentative potential)? I wonder if there is in fact a way to cure this stuff permanently by sticking to this type of diet? If there isn’t, we surely can’t be far off?!?! Also curious if the servings of jasmine rice in the book are based on a ‘cooked’ or uncooked serving size? Thank you again for changing my life and for giving me hope.
Hi. Love the ftd book so far and am excited to see if it works for my crabby gut. :-)
Quick questions: a lot of paleo recipes use coconut flour. What’s the fp on this? Also, what is the FP on brown rice protein powder like sun warrior and garden of life? Since most of the starch is removed and it is mostly protein, am I sage to assume that it is in the low Category?
Thanks
In the absence of a glycemic index value (maybe it’s been tested and you can find one online) I would assume an GI = 50. Then calculate FP making sure to add grams of fiber. Below is a reply to another inquiry about coconut flour with some general thoughts on symptom potential.
Below is a reply to another inquiry about coconut flour. On the brown rice protein powder, it’s likely zero if there are not carbs. Check the label so see if carbs are present.
“Great question CM. I have actually been looking into coconut flour. The numbers vary quite a bit as to the amount of fiber in coconut flour but range as high as 60 g fiber per 100 grams of flour. Coconut fiber is also fermentable by gut microbes, but the question is how fermentable? If it’s fermentability is closer to the toughest fiber, cellulose, it might not be too bad, but the amount of fiber is cause for caution. In the absence of more research, I would recommend first getting your symptoms under control with the Fast Tract Low FP approach. Then in a more controlled fashion, try consuming some foods made with coconut flour to see how much you can eat before getting symptoms. Then report back to us!”
Most recipes for pancakes call for approx 2 tablespoons of coconut flour, so is that a safe amount.? Also, some recipes call for like 1TB psyllium as a binder (or chia, but the former seems to work best)
How are psyllium, coconut flour and chia in those amounts and ione sserving of a recipe (2tbs Co flour, 1TB psyllium)?
I recommend doing you best to stay in the FP limits per meal and per day remembering to add the fiber grams. Once you are symptom free, you can experiment in a controlled fashion to add less well characterized foods to see if they invoke symptoms. Chances are, a little psyllium and coconut flour won’ hurt once SIBO is under control as the fiber types in these foods are the least fermentable types of carbs.
What makes a carb less fermentable?
It’s hard to know when sibo is “gone”… Does it ever leave or are some people more prone to it and thus always need to follow a modified diet? Or is it more along the lines of once u have it, u always have it, just in varying degrees dependingon diet and such? That would not be cool.. I want to get rid of it entirely and not have to be so strict with carbs.
Fast Tract Digestion goes into all of these issues. As for your last question, when SIBO is under control, you won’t have to be as strict with your diet, but you will most likely always have the potential to develop SIBO again if you revert to the same behaviors or consume the same foods that led to the problem to begin with, or if you have any of a number of underlying factors / conditions that promote SIBO. These are described in chapter 6.
Also, how can hummus be low fp but chickpeas be high fp? What brand of hummus is usually safest? And Lastly, would homemade hummus be high fp or low?
And was the fps for the legume list on dry, or cooked? How would soaking and/sprouting affect the fp?
Thanks
Notice in the FP tables that the serving size referenced for chick peas is 5 times larger than the serving size for the hummus. That accounts for the difference in FP. Unless specified as “dry”, most FPs are listed for “hydrated” or “prepared” foods. Soaking likely won’t change FP much, but sprouting would. The question to ask is what is happening to the carbs during the process (can you get a net carb number for the sprouted product?), be it sprouting or fermenting, etc.
Sprouting changes the carb into more protein, i believe…. So the longer u sprout, the less fp it would have, right? I wish there was moredata on sprouting
I agree, sprouting takes energy and likely gets that from stored carbs.
Don’t yell at me if this is described in the book… I’m still reading it but I have suggested it to many friends and one asked me this question, which I wanted to ask u before she bought the book, in case it didn’t work for her:v
Does the diet address OTHER pathogens besides just sibo? Many people have other types of gut pathogens besides bacterial, like yeast fungus parasites etc. How would this diet address those types of pathogens… Wouldn’t carbs of any type feed those pathogens, especially the more refined ones that have a low fp bc they digest to sugar more readily?
Thanks
WHAT, YOU DIDN’T READ THE BOOK? Ok, just kidding. The books and site are getting more popular, which is what we want. Now my challenge is to answer as many questions as I can until I enlist another moderator to help, or until more dialog picks up between people who have read the book and people who haven’t.
The concept of both the FP and Low carb approach is to create a condition of more limited gut nutrients to reduce microbe counts overall (including various types of bacteria and yeast). In this state, the human body is more able to work it’s magic to allow the good guys to stay and expel or kill the bad guys. The lower the FP, the more likely the carbs are fully digested entering the blood stream instead of persisting in the intestine.
HAHA..Im in the process fo reading it and am so excited by the concept that Im recommending it to a lot of my friends…however, we are skeptical bc everything out there says NO carbs with candida, klebsiella, and other major bugs, so we are trying to wrap our brains around this theory.
So basically, low FP allows u to eat certain carbs and these carbs will NOT feed yeasts and starch-eating microbes at all?
WOuldn’t food combining need to play into this as well….for instance, eating carbs with meats can cause the carbs to not digest properly or vice versa bc the starch requires a more alakine environment and the pro requires more acidic environment. Also, pro digest slower than carbs and thus can hold up the carb digestion and thus ferment. Any thought on this?
Nothing is absolute. Bacteria and yeast prefer to ferment carbohydrates (different species and strains have different abilities to ferment different carbs), but can also ferment proteins and amino acids. The idea isn’t to truly starve all your microbes, just limit the amount of fermentable material available.
Yes, different foods will affect the digestibility of carbs, but you’re still better off with low FP carbs all other things remaining constant. It sound’s like you are looking to take it to the next level with controlling food mixing -go for it and report back.
Kate, I also think food combination probably plays a significant role our digestion. It seems likely that something as simple as eating fruits as dessert after a carb/protein heavy meal is likely to cause fermentation but it seems like a norm among many people. I know Ayurveda gets into this a bit more.
Hi Norm,
I have been using your book for a few days now, after 5 years of dealing with heartburn. I had a couple questions: 1) What is the best way to wean off of PPI’s while on the diet, and 2) Can I use DGL Licorice while on the diet?
Thank you!
Hi Daniel,
Once on the diet, many people just go cold turkey without symptoms. A more gradual approach is to wean off over a period of two weeks – with your doctor in the loop.
Lastly, I don’t recommend DGL due to the sugar alcohols used in the product.
Wow, thank for the fast response.
After 5 years of constant struggles – I have no idea how its been so long – I’ve finally found an explanation that makes sense. I told all of my Dr’s that it followed a strong course of antibiotics at age 24, but none of them had any insight. I have daily symptoms despite 40MG Prilosec so I doubt I’ll have no symptoms cold-turkey. But I’ve tried many, many things and this is the first that has my unbound optimism.
You are the best Norm. I wish I would have tried this 5 years ago (I know you posted on a GERD forum I write on back then). I know you have helped many selflessly. I have contacted your email for a phone consult and hope to have the opportunity.
Similar question: assuming the DGL is unsweetened capsules rather than the chewable wafers, do you think a small amount of rice flour or cellulose in the tablets (like these: https://www.vitacost.com/productResults.aspx?NttSR=1&ss=1&x=0&y=0&ntk=products&Ntt=DGL%20capsules) poses a problem?
Probably not.
Hi,
Does DGL contain sugar alcohols naturally, or are you referreing to DGL tablets that contain a lot of extra ingredients in addition to DGL? There are brands of DGL that are just pure DGLpowder — wouldn’t that be OK?
Wow, thanks Danial. But the pleasure is all mine. I started as a long term GERD sufferer. My research and writing has been a very pleasurable 7 year journey. Seeing things through a new lens (new theory) is very rewarding. Everything you read looks different.
You might be right. Tapering in your case makes sense.
Thank you.
Is it safe to assume that some people have GERD as a result of something other than SIBO? I am afraid of the cancer risk of GERD, and so I am curious if being off the PPI’s long-term would be a great idea. If someone still had symptoms while off the medication, would you recommend they stay off of it? If 2 months of the Fast Track diet and being off PPI medication didn’t help, would you tell that person to go back on the PPI’s because they might have non-SIBO related GERD? I am just curious.
For those of us focused on esophageal health and using things that are supposed to be good against esophageal cancer, like fish oil pills, turmeric (and mustard), brocolli sprouts, etc., is there anything we may be consuming that we should not while on Fast Track?
Thanks again!
The only reason I can imagine someone having GERD symptoms other than SIBO is having a lower esophageal sphincter that is extremely weak or damaged easily allowing stomach contents to spill into the esophagus. I see SIBO is the driver of acid reflux in every other case. if you still were to have symptoms after being on the Fast Tract diet or other dietary approaches we discuss through DHI counseling, I would no longer advise against PPIs until the symptoms were under better control. But one thing to remember; PPIs don’t stop reflux and do not appear to provide protection against esophageal cancer or lung problems such as asthma and other respiratory complications from GERD.
I finally received the book and have been enjoying reading it and trying to implement the principles in my lower-carb diet. I am still having quite a few symptoms and, beginning today, am trying to measure more carefully how many grams of FP I consume daily. Until now I’d just been eating foods considered lower-FP without really tracking overall consumption.
A few questions I hope you’ll have time for:
1) Any guess as to the FP of plain 24-hr.-fermented/SCD yogurt (https://www.breakingtheviciouscycle.info/legal/detail/homemade-yogurt/)? I make my own yogurt and let it ferment for at least 24 hrs., which theoretically gives the cultures enough time to completely break down all the lactose into simpler sugars. Would the FP be lower than the 7 grams listed for (presumably) commercial yogurt?
I’ve also read that carb counts on even commercial yogurt are slightly misleading because they don’t account for the cultures converting the lactose, but instead measure the carbs in the milk pre-fermentation. (https://www.carbsmart.com/greatyogurt.html) With that in mind, do you think it’s fair to use the 4g carbs/cup of yogurt estimate to recalculate the FP for plain yogurt?
2) In the book and in your post, you mention that lactose-free milk is acceptable. I’ve looked all over the internet trying to find a GI for Lactaid (either 2% or whole), and it doesn’t seem to exist. Do you have an educated guess as to the FP of lactose-free milk? I would guess it’s less than the 8g listed in the book for regular whole or 2% milk. Is lactose-free milk still something heartburn sufferers should try to limit or count toward daily FP targets?
3) Brown rice pasta looks like an attractive occasional alternative to jasmine rice. Do you recall which brand you calculated FP for? I picked up a bag that turns out to have added bran, which strikes me as a no-no considering fiber’s potential fermentation.
4) Most varieties of potatoes available in stores, even organic or specialty stores, are sold unlabeled. Is there a good source for the low-FP potatoes mentioned in the book (Desiree, Pontiac, Sebago)? Also, have you thought about whether aging tubers/potatoes impacts their FP? I’d read somewhere that refrigerating potatoes isn’t generally advised because it encourages them to convert start to sugar—which might actually be beneficial in terms of lowering FP, no? I also heard somewhere that McDonald’s stores their potatoes until the starches convert and they become sweeter, which makes for more addictive fries. Just curious whether this might be a factor to consider, just as we have to think twice about refrigerating cooked starches.
Thank you, and keep up the good work!
Great post Christina,
The student becomes the master. Your questions are amazing. I don’t have all the answers, but I love the questions.
Your thought and link on yogurt is really interesting. I will look into this because wouldn’t it be nice if yogurt was even more gut friendly than we thought.
Lactose-free milk is most definitely lower FP than lactose-containing milk, but I suspect they add sugar back for the same taste. Another mini research project.
On the brown rice pasta and the various types of potatoes, all I can say is that I sourced all my data (for calculation of FP) from the public domain glycemic index tables. I removed many foods due to the fact that they would not be recognized in the US. Still many of the foods in the tables are Australian as much GI work has been done there. Now I will need to rely on well informed curious readers like your self to learn more about the availability of the less well recognized foods in the tables.
This whole idea is new and there is still much to be learned.
Thanks for adding your keen insights!
On the FP tables, I wanted to see if you could clarify….
What is the difference between rice cakes and puffed rice cakes? The only ones I have found are Quaker Oats rice cakes would these be considered puffed rice?
Also, the peanut butter listed doesnt specify whether it is typical peanut butter or natural peanut butter=only ingredient being peanuts. Which one are you referring to?
Also, is the Almond milk on table, sweetened or unsweetened?
I have read your IBS book but need to fine tune the details.
Thanks for your help.
Hi Sherry,
Thanks for reading. Puffed rice cakes are made with “puffed rice”. They look fat and round and very light. Likely the same as the Quaker Oats rice cakes you mentioned. Peanut butters likely won’t vary much in FP since peanuts are the main carb ingredient that registers in the glycemic index test. The almond milk / drink is unsweetened. Good luck with the diet!
Hi CM,
Do you have a link to how you make this yoghurt? Thanks!
Here’s my approximate “recipe”:
Heat 8 cups 2% or whole milk to 180F (just at a simmer) and transfer to a large Tupperware you’ve just cleaned with very hot water and dish soap. Cover with plastic wrap and monitor the temperature until it drops to around 110-115F (you can use ice packs or a water bath under your bowl to cool down the milk more quickly). When the milk reaches 115F, whisk in 2-3 Tbsp. of your favorite yogurt that contains live cultures (I like using Liberte vanilla or Stoneyfield organic). Whisk well. Cover your container with its lid (discard the plastic wrap), wrap it in a towel, and stick it in the oven that you have very briefly preheated to warm it up slightly (like you might for proofing bread dough). Turn the oven light on. Note the time—your yogurt will be ready in 24 hrs. Every 6-8 hrs., if you can remember, it’s helpful to very briefly turn your oven back on just to warm it slightly (just don’t forget or you’ll overheat and kill your yogurt). At the end of 24 hrs. you’ll have a tart, thick yogurt—almost Greek yogurt style. It will also firm up further once you refrigerate it. You can also use a heating pad (I’ve done this using a styrofoam cooler for insulation) instead of the oven.
Thanks! Really appreciate you taking the time to write that out.
No problem. The higher the fat content, the thicker your yogurt will be. If you want to use fat-free milk, you’ll need to whisk about 1 c. of dry milk powder into the hot milk to help augment the thickness—not sure how that might affect the FP (perhaps in a bad way). My normal breakfast is about 1 c. of this yogurt with some sliced strawberries (it’s less sweet than the commercial stuff, but you get used to it).
Also, regarding your other post about heartburn being up and down, that’s definitely been my experience. I don’t think you can assume that whatever you ate immediately prior to symptoms is what caused them (e.g., chicken). The impression I have from the book is that you can sometimes experience symptoms 2 or 3 days out from something you at earlier (which is why the diet has you reintroduce wheat and other potential allergens slowly and separated by several days to monitor for symptoms). You might be able to keep chicken, after all ;)
Does this mean that after some time on the diet that one could eat within an hour of sleeping without heartburn, and not have to sleep on an incline?
That is the goal – get SIBO and reflux under control so there is less intragastric pressure and the LES tension can improve over time. I would keep the technique on your GERD tool belt in case you ever have breakthrough symptoms.
Thanks Norm!
I have weaned from 40mg Prilosec to 20MG Prilosec and am doing much better symptom-wise since starting the diet despite the lower dosage. Although I eat basically the same thing every day, yesterday I did get a lot of heartburn after days of doing very well. I guess it is just how it goes – ups and downs without any real logic, with a long-term trend of improvement.
I did eat chicken, which I thought would be fine, but perhaps the seasonings do come into play and can cause heartburn even if the protein and fat do not. But I will leave chicken out of my diet for a while though and go back to what I’ve been restricting myself to so far.
Thanks!
My chiro just sent me this link. I have been having reflux since October, and off and on for 3+ years. I am celiac and hypothyroid (Hashi’s). I am a vegetarian (since ’76). I am 5’2 and weigh 103#. I am concerned if I cannot eat some of the sweets (mostly pumpkin muffins and other gluten free products). These are made locally, so did not have the stuff that no one should be eating. This might cause more weight loss than I can afford. I have been following an Ayurvedic diet, which excludes brown rice, soy and all nightshades. I have been using Basmati rice which I will change to Jasmine. Since doing the Ayuredic diet, I have had no IBS bowel issues, but do have the reflux. Part of it may be caused by constant back spasms (overuse of computer/work) which impacts the nerves in the esophagus and irritates. I also have a small sliding hiatal hernia. I also use Aloe and DGL and drink lots of water. Any thoughts/suggestions? I did have the breath test for h pylori years ago which was negative. Thank you for your time.
Hi Marty,
If you need to add some sweets you can prepare them with Splenda, dextrose or even maltose, though I would watch the latter two until your symptoms are under control. One of the problems with gluten free diets is that they have too much resistant starch because they only limit starches from wheat, barley and rye. Many celiacs therefor are consuming too much resistant starch in the form of corn, certain potatoes and rices and even bananas. I would stop the DGL as most brands contain sugar alcohols.
If you would like more specific help with what to eat, feel free to drop us a line under the counseling tab.
Thanks for your reply. I do not eat corn products, except polenta at times, no bananas. I eat Jasmine rice, no potatoes, except sweet potatoes. Having been a baker most of my life, I found making gluten free to challenging and never tasted as I remember those receipes tasting, so I no longer bake, so that creates problems with the “sweets”. The DGL that I use is Fructose Free and Sugarless. I will look where you directed me. I believe Gluten Free diets are not healthy. Choices are limited though better than 8 years ago. You have to read labels really carefully.
when will your hardcover IBS be available. Will that have the list of foods and there fermentability? I am curious about garlic and onions on this plan. These are major triggers for me.
The print book is scheduled for release by the end of April. The book will have FP tables that include garlic and onions.
How do purple potatoes, Yukon potatoes, and jewel and garnet yams fall in the fp?
Sorry Kate. I don’t have info on the specifics of these potato varieties at the moment. For the time being, you could look up the carb counts and assume a glycemic index (unless someone tested these foods) of 48 (conservative for potatoes based on sweet potatoes). That will allow you to calculate a rough FP. Remember, there are potato choices with known lower FPs such as Pontiac, Sebago or Russet.
thanks, am looking forward to that.
Hi. I just took antibiotics for sibo. I’m overwhelmed knowing that I have to drastically change my diet. In the past few months I’ve been eating cookies, scones at Starbucks, big bowls of oatmeal, etc. Now it seems like I have to eat meats and some veggies or just starve. Here’s my questions:
1) is there any kind of oatmeal or wheat bran or some type of grain I can eat a lot of by simply adding hot water and honey? I don’t like cooking
2) what kind of sweetener is ok for my coffee? Splenda, stevia, organic raw honey or what?
3) have you tried that new sweetener made by Splenda, which is mostly monk fruit? Is it safe for sebo?
Thanks for your time. I am going to get the book people keep mentioning in these posts
I hear you Joe. We all wish we could eat like we did as teenagers. But I think you will be surprised by the recipes in the Fast Tract Digestion books. For instance, the sticky rice cereal is easy to make, delicious and creamy, and you can sweeten either with Splenda, dextrose or even maltose (better not to use honey). I have not tried this new Splenda sweetener based on monk fruit, but I am very curious now that you mention it.
Hi… I’m not sure if this has been addressed, but does the “fast tract digestion” diet help with yeast/fungal/mold overgrowth and parasites in the gut? I had a recent Metametrix stool test that showed these results. There are many variations of the “anti candida diet”… Some say that brown rice, starchy veg, and even some fruits and beans are ok… Other limit just some of those foods or are very strict and promote lots of meats eggs veg and fats.
How low carb and fp would be beneficial for me to go? How high fat? Are there any particular foods I should avoid based on these infections?
Lastly, do u feel that the natural antimicrobials like oil of oregano and grapefruit seed extract are helpful? Probiotics?
Thanks for being such a great resource
Hi Kyra,
I can’t give you a very detailed answer with out more information about your situation, but here are a few thoughts. The Fast Tract Diet limits the amount of (carbohydrate) fuel that supports the growth of all intestinal microorganisms including yeast and other fungi as well as many parasites. In your case, knowing what specific organisms are causing the problem would be very helpful. Parasitic microorganisms can be tough to get rid of because they have well developed virulence factors that allow them to attach, feed and reproduce in the digestive tract. Many of these specific parasites or fungi may require powerful antiparasitic or antifungal drugs to dislodge them.
If you choose to try the general approach of “starving them out”, you can’t go too low on carbs or too low on Fermentation potential. I would focus more on limiting carbs than fats or proteins. You should avoid high carb or high FP foods. I don’t think the herbs and extracts will be of much help in your case, but that’s just my opinion. In the case of probiotics, it wouldn’t hurt to try it.
I recommend you discuss any ideas on this site with your own health care provider to arrive at a comprehensive diagnostic and treatment strategy tailored to your specific situation.
Thanks norm!!!
I wish i knew the strains. The test couldn’t id them, but my yeast/fungus level was the highest possible at 4+. I have bad uc and gerd. Low carb is hard for me bc i get constipation, which flares the uc. I’ve been trying to go low carb the last few days (no fruits only some squash, peas, and veg for carbs… Eggs, chicken/fish for pro… Coconut oil for fat) but it’s caused my stools to become gluey/tarry and constipated with some incontience (sorry for the tmi) … I’m also craving fruit badly and i dont feel satiated.
Any advice, based on what I wrote above?
What would be a good general macronutrient ratio? I’m not used to eating low carb, so idk how low my grams/percent should be, nor hw high fat.
Lastly, any tips to prevent these sticky stools and constipation?
Don’t worry, never tmi on this site. Your diet sounds pretty reasonable. Fast Tract Digestion IBS- coming soon- has lots of information on constipation including a detailed section on the four basic types of laxative. Here are a few suggestions. Go on the Fast Tract Diet because constipation has been linked to a particular type of SIBO. Loose the legumes which can make matters worse. Add more green leafy veggies. Drink lots of water. Consume more olive oil. If you use laxatives, don’t over do it as that can create a dependency. Antacids and some pain medicines such as Tylenol 1, 2, 3 and 4, which contain codeine, can cause constipation. I don’t worry about macronutrient ratios because there are so many low carb vegetables and I eat plenty of fat and protein.
Cant wait for the book to come out!!! :)
I’m not eating legumes…. Aren’t green peas a veggie? I would be really sad to cut them out bc i make a good sauce with them. It’s the only way I can tolerate meat (i am normally a vegetarian)
I don’t use any meds. I am trying hcl and digestive enzynes. But Idk if these are making things worse?
I’m all about the natural aporoach
I worry abt macros bc i want to eat balanced.
Also, I’m getting hypoglycemic and feel “imbalanced” eating low carb. So, having macronutrient parameters helps. Any advice on the physical symptoms?
Yes, peas are a legume, but not quite as symptom provoking as beans. A 2.8 ounce serving has an FP value of 8 grams. Just keep daily FP grams under 40 (25-30 might be even better if your symptoms are persistent).
The enzymes should be OK to try. I wouldn’t recommend the HCl unless you are over 50 years old or have had a test showing you have low acid.
On low carb, the human body easily adjusts making blood sugar from protein. Hypoglycemia should not be an issue. But the Fast Tract Diet is flexible for people who want more carbs. Just focus on reducing high FP carbs.
Thanks so much norm… U are more helpful than any practitioner I’ve seen
I read in another post regarding someone with candida and how u said that refined carbs won’t feed candida as easily as whole/natural carbs. Can u explain this bc my understanding was that yeast thrives off of refined grains/sugars moreso than refined ones
Lastly, what would then approximate fp be for this product?
https://www.foodforlife.com/product/tortillas/brown-rice-tortillas
And would it be “safe” to eat daily for someone with my gut infection?
Ps, imI’m also prone to klebsiella pneumoniae…. It is supposedly gone now, but i dont want that bugger to come back!!
Yeast would love to consume refined carbs, but these are also the carbs preferentially absorbed leaving few available for yeast or other gut microbes. The brown rice tortillas have an estimated FP of about 12 grams. BTW, K. pneumonia overgrowth responds favorably to low starch (Dr. Alan Ebringer’s work) and should respond even more to low FP.
Speaking of candida and yeast, isn’t it important to go on a low sulfur diet if u have candida bc sulfur feed the yeast (and can also be bad if u have mercury toxicities)?
How would a person do a low fp, anti candida, low sulfur diet?
I have also read a few posts about low sulfur for Candida. I don’t understand this approach as sulfur-containing compounds inhibit yeast so foods such as garlic and onions are recommended because they contain sulfur compounds. Just don’t eat too much garlic and onion because they also contain difficult to digest but easy to ferment fructose oligosaccharides. The best overall approach is low FP, low carb, low starch type diets while addressing any existing immune system deficiency that can allow yeast (Candida) to become established. Also avoid antibiotics, hormone treatments and other drugs that can promote yeast overgrowth wherever possible. It might not hurt to try a probiotic containing Lactobacillus acidophilus though there is little information on the effectiveness of this approach.
Mercury toxicity is a much more serious condition that goes way beyond candida overgrowth.
Dear Norm,
First of all I would like to express my deep gratitude for your great insights and research! I got an electronic version of your book through Amazon, read it the same day and was ecstatic to find something that actually explained the problem behind GERD and presenting such a brilliant solution for it!
I have been experiencing severe GERD symptoms for about 3 months, it started abruptly and seemed to never end. By the end of the 3d month, my esophagus was so bad that I had trouble breathing.
My physician put me on PPI and told me that my problem was weak LES and that it was genetic. I felt so hopeless. I then discovered a Candida diet and tried a strict candida diet for 4 days. I ate exclusively vegetables (onion, cauliflower, broccoli, kale, artichoke) and eggs for those 4 days, my vegetable portion was quite low (about 150 grams per meal 3 times a day). I had a horrible acid reflux all those 4 days. The worst one was after dinner of one boiled artichoke and one boiled egg.
I discovered your book and eliminated all veggies (all fiber) and instantly within a day felt like a human being again. I have been on your diet for 3 days now and have not had a single acid reflux episode!! It is just like a miracle!
I do have a couple of questions for you though
1. On a diet of just veggies and eggs I had a bad heartburn still, although the FP of those veggies was not great. I probably was having FP of about 10 per day. My question is, are there certain vegetables that are not very safe to eat with SIBO even if they have low FP?
2. I have heard of ways of lowering GI of a meal or food by adding vinegar, fat or eating it with protein. Rice for sushi is always seasoned with vinegar for example; I always put butter or ghee in my rice and often eat it with protein of some kind. Does that mean that the FP of a meal gets higher in this case with GI being lower?
Thank you so much for you work and for your time!!
Olga
Hi Olga,
I really appreciate your comments. I like the way you embrace the scientific approach and question everything. I am not sure why your last diet did not work, despite the fact that the veggies were of the low FP variety. But I am glad the Fast Tract Diet is working. I can comment on one thing. Even though eggs have zero FP by definition and overall appear to be a very safe food for heartburn, once in a great while, I get heartburn after eating them. I can’t explain it except perhaps relating it to a slowly fermentable fiber that I may have consumed the previous day. When I assess which foods may have caused my very infrequent reflux, I look back for the last full 24 hours to see if I can identify foods that may have contributed.
Also, you bring up a good point about the affect of vinegar, fats of protein. While some foods will lower the GI (and hence raise the FP) of other foods, the FP system just compares foods to one another without adjusting for these affects. I figure if you start with the safest foods, even some influence from things like vinegar, fats and proteins on the FP will be less significant compared to high FP foods. I recommend using your observation as an additional tool to pull out when and if you have any breakthrough symptoms.
May I chime in?
Olga, are u still eating eggs or did u cut them out? What exactly is ur diet like now?
The diet u ate was very high sukfur. Some people have a genetic sulfur clearance issue with the cbs gene. If so, then a low sukfur/thiol diet would suit u best until u clear this pathway. Supps like molybdenum can help, but only take small doses, like 30mg. Test ur sulfate level with quantofix sulfur strip. It should be <400. As u clear sulfur, ur levels may rise very high, but if u stick to a low thiol/sulfur diet and use the molybdenum, it should clear in approx 10wks. Addingyucca and bbutyrate supps can help clear excess ammonia too,which often goes hand in hand wwith cbs issues. Sprinkle yucca capsules over any food that has animal pro (1/3-1/2cap)
Sulfur is essential to live, so don't go completely sulfur free… But u may need to watch ur intake for a short while. Bad gut hugs can influence this sukfur intolerance issue, and if u have other genetic polymorphisms (snps), these might influence ur ability to methylated, detox, and tolerate certain foods
Hope this helps
Dear Amy,
Thank you so much for you input!
I do still eat eggs on this diet, about 2-3 a day and since I eliminated all veggies I have not had an incident of heartburn which tells me that my reaction while on Candida diet was probably to fiber in vegetables. Of course by eliminating sulfur containing veggies I did cut down on sulfur a bit but I still do not think that I have a sulfur issue also due to the fact that ironically, about 4-5 days ago I also started to take organic sulfur crystals(after reading about importance of sulfur for detoxing), about 4 gr per day dissolved in water and Alpha lipoic acid(both rich in thiols) and I have not noticed any worsening of my symptoms and still have not had a bad reaction. Or maybe there has not passed enough time yet and all the hell will fall on me in two or three days? I hope not.
I am curious though about this issue and would like to test myself for my sulfate level. Where can one get quantofix sulfur strips? Also, is this condition genetic or it can also develop with age? I used to have no trouble with sulfur rich foods before, at least I thought so
As for my diet I try to take it slow and eat mostly animal protein, animal fats and a little bit of sticky rice. I am cautious to introduce anything else at this point since the diet I am on is working now. I will be introducing other things gradually in the future and see what my reaction is. Sulfur issue is definitely worth exploring more which what I will definitely do.
Thank you very much for your advice and new insight into my problem
U can get ur genes tested thru 23andme. Cbs is a gene that can make people sensitive to sulfur if it is activated. Taking small doses of molybdenum can help (like 30mcg and working up), in addition to avoiding foods that cause issues (look up foods high in thiols).
Hope this helps. Sorry for the delay
I wonder if the occasional problem with eggs could be related to what the egg-laying chicken has been fed. If the chicken was fed GMO soy and corn, I suspect her egg could be problematic, whereas an egg from a hen allowed to eat free-range might not cause any issues.
Norm, I found you from your interview on oneradionetwork.com. Thanks for being on that show.
Hi Lynn,
Thanks for catching the show. On eggs you never know. I recently was having almost immediate diarrhea right after eating eggs. But (like an idiot?) thought that if I hard boiled them they might not make me sick. When I put them in a pan of water, they all bobbed in the water – full of gas, a sure indication that they had become contaminated with bacteria. I bought new eggs which sank to the bottom of the pan and the problem was solved.
Dear Norm,
Thank you so much for your quick response! I absolutely agree with you , sometimes something that has been eaten a while ago may still have an effect and one should always examine the foods consumed at least within 24 hour period. I used to get bad heartburn in the mornings after drinking a glass of water on an empty stomach. I even told my doctor that I had heartburn from everything even water.
I think in my case I should be careful with eating any vegetables even low FP ones. Apparently bacteria in my gut love vegetables even more than I do.
I have not had any problems with eggs before, although I did stumble upon an article about egg whites being difficult to digest by people with compromised digestion, due to having protein inhibitors and anti nutrients in them. https://paleodietlifestyle.com/an-egg-yolk-a-day-keeps-the-doctor-away/
The author of this article also writes about nightshades and them being not so great for people with gut problems. https://paleodietlifestyle.com/you-and-your-gut-flora/
I used to eat tons of nightshade veggies because I love them but now I feel very cautious about trying to eat them again. I am curious about your thoughts on nightshade vegetables. I wonder if any of your patients ever had bad reaction to them.
Thank you so much for your time and expertise!
Olga
I’ve purchased your book and am so excited — dietary recommendations for my “IBS” that finally make sense! Thank you… this will be well-recommended to a number of people I know who are suffering. I had a couple questions I was wondering if you’d be able to give your thoughts on…
I’ve been spending a year and half with unexplained digestive issues — after trying to quit smoking and getting *badly* backed up while being under a lot of other stress. The primary issue is extreme gas, which has been continuing to build and build. My intestines fill with gas 24/7 at this point. Every hour (sometimes every 10 minutes) I’m forced to assume uncomfortable positions to emit extreme volumes of gas, sometimes it’ll trap terribly, while other times I’ll be attacked by an hour+ of huge, violent, swaths of non-stop gas and still be left bloated & constantly gassy afterwards. It’s not as if I’m intolerant to anything specific, severely constipated, or eating an extreme amount of carbohydrates or fiber. I am already underweight, and a high school teacher, and have not been able to cut out carbs completely, however. Other than that I’ve tried it all from fiber therapy to probiotics to FODMAPS (though definitely still too much sugar, and moreso resistant starch & fiber methinks…) and have had every test done on me. Tested negative for SIBO but know false negatives are common, and figure my problems lie farther down the tract as I suffer no real upper GI complaints. Currently ‘fighting candida’ with a naturopath. Had a comprehensive stool analysis done that showed “friendly” +3 bacteroides fragilis +3 e coli, +2 bifido, +1 lacto / “commensal” +1 of klebsiella pneumoniae ssp pneumoniae , +1 Gamme hemolytic strep, +1 alpha hemolytic strep / “yeast” candida +2 / and then the “potential parasite” blastocystis. I don’t know how accurate/informative any of that is. Blastocystis has shown up before and docs have offered to give me Flagyl, with the caveat that it would likely make my situation worse. Is the culprit of this extreme flatulence a general overgrowth, the wrong bacteria, blastocystis, or some unfound parasite?? Thoughts?
I’ve purchased your book & have started following the diet… but obviously with the extent of my gas despite previous dietary experimentation, things won’t resolve overnight. The gas has become so extremely horrible and controlling that I am becoming severely depressed. Now both my naturopath and GP say I should give Flagyl (250mg TID) a try. I’m worried it could result in making the candida thrive, and possibly the klebsiella or blastocystis as well (to eliminate blasto they usually prescribe 3 times as much), or maybe even c.diff :o? I feel good in terms of elimination, there’s no odor to speak of, and I worry about making things worse than they already are. I can’t remember ever having taken antibiotics before. That said, I’m in pain all day, unable to sleep, and barely holding onto my job. Any advice at all on whether to take the antibiotics and use the diet during/after, or to focus on pushing myself diet wise, i.e. carb elimination? Any thoughts would be awesome… I’m a bit lost!
Also, the more fiber I cut the more constipated I seem to become… quite a catch-22 in my current situation. What’s worse in terms of feeding those buggers… constipation or fiber? Any recommendations there? (I had a transit time test & everything was moving fine– while I was intaking a ~22g of fiber a day & GASSSy– and worry that I’ll be compounding the situation by getting constipated again.) Any thoughts on enemas/colonics?
Thanks a ton. I know there aren’t any easy answers to any of my questions… but I really love the book & you seem to be one of the wisest individuals I’ve come across in terms of your digestive advice
Oops… forgot: -NG Eneterococcus spp. // +2 Clostridium spp….. :)
And how reliable/informative are these stool tests anyway?
I assuming you mean that the test (no growth) was negative for Enterococcus species and positive for 2 Clostridium species. I would not worry about the results unless specific pathogenic (disease-causing) organisms are present. Both Enterococcus and Clostridium species are normal parts of most people intestinal flora. If you were positive for C. diff, that would be a red flag.
Hi Jon, blastocystis is weakened by the enzymes lipase and serrapeptase. Lipase dissolves the fatty cell walls of the blastocystis so the agent you are using to treat the blastocystis can penetrate to the organism and work more effectively. Serrapeptase is an enzyme which dissolves non-living matter in the body, so will dissolve the biofilm which the blastocystis coats the intestines with. Incidentally, serrapeptase also treats candida.
Hi Jon and thanks for writing. Based on the information you provide, I suspect you are experiencing a general dysbiosis, as you suspected – an imbalance in gut microbes likely involving the latter part of the small intestine and large intestine. For some reason your diet is feeding this dysbiosis. I recommend following the Fast Tract Diet and drinking lots of water. If you are worried about constipation read the two sections dealing with this topic. Make sure you have salad and lots of olive oil daily.
Of course consult your own doctor, but I do not recommend taking any other drugs, probiotics, antibiotics, colonics or enemas until you give the Fast Tract approach a chance. As far as stool analysis, more information can’t hurt. You could find out that you have a specific pathogenic organism present, etc. But first give the diet a try. You should know straight away if it’s going to help. We offer coaching if you need some concentrated help on your specific situation.
Dr. Robillard,
Just going over your book on IBS and SIBO, and had a few questions about the dietary recommendations. Can you help me make sense of these? I saw that brown rice has a high FP, but brown rice pasta is low? Similarly, rice crackers are low, but I assumed this to mean white rice crackers, not brown? Can you clarify? Also, I saw that a corn muffin was listed as low FP. Does this mean making baked items from cornmeal would also be low FP? One last thing, not sure how much luck I will have finding the varieties of potato you mention as low FP (Desiree or Pontiac). Any other low FP types of potato?
Thanks so much! Really enjoying the book!
Andy
Hi Andy,
Good questions. There are several varieties of brown rice listed with FPs between 8-19 grams for a 5.3 ounce serving. The brown rice pasta does have a lower FP of 5 grams for a similar serving size. I can’t say whether this is due to the manufacturing process or inherent in the type of rice used. I just don’t have that information. The rice crackers have an FP of 2 grams per 1 ounce serving. If you multiply that by 5 for a similar serving size as that reported for rice in the tables, you get 10 g (similar to some varieties of rice). Again, I don’t know what the type of rice was used to make the crackers. The corn muffin with a low FP is listed as a “low amylose” corn muffin which explains the low FP. To duplicate this low FP muffin, you would need to acquire some low amylose flour. If you find some, please let me know where you found it! Lastly, I can’t help you find these varieties of potatoes. I suggest you do the best you can to find some of the lower FP potato varieties, cook them well and consume them in a controlled manner to identify a variety you can tolerate.
Hi.im a french canadien And im not good in english but i like so much your web site. I have a diagnostic of sibo since 2 weeks. Before That, a lot of doctor said That it was just stress And That i CAN eat everything. I start antibiotic (cipro and metronidazole because we cant take rifaxin in Canada)but i Will Try That just one Time. i buy your book. I Will Try to understand all the Words in english! I Will probably have some questions for you!
Hi Val, Thanks for writing. Check with your doctor, but I recommend that you try the Fast Tract Diet first, before you take antibiotics (Cipro and Metronidazole). You don’t want to kill your good bacteria!
I agree with norm… Avoid antibiotics. Especially the flurorquinolones like cipro. They can cause longterm damage… I’m living proof of it. I’m a nurse and the dangers of flurorquinolones are too great to justify their usage, unless in dire, life or death situations. Try dietary, herbals, and probiotics and fermented foods before using cipro
Thanks for your reply. Its stress me because a already start for 5 days but now i dont have secondary effects. My doctor gave me That because i lost Weight because i lost lipid. So Maby he thinks That it was urgent to kill the bacteriA!. But its the first Time That i take antibiotic during all m’y Life. Its scares me That you think That its so dangerous!
And i just Want to sais That probiotic makes me realy worst so i just Want to said to take care with probiotics but it Maby help some person . But herbal and the dietary Yess i Will do and Try to do the best That i can but it Will be difficult in restaurant.
I dont mean to scare u, and it does sound like u need the cipro if ur symptoms are so severe
Just make sure to do plenty of joint strengthening exercises (start low and slow) once u feel better, as cipro can affect the joints of some people. I hope ur gut gets better asap :)
I will follow your Advice when i Will have more energy to do exercises. :). I hope i Will have more energy one day!.i Will write my evolution here after the antibiotic and a diet if you Want!.i hope That the good bacteriA Will be able to coming back without probiotics.
Hi Val,
Don’t worry too much about Candida. Please do post on your progress.
Where i live, nobody believe That candida is a problem in bowel and i don’t believe in That to. Should i believe in candida ??
Thanks Norm, i Will post on m’y progress. what do you think about taking grapefruit seed extract with the diet in the beggining?
Oil of oregano is better. Gfse has a toxin in it that can cause side effects. Your stool test should show what supplements to take
Val, I would beware of this product as there have been many adulterated (with chemical preservatives) grapefruit seed extract products found on the market. The pure product reportedly does not contain antimicrobial compounds as claimed by marketers of this product.
Hello, I hope this question has not been asked already. I am wanting to make an extra amount of sticky rice to have in the fridge to use for the next day, as I am trying to portion my carbs out. Will the rice become resistant starch the next day after heating up again? Thanks in advance for any answers.
Angela
Hi Angela,
A good approach is to wrap one half cup portions of rice air tight in plastic wrap while its still warm being careful not to squish or mash it. You want it to stay fluffy. Then refrigerate or freeze it. You can microwave it in the plastic wrap before eating. Be sure to reheat well to reduce any resistant starch tha may have formed during storage. Use the prodigestion behaviors discussed in the Fast Tract books to help minimize starch malabsorption.
If you have symptoms from eating reheated rice, I recommend going back to freshly prepared rice or reducing the serving size. Once symptoms subside, you could try again.
Thanks Norm! Much appreciate the info. God bless.
Angela
Hi Norm and thanks,
I learned a lot from your view about resistant starch. I had problem with basmati rice especially when it is cold or even reheated and i didn’t know it. I think it’s good that i buy your book about ibs in future. (I have IBS.)
question: I wonder how watermelon can be a safe fruit, because watermelon has a lot of fructose and (fructose/glucose) ratio is bigger than 1 and has polyol. In fodmap diet this fruit is forbidden.
forgive me about mistakes in writing in english. (I am Iranian)
Hi Afshin,
I am glad you liked the resistant starch article. As described in my books watermelon has a relatively low FP (based both on it’s relatively high GI). That means that the fructose levels are likely not as high as you may think. Also, the FODMAP diet is qualitative, while the Fast tract diet is quantitative. I did not include a value for polyol or sugar alcohol in the FP table for watermelon because I didn’t have any value for this content. Can you provide a source for the amount of polyol? If significant, I will revisit the table and update if needed.
Your book has been a godsend since I was diagnosed with H Pylori and then SIBO. I am much better than I was by following your diet. Since I had the SIBO and was nauseated a fair amount of the time, I ended up losing weight (I am under 100 pounds). Occasionally I drink Ensure Clear. Can you tell me if this is okay to drink or what the FP is on this (I only drink at most once a day)? Thank you again.
Hi Kim and glad you liked the book. Ensure Clear (10 ounce serving) has 35 grams net carbs of which 18 grams are sugar. I estimate the FP value at approximately 14-16 grams. You might consider cutting the serving size in half or trying a different product.
Kim, u could try making ur own nutritional shake for easy to absorb cals…..
Raw organic whey protein (healthy plant makes one)
Coconut oil
Based in coconut water, almond milk, coconut milk
U can add dates for carbs (low fp fruit, but high cals)
Rice protein powder might be worth considering too, as I know some can’t do whey…
Or Kim, if fat is bothering you (Ensure Clear is fat free), try making some kind of drink using dextrose?
Dr. Robillard, Compared to others I feel very lucky since my only real complaint is the nausea that I still get on occasion. I will stop drinking the Ensure Clear and see if I can make some other type of nutrional drink. I know I need the calories so that is why I tried it. I keep reading about low stomach acid. Would that cause nausea? I sincerely appreciate all of the help!
Kim,
I think the chances are slim that low stomach acid is causing your nausea. I can’t speculate on the cause without investigating your specific situation. Please feel free to contact the institute if the problem persists.
Thank you. I may be calling for a consulation. Thanks again!
I was wondering if anyone has ever heard of digestive enzymes (Now brand Super enzymes) causing massive bloat and pain. Tried them yesterday and could not sleep all night because the burning bloat. And it has not gotten any better. All my food was fine, no changes other than one enzyme with each meal yesterday. Pain and bloat came on half an hour after taking the enzyme each meal. I am ready to stop them and I bought 2 bottles. Please if someone knows anything let me know!
Bloating is often linked to probiotics as opposed to digestive enzymes, but the burning is likely due to the betaine in the product. I recommend evaluating carefully if you even have a need for this supplement.
I am thrilled to have found your site doing a google search for amylose/Specific Carbohydrate Diet. I was confused at Elaine Gottschall’s position on this.
I have since purchased your book and am getting so much out of it. Thank you.
I do have a question I am hoping you can clarify… It was my confusion regarding amylose vs. amylopectin that lead me to this site. My research showed that amylopectin is the starch that is easily digested and this is confirmed in your research. The only place I found an alternate position was with Elaine Gottschall. However, I have since stumbled onto the research of Dr. Ebringer who says that it is amylopectin that feeds the organism that causes Crohn’s and ankylosing spondylitis.
I’m perlexed!
A quote from his book Ankylosing Spondylitis and Klebsiella states: “Amylose is a linear polymer consisting of α-(1→4) links between glucose residues and these can be readily hydrolysed by amylases present in digestive enzymes. Amylopectin, however, is a branched polymer consisting of linear sequences of amylose like chains linked by α-(1→6) side chain giving rise to a branched structure. The problem is that digestive enzymes cannot break down the α-(1→6) links present in amylopectin… ending up with a “hard starch”… which is available for the growth and propagation of gut bacteria…”
This seems to parallel the position of Elaine Gottschall. In looking a little further into this I found an anecdotal claim stating “…deprivation of amylopectin starch can cause the disease (AS) to go into remission. In my case, my blood values are all back to normal.” However I have found similar claims from Ankylosing Spondylitis suffers that have limited AMYLOSE and relied on AMYLOPECTIN starch. Confusing!
Most research shows that Amylopectin is more easily digested. Your theory of applying the GI is brilliant and shows that indeed, amylopectin starch is more easily digested. What gives with the above research?! And how odd that followers of both camps are having success??
Hi Lana,
Good work researching this issue. I have become pen-pals with Dr. Ebringer over the years. His research findings on AS are absolutely outstanding. We only disagree on this one point. I think he learned about starches from Elaine. Amylose is most definitely the one that is difficult to digest. There is no question.
Hi Norm,
Thanks so much for your confirmation. It certainly makes sense.
I will share a few food items that I have discovered…
The first is sweet rice flour – this flour is made with sticky rice. When used on it’s own, the texture of baked goods is rather moist and dense. I’m going to play around with additions to alter the texture a little. That being said, I think it will work really well for some items – shortbread cookies, brownies., pastry. It’s a great thickener as well.
Like sticky rice, it is pretty much 100% amylopectin.
The other item is similar. It is a Japanese rice cake made by cooking and pounding a sticky rice called mochigome which is characterized by its lack of amylose. “The protein concentration of the rice is a bit higher than normal short-grain rice and the two also differ in amylose content. In mochi rice, the amylose content is negligible which results in the soft gel consistency of mochi.” https://en.wikipedia.org/wiki/Mochi
Here’s a cute YouTube video of how to make mochi pizza. I’d nix the ketchup (yuck!) and use a real pizza sauce https://www.youtube.com/watch?v=e59erF1YiFA
You’re so industrious Lana. I hope you come up with some good recipes. One word of caution though. We just returned from two weeks in Japan and I understand that mochi is not actually made from sticky rice. Apparently, there is a mochi variety of rice. Here is a link stating a lower GI for mochi rice balls https://www.glycemicindex.com/foodSearch.php?num=1931&ak=detail. I have not been able to confirm the amylose/amylopectin ratio. Perhaps you will find something.
Just watched the video and can’t wait to try it! https://www.youtube.com/watch?v=e59erF1YiFA
Lana, can you share what brand of sweet rice flour you use? I just found all of your great information and dialogue with Dr. Robillard. Thanks!
Hello Barbara,
I must have heard you calling me! For some reason I decided to re-read this blog post :)
My Sweet Rice Flour is just a bulk product that I purchase at my local health food store. I have tried Bob’s Red Mill Sweet Rice Flour and found it the same as the bulk product.
I searched high and low for an organic product – but no such thing as far as I could find. If anyone finds one – I’d love to know about it.
Good luck with the diet Barbara.
Hi Norm,
Industrious :) That’s my food science background… I was a Home Ec teacher in a former life.
Yes, Mochi is made from Mochigome rice. This rice is a type of sticky rice. At one point in the pizza video, when he’s eating it, there’s a long strand of what looks like melted cheese. He points at it and says ‘Mochi!’
Here’s an article on Insulin and Glucose responses to different rice. They state that Mochi gome rice has 0% amylose and 100% amylopectin. The insulin response is as expected for this rice. https://ajcn.nutrition.org/content/39/3/388.full.pdf
I wonder if the GI for the Mochi Rice Balls was skewed due to other ingredients? When I did a google search for Mochi Rice Balls it seemed to highlight different recipes – some sweet, some savory. Maybe that’s what they were testing? It doesn’t seem right for this type of rice. When you were in Japan, were you told that Mochi isn’t made from Mochigome rice? I’m going to try to get down to our Japanese food store today to see if they carry this. I haven’t tried it yet. I’ll see what the ingredient list looks like!
In Japan, they just said “it wasn’t regular sticky rice, i.e., sushi rice” but I have now confirmed that you are correct, it’s called mochigome rice (in Japanese, mochi means rice cake and gome means rice). However, I had not been able to confirm the amylose/amylopectin ratio or GI. I really appreciate your research into this matter. I wonder if there is sufficient data in that paper you cited to calculate the actual GI?
I have eaten mochico fried chicken made with mochico (flour made from mochigome rice) that was delicious – and did not lead to symptoms, but i was unsure about amylopectin/amylose content of GI, so was concerned with publishing on it. Your research has encouraged us to experiment more with this flour.
Thanks again, and keep up the great work!
Glad the research was useful. I’m making fried fish using sweet rice flour tonight. Even those without issues say it’s a superior flour for this purpose. Looking forward to trying it!
Norm, I’m new at this and am very leary to eat out in restaurants. Any tips in that regard?
We are doing the same but with chicken.. We should compare notes later. It can be a challenge at restaurants for sure. I find that most restaurants are willing to make you what you want so I often times give that a try. Rib eye steak loaded with sauteed mushrooms and veggies is a favorite. Other common dishes include broiled seafood or mixed skewers over jasmine rice. Antipasto salad is one of my go to dishes as is a Greek salad with either grilled chicken or gyro meat on top. And of course you can eat at a sushi restaurant and eat most of the foods with the except udon noodles. Also vermicelli (hard to know if wheat is used) and not sure if soba noodles are low FP either.
I wonder where we could get a hold of these potatoes?!
https://www.avebe.com/News/DiscoverELIANE/tabid/1110/Default.aspx
Had to postpone fish to tonight. Will let you know how it turns out. Hope the chicken was good!
By the way, thanks for the dining out tips – they’re helpful. Our favorite cuisines are East Indian and Chinese. I’ll have to decipher the typical sauces and see how they pan out.
Good find. The US distributor is Ingredion. I sent for a sample. I may need your advice for some baked goods.
We actually went out last night so didn’t make the chicken. We ate Indian, including basmati rice. I had to use some proabsorption techniques to avoid symptoms. A bit of gas but no reflux. Mission accomplished.
Well, the fish wasn’t as crispy as I was hoping. Have to work on it some more. Great find getting the US distributor for the potato starch! I think I’ll have to order a sample too :)
Now to find the potato itself…
You might have some luck with another product I found:
https://www.hiwtc.com/products/jasmine-rice-noodle-8206-42766.htm
I wonder what the minimum order is. If you order a container, put me down for a few cases :)
I’m thinking the reason that the GI for Rice Vermicelli and Rice Paper is low might be due to additional ingredients. It took me awhile to find vermicelli and rice paper made just with rice. Most have added tapioca and/or potato starch.
Whenever I make salad rolls I can’t help thinking the rice used must be sticky rice as they’re so stretchy and glue onto everything. The ones I’m using come from Thailand.
Yes, the mochiko chicken we make is also not particularly crispy, but it’s still moist chicken and delicious. We serve it with a mayo / chili sauce mixture. Let us know if you find a way to make it more crispy. Thanks for posting your resourceful finds. Jasmine noodles – perfect. I will have to check it out and see if I can get some. I am also on the look out for rice paper confirmed to be made from a low amylose rice.
Hi Dr. Robillard,
In an effort to control my long-standing symptoms of gas, bloating and reflux, I started a GAPS diet a couple of weeks ago. Although I experienced alleviation of symptoms within a few days, I found that I also had plummeting energy levels and other signs of ketosis, due to such low carb intake. I am very physically active (in both work and play) and have very low body fat (5′ 10″; 125 lbs). I DO NOT want a ketogenic diet nor do I want to lose weight! To increase energy levels and carbs, I added more fruit and some sprouted lentils, with unhappy results (as you can imagine).
Through continued web research, I found your diet program and am thrilled about the potential of adding some carbs back in. (Also thrilled that heavy cream is acceptable–coffee without it is just not the same!). I also appreciate the mechanistic explanation/theory behind the fermentation potential–it makes a lot of sense to my scientifically-trained brain. I will certainly be turning toward your diet recommendations as the next step in my dietary experimentation. A couple questions for you: 1) Will I be able to consume enough carbs to keep myself out of ketosis, yet still restrict the food source for bacteria? 2) Does the analysis of fermentation potential hold for fungal species as well as bacterial? I have had problems with yeast overgrowths in the past, and am wondering if your diet recommendations will help control fungal populations as well as bacterial.
Thanks for the work you’re doing on this!
Heidi
Hello Heidi,
Thanks for trying the Fast Tract Diet. You can consume plenty of carbs if desired. In the recipes, we kept the overall carb counts to less than 100 grams per day. You can consume more as long as the FP levels are maintained. For instance, jasmine rice has an FP of zero so there is technically no limit to serving size. We recommend limiting servings size to 1/2 cup initially – for the first week or so. We do that in case people have advanced SIBO where bacteria are present in the earliest part of the small intestine. In those cases, even the simplest / most easy to digest and absorb carbs might feed these bacteria. By limiting both FP and the total amount of carbs early on, your control systems (stomach acid, motility, immunity, etc.) can clear out the bacteria.
As for your second question, the diet should also be effective for any fungi involved as these organisms also feed on malabsorbed carbohydrates.
Hi Dr Robillard,
I have both gastritis (infection H. pylori) and IBS-C. Currently I am taking antibiotics to get H.pylori out of the way. After that my doctor wants to do the breathing test for SIBO (but I am sure I have the condition since using Xifaxan in the past keeps my bloating and excess gas away but as soon as I am off of the medication the symptoms comes back). Will you kindly take some time to answer some questions that might help me using your diet?
I have bought your book Fast Tract Digestion (IBS); should I wait for the antibiotics to finish before starting your diet?
I suffer from IBS-C and use Flaxeed (in different forms) to fight constipation. How much Flaxseed can I take while in your diet? Can I take extra fiber (if so what kind)?
The recipes in the book are excellent but they use a lot of dairy products. I am lactose intolerant. Can I substitute the deserts with heavy cream/cheese with other things for the first two weeks?
Also what do you think about using Coconut cream?
In advance, I thank you for your time and all your efforts.
Best, Natalie
Hi Natalie,
I am really sorry to hear that you have had more than your share of gut issues lately. The diet will definitely help. I would not wait to finish the meds. Go ahead and start the diet. You can talk to your doctor about it, but it shouldn’t be a problem. I recommend that you discontinue the flax seed as you begin the diet. If you continue to used it, include the FP – which is basically the fiber in this case. The book does use dairy, but only cream and fermented dairy including yogurt and cheese – all in controlled quantities and all relatively low in lactose. Milk is usually the biggest problem. You can substitute if needed as long as you include the FP in your daily allowance. The coconut cream needs to be used in moderation given the overall carbs and fiber counts. try calculating the FP for the serving size you use for this product (use a glycemic index of 50). If you have problems, contact me.
Very helpful website. I’ve been suffering from what I assume is SIBO for two months, though I didn’t test positively for it. I just ordered your book and plan to start your diet. But one question while I wait for it to come. I drink wine, which mitigates the SIBO symptoms, but I assume you would say I should not drink alcohol?
Hi Melinda, Thanks for the visit and for buying the book. You are in for a pleasant surprise on the topic of wine. I won’t spoil it here.
Hello Norm,
Hope your summer is going well. I thought I would check in with you to see if you received the sample of potato starch from Ingredion. I haven’t ordered a sample yet. Let me know if you like it! I find sweet rice flour has a particular flavor – it would be nice to have an alternative.
Being the researchaholic that I am, I keep a folder with all the tidbits I find. I was just going through it to clear it out and came up with this piece of info that I thought you might be interested in. https://www.thefoodcoach.com.au/food/?W=1&Action=Print&FoodID=524 It gives the GI of rice paper as greater than 70. It’s the only place I found a GI rating for it.
I like rice paper and it seems to like me… :)
Hi Lana,
This summer is exciting but going by too fast. I am presenting a talk called “Did Cavemen Get Heartburn” at the Ancestral Health Symposium this week in Atlanta. It should be fun and I will post the video when available.
Thanks for the link on the GI of rice paper. I won’t be able to officially use is as there is not reference for the information. Still, it’s interesting and 70 sounds about right. Also, those don’t weight much so likely have a pretty low FP is you don’t eat too many.
We tried making some crepes with the Ingredion Elaine 100 – pure amylopectin potato starch. No heartburn and they weren’t too bad – but the recipe still needs some work. They sent me a whole bunch so if you email me your address (normjr1@gmail.com), I will mail you some of my batch for you to fool around with.
Rob, have u studied sea salt much in terms of how it relates to health and food reactions and digestion? I notice that if i load my good with sea salt, i digest better and I don’t get as bad of reactions…. Sans salt, i get major histamine issues (headachey, spacey, dizzy, and craving to eat sugar). Also, i dont feel as anxious. I recently added salt in my diet and noticed these positive changes. My anxiety is less too.
Can an imbalance of sodium/potassium cause these issues? Is high potassium linked to anxiety, insomnia, food reactions, edema, low thirst, water retention, and sugar cravings?
Also, does mold toxicity cause a greater need for sodium?
Thanks a bunch
Any tips to stop losing weight? I can’t seem to stop losing .5-1 lb a week. I don’t know whether to have more carbs or less carbs.
More low FP starches should help. Also, more animal fat may help as well. When ever you reduce carbs, you will typically loose some weight the first week or so, but that should stabilize if you are already lean.
Thanks, Norm. I’ve been on your diet for 6 weeks and am doing much better (though I found when I “cheated” on vacation I had a major IBS relapse so I’ve learned that lesson). My question: as you no doubt know, Elaine Gottshall “forbids” stone fruits, including avocados. And Stanford backs heroon that:
https://stanfordhospital.org/digestivehealth/nutrition/DH-Low-FODMAP-Diet-Handout.pdf
I really don’t want to limit peaches, avocados, etc. You list them as “low” fermenting in your latest book. What are your thoughts on eating them?
I say go for it Melinda. Just keep with the FP limits. You should be fine.
Isn’t it only soluble fiber that’s the problem?
Good question Tom. Put another way, which fiber type is more fermentable? That would be the biggest problem. I believe that soluble fiber is more fermentable (so you would be at least partly right), but since I don’t completely have my arms around which types of fiber are soluble and which are insoluble, it’s still a bit of an open question for me. More thoughts on this would be welcome.
Hi. I’m not sure why my comment didn’t post so I’ll try again.
There is a product called “waxy maize” which the manufacturer describes as “a complex starch derived from Non-GMO corn that is naturally high in amylopectin, a high molecular weight, highly branched polysaccharide…. contains 90% amylopectin. Amylopectin is slowly absorbed by the body, and then easily assimilated by muscle tissue, where it is converted into glycogen. Glycogen can then provide a sustained source of glucose for energy. Unlike maltodextrin or dextrose, Waxy Maize supports glycogen resynthesis well after you are finished working out and sustains energy levels throughout the day.*
This sounds like the opposite of what you’ve said about amylopectin being quickly digested. Is this information wrong?
Hi MZ,
There is an inaccuracy in the above statement. Amylopectin is quickly digested and absorbed. That’s why foods such as Asian sticky rice (100% amylopectin) have a glycemic index of 98.
Not if they are eaten raw, which is how “waxy maize” is intended to be eaten. Waxy maize is a type of corn that is almost entirely amylopectin. It is useful if used raw, (put in smoothies, for example). Raw amylopectin has not been altered by heat, the way the amolypectin in sticky rice has. Please get your facts straight.
There are studies proving that amylopectin, for example waxy maize, eaten uncooked is entirely different in effect on blood sugar than if eaten cooked.
The confusion by sites like yours stems from a study using waxy maize that was cooked with water into a paste – it had the same glycemic impact as glucose does. BUT previous studies on amylopectin, that used it uncooked, showed no such increase in blood sugar or insulin.
Yes, I was referring to cooked foods containing amylopectin. I never said or implied that uncooked amylopectin would have a high GI.
Hi Norm,
I am looking forward to your work on leaky gut syndome. Do you think you will eventually write a book on this subject?
My last blood test 4 months ago showed slightly elevated thyroid antibodies (Hashimoto’s). I could tell that my thyroid was slightly sluggish but the antibodies surprized me. Gluten/Gliadin antibodies were negative, and I have never felt bothered by gluten. It doesn’t bloat me or cause any gas or upset as long as I stick to the low FP items you describe in your book. Yet, there must be somewhat of a leaky gut if thyroid antibodies were present. This may have come from antibiotics prescribed in the past, but of course I can’t say for sure.
My question to you is this: Can high FP foods (foods that cause me to have bloating or gas/acid reflux – like legumes, fruits, or certain whole grains – even gluten-free grains) exacerbate or cause the problem? In other words, if leaky gut is the issue, if I keep the FP down low, can that allow my gut to heal, thus allowing the thyroid to heal through the removal of antibodies?
Thanks so much for your GREAT, GREAT work!
Alana
Hi Alana,
Of course, I’m always working on the next book and will have something to say on this subject. I believe a good case can be made that inflammation from SIBO/dysbiosis is the major cause of leaky gut responsible for the onset of numerous autoimmune reactions. There are typically other genotypic / environmental factors involved, but the leaky gut is likely the most significant means by which triggering proteins (such as gluten for celiacs, Klebsiella proteins for Ankylosing spondylitis, and other cross reacting proteins) enter the blood stream. Over time, I think low FP foods will help heal the gut diminishing or abolishing leaky gut. But antibodies produced from past inflammation/leaky gut episodes can persist based on memory B cells and secondary antibody responses. Overtime, at least in the case of celiac disease Both T and B cell responses diminish upon withdrawal of gluten and restoring gut function. But is it the removal of gluten or reducing the amount of fermentable carbs that’s more important? It may be a combination of both. How this plays out with celiac disease, Hashimoto’s and other autoimmune diseases is something I’m looking at.
Alana,
Have a look at the Conclusive Remarks in this paper
“This new theory implies that once the autoimmune process is activated, it is not auto-perpetuating, but rather can be modulated or even reversed by preventing the continuous interplay between genes and environment. Since TJ dysfunction allows this interaction, new therapeutic strategies aimed at re-establishing the intestinal barrier function offer innovative, unexplored approaches for the treatment of these devastating diseases.”
This is the principle I am operating under. If you can control leaky gut, you may be able to control the progression of many autoimmune diseases by limiting exposure to ingested environmental triggers.
Very interesting manuscript! I want to learn as much as I can about this leaky gut/autoimmune connection. I also find it very interesting (for those of you who think outside the box) that way back in the early part of the last century, a very famous mystic by the name of Edgar Cayce (aka The Sleeping Prophet), described in well over 100 readings the thinning and permeability of the gut wall as being a causitive factor in many illnesses, including arthritis.
As well, I have often heard medical professionals swear that beta casein is the number one cause of T1D. Here’s something about that: https://www.ncbi.nlm.nih.gov/pubmed/12198602 Thanks, Norm!
Hi,
I bought your Fast Tract Digestion IBS book and have a few questions:
1) Is it possible to get rid of SIBO eating raw vegetables and following the books FP guidelines.
2) Are raw vegetable smoothies permissible if they adhere to FP guidelines.
3) Do u know what helps to how to cure Gastroparesis. I did the Heidelberg stomach acid test and it shows that I have excess acid but yet i have NEVER felt heart burn. However, when i eat, I immediately feel extreme distension likely due to extremely slow gastric/stomach emptying. I believe I HAD SIBO but not any more. I just started taking Iberogast a week ago to see if it could help. I eat absolutely no processed foods. What do u think can help?
Thanks
Kes
Hi Kes,
Glad you are reading the book and trying the diet. The answer to 1 and 2 is yes. Gastroparesis has symptom overlap which GERD, IBS and SIBO. I recommend staying the course with any of your current doctors recommendations for your condition while implementing the Fast Tract Diet and see how your symptoms respond. We may be able to help further through our counseling program if you continue to have issues.
Hi Norm.
Firstly thank you for the great advice you give, its comforting to know that someone really knows their stuff on the subject. I shall be buying your book ASAP.
I’ve recently been diagnosed with SIBO and after a ten day course of antibiotics and a thirty day cycle of Probiotics my symptoms improved but came back again after a week. So this process was done again, same thing happened the second time around.
Last week i was put on a three month course of a changing cycle of antibiotics the first being Augmentin (625mg) twice daily coupled with the use of multibionta with probiotic. I was also advised to change my diet to a high fat low carb diet with the ability eat all dairy providing they are high in fat. I was also told to eat some carbs but haven’t due to the amount being so small. As yet certain aspects have improved but the churning sound in my small intestine seems ever present. Would you recommend sticking to this diet or swapping it, as it appears that i’m eating meat virtually every meal. Also looking at what you have written i see that antibiotics are common in the cause of SIBO, though when i asked my specialist he suggested it wasn’t a factor even though my symptoms all came after a course of antibiotics treating an infected wisdom tooth, how likely was this to be the cause of the onset of SIBO. And one last question how long does a sufferer of SIBO usually have the condition once diagnosed and how manageable can it be if a lifetime condition.
regards, steve.
Hi Steve,
You will find the answers in Fast Tract Digestion. I recommend the IBS volume. Antibiotics (or an intestinal infection) can absolutely trigger SIBO/dysbiosis and the symptoms you are experiencing. High fat/low carbs is a good starting point. The Fast Tract Diet has some definite advantages to other diet. For instance, dairy can be a problem in terms on oligosaccharides and lactose and must be limited. You can control SIBO with diet and cure it completely if you address any other underlying factors present – the book explains what these are and how to address them.
Hi Norm,
so do you think the Fast Track Diet also adresses psychological issues like the GAPS. If so, are there any adjustments you suggests (like more strict amount of FP, etc).
Thank you.
Hi Mark,
That’s a good question. I have been doing some work on other SIBO related conditions. Psychological, gut / brain related problems have been a lower priority because I think they are less likely to be tied to SIBO, compared to autoimmune diseases, etc. But it’s certainly possible. Sorry I can’t be of more help on this currently. Given the good results we are seeing using the Fast Tract Diet with other SIBO-related problems, it can’t hurt to try it.
Hi Norm-
So glad I found your website. I was researching resistant starch and was getting ready to try to increase it in my diet thinking that it might help feed my good gut bacteria-but I was nervous because of my history of gut issues. Good thing I happened on your website!
I have MS and have been paleo-esque for 5 yrs since diagnosis. I never eat gluten grains and do not eat much non-gluten grains either, am low dairy, no legumes, etc. I do include rice and potatoes but not too much. I have growing children to cook for and had to make the diet fit so I wasn’t cooking differently for everyone.
I have done extremely well with my MS for 5 yrs. and rarely have issues with the GERD that troubled me before cleaning up my diet. I definitely have trouble with fiber-twice after eating some coconut flakes I thought I would have to be taken to the hospital I was in so much pain. On the occasions that I eat gluten free breads it seems like it takes a long time to digest and I need to drink lots of water. When I used to eat oats I would get severely constipated which still causes me problems. Magnesium really helps me in that regard. I do get gas from fruit-especially the high FP ones you mention. I feel like this info may be another piece to my puzzle. I have had an improvement in my rosacea (no more flushing-this actually stopped when I stopped taking melatonin at night) and a reduction in pimples but still have quite badly clogged pores especially on my chin.
My questions:
which volume should I order?
Is it your opinion that most people with MS suffer from SIBO?
does leaky gut cause SIBO or SIBO cause leaky gut?
splenda makes me nervous-is stevia a problem w/SIBO?
what do you think of soil based probiotics such as Prescript-Assist for SIBO?
Thank-you so much for writing this book I have spent 5 yrs researching and trying to fine tune my diet-I have learned so much but am sometimes stymied by my limited scientific knowledge.
Hi Sarah, I really enjoy hearing from such well informed readers who stand up and fight back by learning as much as possible about their own health issues and reaching out for healthy solutions. I have not seen a lot of info on the connection between MS and SIBO, but I am not surprised due to the fact that some 70% of people with MS have digestive complaints, particularly around motility issues. Motility is a major driver of SIBO and must be addressed to fully resolve SIBO. Every thing you said leads me to believe that the low FP approach would work well for you. I would suggest the IBS volume of Fast Tract Digestion as the sections on gut motility are more extensive. As for your chicken and egg question, SIBO causes leaky gut, not the other way around. If you like Stevia, used the liquid version that is (sugar) alcohol free. Splenda can also be replaced with dextrose (powdered glucose) or maltose (a little harder to find, try brewers supply shop). I am not familiar with Prescript-assist, but please feel to post what you learn here.
Hi Norm.I am suffering for 5 years of bloating nausea gerd(silent reflux) but the worst thing is the fatigue.
5 years ago i used to weight train heavy and took a lot of suplements whey protein vitamins minerals creatine glutamine and i had a stressfull period 4 months in wich i developed erosive esophagitis with after gastro endoscopy but my biggest problem was that i couldn’t eat protein anymore(whey chicken beef ) after i eat it i get belching bloating (burping meat taste) and nasuea fatigue.dr gave me PPi but this made things worse.
I am a pharmacist student and this gerd slowly destroyed my energy focus levels and i do not know what to do and what to eat.i tried all the suplements under the sun for this until i discover rifaximin wich made the symptoms better(i can eat some protein no more fatigue and energy is comming back) but i cannot rely on rifaximin all my life.So i am living in romania i cannot buy ur book but maybe u have the kindness to guide me with sime hints about what u think i might have.I know is related somehow with SIBO.
also simple sugars are ok (rice is a no no ) also mashed potatoes are ok.i do not know what do eat anymore the only time i feel good is when i am fasting but i get tired and fatigue with no nutrients in me.training is hell because of the lack of protein in my body.i also get gerd from drinking water it is hell,i am eating only small bites of everything to feel ok.how can i combine foods to cure myself?
enzymes HCL is a total No for me they make things worse also probiotics and yoghurt are not ok.i think is something related wih fermentation..
Hi Bogdan,
Thanks for writing and truly sorry to hear of your struggles. While it’s possible that you can have some symptoms from excess protein fermentation in your gut, it’s more likely that your bloating, reflux and esophagitis are being caused by carbohydrates in your diet. Some types of rice (jasmine, for example) is OK, others (Uncle Bens, Basmati) are not. The same goes for potatoes. You might not feel symptoms until much later after eating these or other carbohydrates, so its hard to know exactly what food caused it. You should be able to buy the ebook – Fast Tract Digestion Heartburn on Amazon. If you can’t get it from Amazon, write to me at normjr1@gmail.com and we can arrange to have a bound book sent to you.
Hi Bogdan,
I have read the book, and it’s really helped me. Maybe I can offer you some tips since you can’t get a copy where you are.
Just email me, ChristinaEMason at hotmail dot com
Norm may be able to give you some pointers, too.
Christina
Norm “likes” your comment.
Tks so much Norm.
i e-mailed Christina for some meal examples is she has the time and i wnt to ask you
Norm if it’s ok to eat just meat at one meal and how many meals/day are ok in the healing period?
Sorry,i have some idiot questions but these things i ran into every day when i eat.
should i combine small quantity of carbs with meat?
Whey protein isolate is ok to take or cassein?(i do not know the FP of whey)
i am afraid from so much protein of acidosis also my urine is concentrated fro 2 years now like i am dehydrated or something.
TKS A MILLION NORM!
Small amount of carbs with every meal is best, do not have a large meal of carbs unless they are really fast acting carbs like Jasmine rice. Casein protein is terrible for anyone having digestive disorders. Isolate is always best, no time for it to ferment! Use some lemon juice to help with acidosis. The Inuit do not worry about acidosis, I would not put too much fear and worry into that. Good luck.
Tks so much Angela.
Could u give ma a small example of ur meal for 1 day?how many hours before sleep u stop eating an how big are ur portions at one sitting?(i do not have the book)
i have the bad habbit of now chewing verry well the food and i think it’s a big mistake.correct me if i m wrong.
The worst part about having this illness is after i eat i ted to get verry lazy(i think low dopamine) tired no motivation a generally bad mood and when i fast for 5 hours my energy levels come back and only when i am on empty stomach i feel good.
I tred melatonin 6mg before bed for 2 weeks in wich time i felt great my muscles were fuller ,hydrated but i developed anxiety and joint pain so i stopped.
of course the symtoms returned.
i stopped also yesterday the rifaximin after 3 weeks and i feel BAAD.i do not know why but feel bad.
maybe i should’n eat nothing for 2 days..
also i get this from vitamins tablets or capsule(i can tolarate liquid forms)
PLS PLS some hints…
Sounds like you get high blood sugar after a meal. I do not have the book either, but have experimented alot. Keep a food diary. I am not the best to give my menu as I do not tolerate greens at all. I have big problems with salads and anything fiberous and raw. My veggies consist of cooked carrots and some peppers and cucumbers (peeled). I react to all the FODMAPS (I believe Norm has some info on this). I do not tolerate garlic or onion of any kind. Make sure you are taking pro-biotics that do NOT have any pre-biotics(like inulin, chicory,or FOS). Ones with high Bifido are best for me. I eat lots of protein(there is no problem with meat without additives. I eat sushi rice, some hot potatoe(do not eat cold), home made kefir. Keep a food log, I eat right before bed and about % times through out the day. I take melatonin as well and fish oils.
I also cannot eat vegetables or onion garlic but also i cannot eat meat bio or not it’s the same and i simply cannot understand also i have bad breath after meat alone..probiotics i use chewable kind because in my country the ones that are in capsules give me bad nausea..i get bloating belching even from water
Hi Norm.
I tried to send u an e mail but you’re adress is incorrect so please maybe u can give me the e-mail again.
Thanks bogdan. Which email address doesn’t work? I will check it out. For now, you can write me at normjr1@mail.com
Hi Norm.
I tried the e mail adress but an message came back like this
Sorry, we were unable to deliver your message to the following address.
:
Remote host said: 550 Requested action not taken: mailbox unavailable
Basicly i wanted to ask you for a e-book copy of the book ,i am so desperate and i can’t get the book from amazon(politisc stupid bull..)so with all the shame in the world if anyone can help me with an e-book copy i’ll be verry gratefull….it’s not about the money it’s about i can’t find it anywhere and when i did find it the romanian bank that i have visa told me that i cannot make the tanzaction!
The only ebook version is Kindle. Here is a link on suggestions for getting Kindle books in Romania. https://www.mobileread.com/forums/showthread.php?t=131824. I hope this helps Bogdan.
Does amaranth have a really low fp? Livestrong says its glycemic index is 97. I figure 40 grams of carbs worth is an fp of 5.
Bodgan,
If Norm was willing, maybe he could mail you a hard copy of the book by post. You could reimburse him through Paypal or something?
Tks Norm,Christina.
i tried this method and i didn’t got any answer from kindle.
Pls tell me can i drink free lactose milk(it seems i am k with it) and eat small amounts of peanuts throu or eggs.gh the day?
free lactose milk is more ok for me than whey protein isolate and meat or eggs wich gives nausea.
and i have 3 days now with no wheat potatoes legumes bread rice but i eat small amounts of sugar (chocolates or glucose) and i am feeling better.
can i drink sweet beverages like fanta coca cola or sprite?
i can’t go zero carbs so i’m looking for something to eat with simple sugars ..any hints?
Hi, I’ve had the book on ibs for a while. I haven’t been able to fully implement the diet, although I’m sure it would help me (my main symptom, which is bloating, improves on a low-FODMAPs diet, but doesn’t completely disappear. By reading your book, I realized that there are low-FODMAPs foods with high FP).
My issue with the diet is the following: I cannot eat meat and fish a minimum of two times a day, as the sample menus require. I’m not vegetarian, but for different reasons I think I do best if at least one of my main meals is vegetarian. I’ve seen comments by Norman stating that it’s possible to implement a vegetarian version of the diet, but I haven’t been able to figure out how. Has anybody been able to come up with a full day vegetarian menu that is filling but with FP below 30? I’d really appreciate some suggestions.
Hi Maria,
Sorry for missing your question first time around. I am not an expert in vegetarian matters, but here are a few thoughts that others might be able to add to. Most vegetables are low FP. So you can add them pretty much at will. Just avoid the higher FP starchy vegetables in favor of the low FP starches including jasmine or sushi rice, certain potatoes, etc. But you need to find a way to include complete proteins as rices are deficient in certain essential amino acids. Legumes are the go to protein vegetables, but are relatively high in FP. I suggest including some hummus, yogurt if permissible, and nuts. That should cover you for protein. Also include olive or coconut oils for healthy fats.
Hi Norm,
do you suggest to use a sugar and sugar alcohol free tooth paste? Is gum as an ingredient okay?
Hi Mark,
I wouldn’t think it would matter too much if you don’t swallow it.
Hello, I recently purchased your book and it’s been an enlightening read. You mention hypochlorhydria, but finding doctors to perform the test might not be easy. What is the test for hypochlorhydria and how do you get tested? Thank you.
Hi Jean,
Here is a link to the Heidelberg test and doctor referral and one on the use of Betaine to increase stomach acidity.
Thanks for all the great resources on this site! Have you heard of SIBO causing upper abdominal discomfort? I mean the actual stomach area (I know people use stomach to refer to the whole abdomen sometimes, but I am talking about below the sternum but above navel). How might SIBO be experienced differently from another stomach issue such as peptic ulcers in terms of symptom presentation? I have been diagnosed with SIBO but have more upper GI symptoms than lower. Thanks!
Hi Andy,
Do you have acid reflux? This can cause a number of symptoms including nausea and stomach discomfort.
Hi Norm,
Thanks for the reply. No acid reflux as far as I know. I have discomfort below the ribs, but no burning sensation in the chest area or throat and never any acidic taste in the mouth or other feelings of regurgitation. Pretty steady nausea is a problem as well as a dull ache in upper abdomen.
Thanks!
Have you noticed any symptom improvement on the Fast Tract Diet? You might consider H. pylori testing and endoscopy if you haven’t already.
Hi Norm.the nausea is present also in my case although i run 2 weeks on 2 antibiotics bismuth and zantac for H pylori with no succes eliminating the nausea and the fatigue.
i don’t know what kind of gerd i have but 5 years ago when i did an endoscopy they said i have erosive esophagitis so i follwed PPi treatment with really bad side ffects
the thing is i don’t have acid reflux i have silent relfux with bad dyspepsia (foods sits in my stomach toooo long 6 hours ) and i feel fatigued almost all the time maybe because i am malnourished.
and maybe ur opinion on why meat as soon as i swallow it, i burp meat like taste and sits too long in my stomach..
i have ur book and i started the diet but is verry hard.i also weight train( do u think i should stop?)
i try to stay away from all carbs but the protein is the big problem for me..also i get nausea from eggs too.please tell me u have an answer because all the dr i talked to said they never heard problems with protein…what should i eat ,i mean i am looking for a “perfect foods” that does’t sits too long in my stomach and has low g.i.
or maybe i need serotonin treatment?
Hi Bogdan,
You can reduce your meat/eggs and protein levels in general a fair amount without a problem. You can make up your calories with medium chain triglycerides (coconut oil) if you tolerate them (they are generally easy to absorb) as well by adding some low FP starches.
I recommend staying away from serotonin modulation and drugs in general if you possibly can.
Tks good Dr.
one thing i do not understand though,i tried in the past eating only carbs like swets grape juice rice potatoes with no animal protein,i felt ok no more bad breath fatigue depression nausea but still bloating and gaining weight and water retention that’s why is so difficult for me to give up protein is because i gain weight verry fast from carbs,
i must keep insulin at bay..that’s why i am desperate to eat protein with some low g.i carbs but these meals gve me the most unbereable side effects..one thing i can digest is dilluted free lactose milk but i get attention defficit from it and it’s not ok for my studies(hyperactivity relestless leg etc) i do not know why..
so i follwed ur boook and Christina advice and began eating smoked salmon,it is ok but i read it contains nitrites and other not healthy stuff but i keep going,it’s better that cooked meat.
also i want to try biftec tartar..maybe u can help me with some ideea how to keep insulin at bay but also have some proteins in my system(weight training)??peanuts are ok??
Tks a lott
I read about Lactobacillus plantarum 299v (Lp299v) and how it can colonize the small intestine, thus preventing other bacteria from adhering to the intestinal wall, so I started drinking Goodbelly, which has 20 billion Lp299v in it. Would drinking Goodbelly — which also contains concentrated fruit juices and evaporated cane sugar — help my SIBO or hurt it? If it hurts it, would taking Lv299v it in conjunction with your diet help or hurt my SIBO?
Sorry, but I meant to say would taking Lv299v alone without the Goodbelly in conjunction with your diet help or hurt my SIBO?
Hi Brady,
As you likely suspect, the fruit juice concentrates and sugar will exacerbate, not help control SIBO. Taking L. plantarum alone will likely not hurt but there are a couple of relevant points. Since we have a complex population of gut microbes – even in the small intestine, taking a single strain might alter the more balanced natural population that can generally be achieved with diet. Also while most lactic acid bacteria don’t make gas from carbohydrates, L plantarum under certain circumstances can produce carbon dioxide gas (malic acid fermentation, for instance). Taking the supplement alone will probably be fine and who know, might even help, but if you can balance your diet using low FP foods without supplementation, that would be the best bet.
If the L. plantarum can throw off my gut flora, then what about other probiotics? For example, would drinking Lifeway’s Kefir be beneficial? It is 99% lactose free and has 12 different cultures.
The most important thing is to be sure the carbs/FP are inline with the Fast Tract Diet. If so, it should be fine. Just note that many probiotic strains can make gas from carbs (the term is “heterofermentative). That’s why some people report bloating symptoms after taking probiotics. The least troublesome pair is lactobacillus and bifidobacteria.
Does Candida play any role in SIBO? If yes, would your diet help that as well??
Hi Brady,
Some suspect that Candida or other fungi may contribute to SIBO, but to date there is little data supporting this idea. The good news is Candida, like bacteria, dines on fermentable carbohydrates which are limited in the Fast Tract Diet. So the Fast Tract Diet should limit yeast growth as well.
I thoroughly enjoyed your post and look forward to reading your book. As a SIBO sufferer in the past, I have had complete relief of symptoms and tested negative after following the SCD diet for over a year and going through 2 rounds of rifaximin (at the beginning). I also think the addition of herbal antibiotics, ginger and orange peel oil for motility, and digestive enzymes have played a large role in recovery as well. Something this SCD diet does well, is the fermented dairy. I make my own yogurt using gut issue friendly strains and I think that makes a huge different in recolonizing the gut. I have now successfully added back some of the starches you mention being unnecessarily restricted (certain tubers and rice) and other sweeteners that you also discussed. I have experimented with my own personal fructose tolerance level, and find it is quite high. I am enjoyed more variety in my diet but will never go back to the Standard American Diet. Anyway, in my personal journey and professional one (I am a health educator) I have learned a great deal and am always thrilled to find others conducting research in these areas. Have you heard about the SIBO symposium in January? If not, I think you would love it! I will attend via live webinar and am very much looking forward to hearing the presenters – Doctors Pimentel, Siebecker, Wienstock, and Sandburg-Lewis – all SIBO experts, as you well know. https://sibosymposium.com/
Hi Emily,
I’m happy you enjoyed the article. Thanks for sharing what you have learned on the SCD. The supplements you mentiond are very interesting. I hadn’t heard of using ginger and orange peel oil for motility issues. I need to remember that one.
I will definitely be tuning in to the SIBO symposium this January. I met Dr. Siebecker at the Ancestral Health Symposium last August. She is so knowledgeable and dedicated to helping people struggling with SIBO. Her talk was excellent.
What are your thoughts on tap water? Is the chlorine good or bad for people with SIBO??
I am going to buy your book. Before it arrives, would you please tell me what the FPs are for mushrooms, onions, and garlic? Also, are all onions created equal? There are yellow, red, white, and sweet/Vidalia onions, so I would think that their FPs would be different as well.
The FP for 2.8 ounce servings of mushrooms or onions is 3 and 5 grams respectively. I didn’t do a calculation for garlic as of yet, but since a clove has so few total carbohydrates, I wouldn’t worry about it.
Hi Norm,
bought your new book,just working through it now.
2 questions
whats your take on barley malt and or Rice syrup as sweeteners.
and I have psoriasis which many say can be gut related,have you come across any such link in your work?
thanks
Chris
Hi Chris,
Barley malt and rice syrup make good sweeteners. Use them sparingly at first and see how you tolerate them.
I have not seen too much on psoriasis and SIBO/dysbiosis, but will be doing some work on this early next spring. You might want to check back then. I will tell you this much. I had psoriasis through out the nineties and it abruptly went in to remission in 2004 (never to return) when I started low carb dieting. But that’s just an N=1 story. The great thing about the Fast Tract Diet or low carb diet is you can always try it to see if it works with no downside risk.
Hi,
I have seborrhoeic eczema and I found out that it gets worse on carbohydrates. Now the carbs with low fermented potential described in Fast Track Diet indeed don’t exacerbate the eczema and overall my skin is much better but the excema isn’t gone (yet – hopefully).
On the other side I am not sure if I have SIBO because besides excema I don’t get sudden symptoms on carbohydrates except that I have extreme cravings which regularly lead to overeating.
Norm, do you think that eating FTD will restore the colon flora as well?
The diet won’t add lost organisms. They need to repopulate as they are reintroduced from the environment and diet over time. But the diet should provide a healthy / competitive atmosphere for the organisms as they are reintroduced.
Hi Norm
thanks very much for your reply.
thats very interesting and inspiring that you had psoriasis and it retracted on the low carb.will keep you posted as I’ve had P for 38 years and only chinese medicine cleared it for about 18 months .
this is a great site especially as you engage with your readers so well.
thanks again
Chris
My pleasure Chris. I learn a lot myself from all the thought-provoking posts on this site. Its funny, I never gave a thought about my own psoriasis until you asked this question. I never made the connection. I had forgotten about it entirely. I hope yours goes into full remission for good.
Thanks Norm.
Im a little confused as i looked up jasmine rice as ive never used this
And it said its less sticky as it contains less amylopectin yet i thought
It contained more because of less amylose?
Could you clarify please
Regards
Chris
It was a wilkapedia site, 1st site that came up, reading others it seems
that its misleading. Just bought some to try.first day of the regime.
Chris
Hi Chris,
Not sure what you read, but jasmine rice contains very little amylose, hence the very high GI / low FP. I am not sure why it does not have the sticky nature of sticky rice, but it does contain mostly amylopectin starch.
Hi Norm
Thanks for the clarification. Just for the record, this is the link to
The wilki site which was a bit misleading,
https://en.m.wikipedia.org/wiki/Jasmine_rice
Regime going well so far, love your book
Cheers
Chris
Thanks for the link Chris. Actually, it’s technically accurate. Jasmine rice does have less amylopectin than short grain sticky rice (which is 100% amylopectin) and a bit of amylose. But that’s still a lot less amylose than high FP varieties such as Uncle Bens.
Hi Norm,
Thanks for that. In your book the jasmin rice has a 0 fp yet the stick rice has 100 amylopectin and a rating of 3 fp, is this because the sticky rice has 2 asca fibre score compared to 0 for the jasmin ?
Chris
Yes, the reported fiber value is one reason the FPs are different. But GI measurement is not a perfect science. There is some degree of variability based on test methodology, which lab and analyst does the test, individual differences in the test subjects (people) and finally differences in food source and preparation method. Helping to even out this variability is repeat testing. Many of the GI values used to calculate FP come from several GI test results that are averaged.
I just ordered your Fast Track IBS. Should I have read your first book too? I am suffering from abdominal pain for 7 years which just turned into severe constipation. All the doctor’s theories have proved wrong They told me initially that my pancreas was inflamed, not they say I never had pancreatitis. So confused and so sick. It does seem that all my healthy high fiber foods and PPIs have exacerbated my condition. Help.
Hi Loretta,
There is no guarantee that your symptoms are caused only by IBS, but reading the sections on constipation and underlying conditions should help. I recommend trying the diet, talking to your doctor about weaning off PPIs, and losing the fiber. Let me know how you make out.
The book arrived and it is very helpful. Recent colonoscopy ruled out anything that might have contributed to constipation. I have experienced tremendous relief following your protocol. The recipes are a little involved for me but I find that recipes on other SIBO diet sites disagree with your guidelines. Does your first book have additional recipes or can you recommend a source?
Hi Loretta, Great to here that your constipation has responded to the Fast Tract Diet. Some recipes are more involved than others, but you can always use the basic low FP foods from the recipes and prepare them your own way. The Fast Tract recipes differ from other SIBO recipe sites because they are based on my novel formula for evaluating the symptom potential of different foods.
In terms of additional recipes, The Fast Tract Digestion IBS and Heartburn books both have many unique recipes, so having both books will provide more variety for sure. You can also make your own recipes simply by choosing low FP foods from the tables in the appendices. Also check out the recipe section on this blog, though some of these may appear in the books.
Are Miso and use Japanese plum sauce useful as anti bacterial condiments,
Macrobiotics considered them highly?
I am not sure Chris. I do know that wasabi has antimicrobial properties. But my real effort has been focused on limiting the overfeeding of gut microbes, not inhibiting their growth by chemical or natural antibiotics. Fermented foods in general, including miso, fit this strategy.
I want to buy some sugar-free gum. Which brand do you recommend for people with SIBO? BTW, I just bought your book and am in the process of reading it. VERY informative!!!
Hey Brady,
Good question. All that I could find have either sugar alcohols or sugar. Even Stevia-sweetened gum has sugar alcohols. The best bet might be regular sugar sweetened gum that has 2 grams of sugar, some of which is dextrose, so the FP would be below 1 gram per piece. Let us know if you find a better solution.
Once your diet eliminates my SIBO, how long, in your opinion, will it take the inflammation in my small intestine to heal? I ask because my antidepressant medication, which I take for a serotonin deficiency due to chronic back & neck pain, became ineffective after my SIBO arose, which I deduce was due to inflammation reducing how much medication got absorbed..
How long depends on the extent of intestinal damage as well as how effectively SIBO / dysbiosis or various underlying conditions driving the problem are addressed. Most people with GERD (including me) and IBS begin feeling much better in a matter of days. More extensive damage from Celiac Disease, for instance, can take months or even years to fully heal.
Hi Dr. Robillard,
I just ordered your book yesterday and am looking forward to reading it. I feel it’s essential to address the cause and not just the effects, and I have a gut feeling (pardon the pun) SIBO is my problem.
For years I simply avoided the worst offenders (rice, potatoes, bananas) but it got worse as my health declined, so I tried Carol Sinclair’s starch-free diet. But that just made matters worse because it made me eat more of other foods that were even more problematic (according to her, honey is the best thing ever, but it was the worst for me.) Once I had completely cut out absolutely all starch and my symptoms were just as bad, I finally found out about the low-Fodmap diet. I added that to the starch-free diet, but not only is it prohibitively restrictive (I also have outright food allergies to contend with), it hasn’t solved the problem. As soon as I add any of the supposedly starch-free low-fodmap fruits or vegetables, symptoms return (including an unbearably itchy rash on my abdomen and lower back.) It may just be after all the high fodmap food I ate on the starch-free diet, the bacteria have overgrown so much I cannot even tolerate small amounts. But I’m hoping your diet will provide me with more information that can help me eat at least some fruits and vegetables (I would be in heaven if I could eat certain kinds of potatoes and rice after all these years!) Malnutrition and weight loss are becoming a problem. It probably won’t be a perfect fit for me (I react badly to watermelon but seem to tolerate sugar–I drink a lot of ginger ale for nausea without problem) but maybe by mixing and matching I can tailor something to my own individual idiosyncrasies.
Speaking of malnutrition, I’m trying to take vitamins while I sort this out, but all of them seem to contain cellulose. Do you know if that’s a problem for SIBO?
A few things that may be of interest to you: my IBS started when I was prescribed megadoses of iron for anemia about 15 years ago. I thought the problems would go away when I stopped taking the iron but they never did. I’ve been told iron fuels bad bacteria in the gut. But prior infections probably made me vulnerable. Before that I had a couple bouts of amoebic dysentery while working in Central America. And it has now been confirmed via biopsies I have a chronic enteroviral infection which causes IBS amongst many other problems. (I was infected at age 8 by my father, a microbiologist handling enteroviral-infected fecal samples, and lax about washing his hands.) Dr. John Chia at the Enterovirus Foundation did the tests; he is spearheading research into chronic enteroviral infections. https://enterovirusfoundation.org/index.shtml
Another contributory problem in my case is fatty liver. Because my common bile duct is clogged with fatty “stones,” enzymes from my pancreas don’t get through as well, carbs go undigested, you know the rest (you came up with the theory :) ). I have done many liver flushes and flushed out ridiculous quantities of “stones,” and in the few days or weeks afterward before more fat clumps have descended to block the CBD again, my IBS completely goes away as do my food allergies. I’m unfortunately too sick at the moment to keep doing the liver flushes. So I’m hoping a more gentle and gradual approach through diet will bring the SIBO numbers down for starters. I haven’t read your book yet, but my understanding so far, in a nutshell, is: too many bacteria, not enough enzymes. So I’ll start by decreasing the bacteria, then increase the enzymes when I can.
Thank you!
Your book is in the mail. Give it a read and try the diet without worrying too much about all the other things you’ve heard. You may find you don’t actually have many food allergies once you are controlling FP. Bacteria do sequester iron to live, but they also need fuel (mostly carbs) to grow. Also don’t worry about cellulose in your vitamins. The amount is small and cellulose is the least offensive fiber type.
Thank you for the reply. It’s good to know I can keep taking the vitamins while I sort this out. It’s all very complicated and confusing, with so far things only half-helping or making things worse. I look forward to reading your book and I’ll clean the slate and try the diet as you suggest.
Hi Norm,
I’ve got a few questions if you don’t mind.
a) I read somewhere that you now recommend 7FP per meal as low (I think some presentation slides). In my book version it is still 10. Do you have written an article recently which points out the new guidelines for those who bought the old version?
b) How much does fat influence the FP because I read that combining foods with fat can reduce the GI by a third. So that would turn a slice of baguette (30g, GI 95, 1FP) with butter to around 6FP (with GI 65 if I calculated right).
c) I have IBS-C with strong malaise, dizziness, burning mucous membranes throughout the body after eating especially from fatty, sour, spicy foods. Carbohydrates I actually do tolerate quite well except that I crave them a lot which leads to overeating frequently which makes my situation worse over and over again. Since FTD approved foods usually being high glycemic it became even harder to withstand the cravings.
Diagnosis couldn’t find anything except a tissue example from colonoscopy recently showed “focally accented eosinophile in the colon mucosa”. I don’t have allergies so I don’t know how to connect this to anything which could make sense. Do you have a guess?
d) I think my constipation was triggered by antidepressants and 5htp I took for several years. I skipped them four years ago, but my constipation is as bad as ever. Have you come across some informations that this is plausible and what might I do about it?
Thanks and all the best
Mark
Hi Mark, I am not in a position to comment on “d.” We did revise downward slightly the cut-off for low FP meals, but how you feel in terms of symptoms is a far more important determinant. You should find your own cut off as you try the diet. This cutoff may increase overtime. Fat’s and other factors can influence GI and hence FP. But all carb-containing foods will be affected, so it still makes sense consume lower FP foods. If you are reacting to fatty foods in the absence of carbs, you may have another type of problem / complication beyond carbohydrate malabsorption – such as lipase deficiency /gallbladder issues, etc. You may need to explore further to see what is driving this reaction to fat. I am afraid I can’t comment on your colonoscopy results.
Dear Norm,
I ordered your book 2 days ago and am really looking forward to reading it… the information on SIBO is so conflicting! I’m not totally sure that’s what I have but my intuition and symptoms indicate so. I”ve literally had the runs for 5 months on and off and i’m an a long distance bike rider!! Imagine how that gets in the way! last year after feeling bloating and gas in my stomach after eating I had an endoscopy and colonoscopy all coming out normal and the GI dr said he did biopsies…not sure of what… but all was normal and he said I had IBS… literally because he didn’t know(he admitted this to me) … Anyway i’ve been on a low carb diet for a long long time and have eaten pretty healthy…. wine and cocktails are my downfall, however recently i’ve stopped those too. My Naturopath and I have finally gotten to me doing the SIBO antibiotic protocol… Im on my 6th day of metronidaziole and neomycin and it’s been difficult. Today is the first day i felt better. After reading so many articles and your blog i’m realizing that the veggies i’ve been eating are feeding the bacteria….like lots of broccoli and cabbage family veggies. I’ve been mostly gluten free for several months also. i was hoping to be done with this very soon but from what i’m reading it sounds like this is a long process…. I want my life back!!! so here’s my questions and i’m sure some of this will be answered in your book but i can’t wait i feel so limited in what to eat!!
1.Can i have lettuce ? Like a ceasars salad? no croutons or gluten free ones?
2.Also you seem to support he Paleo diet and they say this bone broth is really really nutritious for the gut.. what’s your feeling on that?
And I’m hoping your book will fly quickly across this ocean to me…
Thank you for your time…
Angela from Kauai
Hi Angela,
Yes, your questions are covered in the book which contains a recipe for Ceasar salad (there is also a recipe for Caesar salad on this site). Bone broth is wonderful stuff and fully supportive for SIBO.
The FP tables in your book don’t mention lactose-free milk, so what is the FP of lactose-free milk?
Great question Brady. I have not found a published glycemic index for lactose-free milk. Clearly lactose-free milk will have a lower FP than regular since the lactose is broken down to two much easier to digest sugars, but you still have other oligosaccharides to deal with. Let me give this one a bit more thought.
Hi,
Can you explain your reasoning as to why you think resistant starch are bad for a SIBO suffering patient?
I am currently on low FODMAP diet and I find to be able to handle resistant starch just fine.. and I was diagnosed with SIBO last year.
Hi Ray,
Thanks for your question and comment. This article gives my general rational. Also, my own reflux symptoms act up when I include starches (other than low amylose / high amylopectin starches) in my diet. What else in foods like potato and pasta would be driving my symptoms, I can’t imagine. Did you add the RS after your symptoms were under control on FODMAP or jump right in? One possibility is that some people can tolerate certain types of carbs better than others. But your case does make me curious.
Hi Norm,
I’m stil waiting for your book to arrive so I need to ask this question. I’m a long distance bike rider and have been using hammer nutrition Heet as my electolyte nutritional drink. it has 2g of sugar..xylitol.. and 25 grams complex carbos…not sure what they are… it hasn’t bothered me in the past like creating gas or anything but i’m not sure. i need to have something to replenish and i discovered that their plain electrolyte tabs have tiny amounts of sorbitol and stevia… any suggestions? are they ok or just eliminate completely?
also what is “femented cheese”?
thank you…
I made the bone broth..it’s a little greasy…
aloha, Angela
Hi Angela,
I would consider any drink with xylitol and can complex carbs to have relatively high symptom potential. But if it hasn’t bothered you who am I to tell you to stop. But somethings things you consume now will bother you later. Proceed with caution. All cheeses are fermented, that’s why they contain only small amounts of sugar – because bacteria used in the fermentation have consumed most of the carbs. Cheese would be a good snack on your trip as would be the recipe “Anne’s recipe for Jasmine Energy Balls” on the Consultation tab.
Norm,
Thank you so much for your prompt reply… i am truly impressed with your commitment to help people!!!!! I actually saw those and sounds good for training. the electrolytes I have have sorbitol.. it’s a tablet I just put in water.. is it okay or do you have another suggestion for an electrolyte drink?
thank you so much and Aloha,
Angela
I JUST PURCHASED BOTH BOOKS ON AMAZON AND GOT A POSITIVE BREATH TEST FOR SIBO, MY DOCTOR IS PERSCRIBING 20 DAYS OF NEOMYACIN 500 MG 2X DAY AND XIFAZON 550 MG 3X DAY AND THEN 50 MG ERTHROMYACIN FOR 3 MONTHS AS YOU CAN IMAGINE I AM REALLY FREAKED OUT ABOUT ALL THE ANTIBIOTICS . I GENERALLY GO WITH A MORE NATURAL METHOD FOR TREATING THINGS. I WAS IN ANTIBIOTICS BACK IN MAY FOR DENTAL WORK. DID NOT HAVE ANY OBVIOUS PROBLEMS ATTHE TIME , I HAVE HAD ACIS REFLUX FOR 3 YEARS BUT DO NOT TAKE MEDS JUST WATCH DIET. IT SEEMS THAT WHEN I STARTED TAKING A PROBIOTIC CALLED LACTINEX THAT THE PROBLEMS REALLY STARTE WITH THE SIBO OR AT LEAST THE PAIN AND BLOATING . CAN YOU SHED ANY LIGHT ON WHY A PROBIOTIC WOULD MAKE THIS WORSE OR BRING THE CONDITION ON IF IT WAS UNDERLYING ANS ALSO DO YOU THINK I SHOILD START THE MEDS OR WAIT FOR THE BOOK TO GETHERE AND CAN THIS BE CURED WITHOUT MEDS . PLEASE HELP I AM DESPERATE, I DONT KNOW WHATTO DO OR WHAT I CAN EAT . PLEASE PLEASE HELP
THANKS DINA
Hi Dina,
Your doctor is in the best position to help you make critical decisions about your health. On this particular matter, I suggest you bring the books to share with him or her and ask about the possibility of trying the diet before you take any antibiotics. You can find the rational for giving the diet a try first in Fast Tract Digestion IBS, Chapter 5. And also in a blog article entitled “Antibiotics for my IBS” on this site.
Also, I recommend stopping the probiotics for now as well. Some probiotic bacteria make gas from carbs causing bloating. And taking a small number of probiotic strains don’t do much to rebuild your gut microbiome which is comprised of hundreds of different species. If you really wanted to take a probiotic, you could try a simple lactobacillus probiotic – this strain makes no gas and does produce healthy lactic acid. But with or without a probiotic, your gut microbe diversity should gradually improve over time as long as you are following the Fast Tact Diet and staying healthy overall including good hydration and a multivitamin with minerals until you recover. Avoiding antibiotics (unless you are very sick, then they can save your life) is one of the most gut-healthy things you can do.
ALSO FORGOT TO ASK IS ORGANIC YACON SYRUP ALRIGHT TO USE . THANKS DINA
No!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!
Just kidding, but no, it’s the opposite of good and has high Fermentation Potential (FP). The same goes for Agave – with lots of sugar alcohols. Dextrose is a much better choice. Barley malt syrup is another alternative if you don’t have gluten sensitivity.
Hi dr, I am excited to find this post. I have been dealing with SIBO for a year and am a patient of dr seibeckers. She is wonderful.
You don’t mention the migrating motor complex and its role (buying ur book Today so perhaps I will be reading about it in the book?). I was under the impression that SIBO could never be healed because what is broken is the migrating motor complex and therefore even if you get rid of the bacteria, eventually it will buildup again because the MMC is not working. What are your thoughts on this? Can the mmc ever be inner gated again?
We just found out that my daughter who is five years old, is positive for SIBO. She’s been having symptoms for a long while and I just feel awful but she has to go through life being so limited. I really didn’t mind my limits but for my baby, it is heartbreaking. Any thoughts on recovery for children? I guess I’m just hoping to hear that children are better able to recover from this because from what I am experiencing and reading adults don’t usually seem to recover for very long.
What are your thoughts on lyme disease linked with SIBO? We were both just diagnosed with Lyme disease and because I did not think SIB was genetic or contagious I just can’t see how my daughter and I both have this without there being a link to lyme disease. Also do you think treating Lyme disease will help sibo?
Also where are you located and can I make an appointment with you?
Hi Cheryl,
Glad to here you have been working with Dr. Seibecker, a real expert in this area. I do address motility issues in Fast Tract Digestion though I don’t refer to these issues as the MMC. Some forms of dysmotility, such as those caused by surgery or scarring, may be permanent, but others are more likely temporary based on your bodies reactions to food, nutrients or other factors. Regardless, modifying diet by reducing high FP foods is a supportive measure I highly recommend for SIBO-related conditions.
I have not given much thought to a connection between Lyme disease and SIBO, though I am aware of anecdotal reports of a connection. Have you taken antibiotic for the Lyme and if so, have you noticed any improvement in SIBO symptoms?
You can find our contact information on the Consultation tab on this site. We offer consultation by phone, so our location (Watertown, MA) won’t be a factor.
Hello Dr. Robillard,
Very happy to come across this site and I am going to try and find your book today. I am being treated for SIBO by Seibecker’s collegue Dr. Steven Sandberg-Lewis at the SIBO Clinic. I am following Seibeckers diet plan which combines SCD and Low Fodmap. My biggest issue with this diet is due to all the conflicting information given by very knowledgeable experts on what is “legal” and ‘illegal”. It’s interesting for example that you say Jasmin rice is a low FP yet and allowable, yet Seibecker does not allow for any grain. Also she says bone broth soup is ok in limited quantities because it contains polysaccharides. This diet is challenging enough and it’s easy to feel isolated, but the great challenge too is trying to discern who is correct on any given foods. I would give anything to eat Jasmine rice, but can I? It’s the inconsistency that is most troubling. Please try to understand how for some of us, this diet very difficult and to me, perhaps potentially unhealthy given the fact that so many important fruits and vegetables are not allowed.
Thank you for your thoughtful consideration. Diets that are too restrictive have the most failure rate among those with even the best intention of following it.
Terry
Hi Terry. All I can say is please read the book and have a look at the various blogs and comments on this site. The rational is very clear as to why jasmine rice is allowed and the tables in the back of the book will show you which friuts are safe and which ones you should consume in limited quantities based on the FP system. Also check out the SIBO diet comparison here. I am not aware of polysaccharides in bone broth and can’t imagine this being a problem.
Dr. R,
Just one last thing, I see that you know Seibecker and her collegue Sinclair Lewis. Are you familiar with her SCD and Low FODMAP chart? She also says no garlic or onions and allows 2 tbls of honey at at time. What are your thoughts here? You mention not to worry about garlic because it has such low carbs.
Terry
Hi Norm,
I’ve been suffering from GERD for several years now (and also systemic Candida probably due to or at least much worse due to PPI usage) and have tried a number of dietary approaches with different results. While I am inclined to agree with you about the connection with SIBO and carbohydrate malabsorption, for me personally fructose (from fruits) does not seem to pose a problem.
A while ago I went through a raw vegan period where I would eat nothing but fresh raw fruits and vegetables, with often more than 10 bananas a day. I did not exclude certain types of fruit or anything like that. While I couldn’t keep up with such a restricted diet for more than 2 weeks at a time, my acid (and pepsin) reflux did go away completely while on the diet and my Candida overgrowth (thrush, balanitis) also improved greatly. In fact, I had no digestive problems whatsoever and could leave the PPIs behind. When I quit the diet it all came back (gradually).
Might you have some insight as to why this is? I am convinced that I have SIBO (or SIFO?) and whenever I increase my consumption of grains I get more bloated. When the holidays are over I’d like to start with your Fast Tract Diet plan, but I am somewhat unsure as to what to do with fruits. I would like to incorporate them as they don’t seem to cause me any trouble.
I would love to hear your thoughts on this. Thanks for reading!
Hey Tom,
You might be right and fructose is not a problem for you. Not everyone malabsorbs fructose. It won’t hurt to try the Fast Tract Diet without limiting fruit. If it doesn’t work, you can always double back and restrict the highest FP fruits.
Cheers
Your book doesn’t mention whether or not the fillers and fibers in multivitamins are good for people with SIBO. I’ve been checking out the ingredients for several multivitamins, and all of the ones at Wal-Mart have some sort of fiber in them. Which multivitamin do you recommend for people with SIBO?
Hi Brady,
A couple of points. The amount of fiber in vitamins is so small (less than a gram), it should not present a problem. Also, cellulose, commonly included, is the least fermentable fiber type. So I wouldn’t worry about.
Dr. Robillard,
I was recently diagnosed with SIBO and currently on Xifaxan ( for a second time) at a dosage of 1650mg daily in three divided doses. I’m also on a PPI, oh what a surprise …..
I am very concerned because I also have been battling chronic urticaria with mad histamine releases for about one year, which are hardly controllable on daily antihistamines plus an H2 blocker as needed. I am being considered for Xolair injections by my physician at MGH in Boston to help with this raging urticaria.
What are your thoughts?
Hi Shari,
Really sorry to hear about your current condition. SIBO and allergic reactions together sound challenging. It’s possible they are related (via leaky gut / food allergens). If you have not tried the Fast Tract Approach, I would recommend this as a starting point. You might also read my article on antibiotics for IBS. We do offer counseling if you wanted to delve deeper.
Greetings, Norm and fellow readers! Thanks so very much, Norm, for your terrific work. I’ve been on a “fast tract” regarding educating myself about SIBO, IBS, and slow motility… more than 5 years of symptoms are starting to make sense. Food glorious food has been ‘ the enemy’ for so long …! I’m looking forward to trying a new approach through your ideas and your book.
I have a couple of questions. I was put on Xifran for a 2-week period, but I lasted for only 1 week – my symptoms seemed to be getting worse and worse. I have heard about a “shedding” phenomenon when the gut bacteria are starved … can symptoms be exacerbated by antibiotics…? Just as a happenstance, when treated with Doxycycline for another issue, my intestinal symptoms dramatically improved… for a short while. Is it worth rummaging around in the antibiotic cabinet for one that offers some symptoms relief, while shifting to the dietary focus?
Second question …. I’m sure you address this in your book (I’m ordering it tonight!!)… my biggest problem is keeping up a calorie intake daily. Eating causes so much pain that I’ve reduced my food intake to 1 egg, a bit of brown-rice based (non-yeast) tortilla (GF) that I can tolerate, stewed tomatoes, occasional small slices of avocado, and occasional kelp or spinach. That’s about it. I tried eating salmon and had a terrible reaction. I can tolerate sardines… almost every food except eggs seems to give me problems. So, I’m losing weight and down to the ‘don’t go lower’ zone… at 5’2″ and 97 lbs. I’m wondering if I should ask an M.D. to explore any types of liquid nutrition, etc. – I’m concerned about the weight loss and just can’t eat.
The issue that I wonder about overall with a number of carb reduction diets is how to maintain a healthy weight. Perhaps I’m simply remarkably under-educated about nutrition (this may certainly be so…) but it’s a tough battle to keep the calories coming in.
Sorry for such a long post..!!!
All best to everybody here… may your symptoms resolve soon and permanently!
Thanks, Norm, you’re really so kind to respond to these inquiries and make yourself available for dialogue here. It’s above and beyond the call of duty…!
LK
HI LK,
Thanks for visiting the site. I am glad you are getting the book as it contains the answers you’re looking for. The most likely reason xifaxin is not working is because your gut is colonized with bacteria that are resistant to this antibiotic. Please read the book before searching for additional antibiotics which negatively impact the diversity of your entire gut microbiome. We also offer individual counseling for a variety of specific issues such as ways to control excessive weight loss.
Hello Dr. Robillard!
I’m now following the Fast Tract Digestion-GERD plan, trying to manage my health issues. Your books are great and shoking and fresh! I beleive that you provide a real answer for many health problems. I hope that this type of diet will help me to solve my issues too (bile and acid reflux, bile gastritis).
I’m just one day of strict counting FP of all the day meals , so i am at the very beginning of the story.
What is your opinion about Fast Tract diet effectiveness in the case of biliary reflux?
Sincerely,
Alexandra K.
Hi Alexandra,
When studies have examined refluxate, they have found bile. So I imagine anyone who has acid reflux has a bile component as well as acid, digestive enzymes and bacteria. The key is controlling the reflux. Once you accomplish that you should have no trouble.
It gives hope!
Thank you very much for the answers here – it is very encouraging!
Best regards,
Alexandra K.
Hi Norm, trying to calculate the FP of buckwheat but have some questions. How much does preparation factor into the equation? I cooked groats in the pressure cooker then then blended them into a creamy porridge. But the numbers I found on the Internet were based on the groats or sometimes the flour. I came up with 16 for FP, which is way higher than I’d like, but this may vary greatly based on preparation method . What do you think? Getting tired of just jasmine rice so wanted some other low FP breakfast and snacks options.
Thanks
Doug
Hi Doug,
I can’t answer that without knowing the serving size. I get an FP of 13 grams for a (dry) serving of 1.1 ounces. Hope that helps.
Also, you might consider cream and glutinous rice.
Hi Norm,
i was wondering about coconut water… I couldn’t find anything about it in your book?
It has a lot of electrolytes and would be good for me bike riding… Also I had a bad reaction to watermelon… ??? Is it the sugar in there?
thank you and much Aloha, Angela
Hi Angela,
Then FP for coconut water is 9 grams for an 8.8 ounce serving. A dextrose-based electrolyte drink would be better.
As stated in the tables, the FP for watermelon is very low – based on GI testing in healthy individuals. But some of the sugar in watermelon is fructose which could be giving you symptoms. But make sure watermelon is not getting the blame for symptoms caused by something else you ate before. Foods with a lot of fiber may cause delayed symptoms for example.
THank you so much for your prompt replies…. you are awesome.. I guess I will have to do more searching to find me an elcetrolyte drink….Also in the book you say that carbs will increase x3 if cooled and then eaten. So I made those Jasmine rice balls for a long ride i’m doing later today. they are in the frig. are they going to be ok?… i’m doing much better BTW…. Just trying to figure out how to implement into my current lifestyle.
thank you thank you…..And aloha, Angela
Let them warm to ambient temp on the ride (in that beautiful Kawaiin sun). Further warm each bite in your mouth as you eat them and chew well, eat slowly. You should be alright.
Pretty sure watermelon is high in fructose as well as fructans and/or polyols. I think the Chinese use it as their go-to constipation cure for this reason (like we do Prunes?). Combining the Fast Tract diet with the FODMAPS diet might help you? This is all based on random stuff I’ve read over the past couple years, but it might be worth investigating….
Thank you!!!!! yeah i’m nervous about fruits… it seems blueberries are ok tho…
Aloha, Angela
Hi Norm,
Just thought I would touch base with you again. I wanted to let you know that I found out that my particular issue with acid reflux (which I control beautifully with your program) comes from having fructose malabsorption. I learned this from a breath test I recently took. I have always suspected fruit and legumes to be problematic, far more so than grains for me. So, I did some research online and discovered there is a digestive enzyme product called Digest Spectrum, made by Enzymedica, that is useful for the treatment of fructose malabsorption. Many people swear by it! So I bought some from Whole Foods to see if it would help me, too, if I over indulged in black-eyed peas for New Year’s day, or ate a whole pear or an apple. It really did seem to help greatly. Normally I would have been very uncomfortable after eating legumes and fruit, but not when I took the enzyme. So, I am hopeful and wanted to pass this on to you and your readers. You may already be aware of the product. I know it contains an enzyme called Xylanase that may be helpful to some people. Wishing you all the BEST! Thanks for everything you do for all of us!
Interesting. Let me know how it works for you. Not sure what xylanase would do for fructose malabsorption, but it might help with the breakdown of fiber: “Xylanase is an enzyme that catalyzes the hydrolysis of 1,4-beta-D-xylosidic linkages in xylans that are constituents of hemicellulose, a structural component of plant cell walls.”
As far as I know there is no enzyme out there for aiding fructose digestion, although I think I read somewhere that they are working on such a thing in Europe… (also, I am not sure how that would work since fructose is a single sugar). Perhaps it helps through the breakdown of fibers that often come with fructose in whole foods? Still, I decided to search in case there was something new I didn’t know about and I did find people who had really good results with this product, so I decided to try it, too.
I have your two books. I been ill following a heart stent 4-23, bloating, constipation, upper GI and lower. I use Linzess pill and 2 gram glycerine to have bowels move. But I need to use diet liquid drinks for one meal a day, did you evaluate any for short carbs or Low carb fermentation for carbs in say Glucerna 11 oz hunger shake? or for the sugar in this diet drink, Is it fructose or part fructose? what, with regard to SIBO, is best or most healthy diet liquid drink sold in stores, as I use one or sometimes two daily with one regular meal? cityjimmy@yahoo.com
Hi James,
The Glucerna shakes include fructose, fiber and other carbs and have 16 grams total carbs for an 11.5 oz serving. I calculate the FP to be approximatley 12 grams for that serving size. I haven’t fully researched “meal replacement” shakes and can’t assess your nutritional requirements for this liquid meal based on this short exchange, but strictly from a low FP stance, something like the Atkins Advantage shake has an FP value of under 2 grams.
Hi Norm just wondering of chewing gum made with sugar was Ok and whar about condiments like mayo . ketchup i guess is best avoided because of sugar , mustard ok i would assume and once you get SIBO under control canyou have ann occasional day or meal where you eat what ever you want as long as you get right back on track and what if you cheat onthe diet how long does it take to recover from it there have been a few times where i have caved and had a piece of cake or chips and salsa , how much damage have i done if I get right back on track ? Looking forward to the next book Thanks !!
Hi Dina, Chewing gum has sugar, but it’s not much if you don’t over do it. Ketchup also has some sugar, but again just don’t over do it. Mustard is fine. We all cheat once in a while but once your symptoms are under control, you will find you are more tolerant to these periodic indulgences.Then just get back to low FP and all will be great.
Greetings, Dr. Robillard and fellow readers! Thank you for your Fast Tract
publication and all of the very detailed and comprehensive research involved.
I also wanted to mention that I am so deeply impressed by the fact that when
readers bring up other ‘plans’ and questions about these, that you are extremely
open to looking into other researchers’ work and examining the approaches as
these compare to your own. This adds tremendously to the knowledge base
for fellow SIBO people and very much applauded.
–
I wanted to mention to readers / Dr. Robillard – transitioning to essentially
‘home cooked’ food to make sure there are no additives, I recently made
almond milk, sunflower seed milk, and cashew milk. These are so very
easy and satisfying to make, by simply soaking the nuts/ seeds overnight,
straining, putting in a blender with fresh water (about 2/3 seeds or nuts,
and 1/3 water) and blend on high speed. Voila! Looks just like cow’s milk
and tastes very refreshing. And NO additives!!
–
Also, eating the ‘lower FP’ foods such as jasmine rice (great also to
make in the evening, blend it in the morning on high speed for
‘rice puree cereal’ – and also such veggies as bok choy – these changes
add to the incremental healing process for SIBO – the results I am
experiencing are just a few days of a healthier, lower FP approach,
and already there is symptom reduction.
–
I am a very cautious person by nature – slow to take on experiments
and changes! These changes are incremental, they are non-threatening (!)
they do *not* result in pain… one can introduce a new low FP and then
see the results in the next 24 – 48 hours. It’s a very thoughtfully presented
process in Dr. Robillard’s work. One understands not just the “how” but
the “why” – this is essential!!
Thank you, Dr. Robillard!
Reporting from ‘the field’ – i.e. – the kitchen!!
All best, LK
Wow, I hardly know what to say LK. Thank you, and thanks for sharing some of your great ideas on the site! Your kitchen sounds like a fun place. I need to try cashew milk. Do you keep the water they were soaked in as part of the milk?
Hi, Dr. Robillard – thanks for your note! I don’t keep the soaking water, as I’ve thought that if there’s anything that might be fairly ‘concentrated’ (I have no idea what) in terms of the soaking, that I should ‘start fresh’ with the water. The ‘how to make nut and seed milk’ advice online is to use fresh water. Perhaps there’s a reason…! Or it’s the ‘folk wisdom’ and it will be shown to have a reason…!
I have read regarding making jasmine rice to first rinse the rice to ‘rinse off extra starch…’ (?) I’ve followed that advice… but don’t know if is logical..?
Logic, folk wisdom, laboratory analysis, clinical evidence, plus trial-and-error… there must be an acronym in there (somewhere!)..!
: ) LK.
Makes sense LK. I always rinse rice too, especially glutinous rice.
Hi Torsten, Yes, you should be able to tolerate small portions of jasmine rice as well as dextrose. And green tea is fine.
Hello, I am on day 1 of my elemental diet and have a question. Since Jasmin Rice is fully absorbed, can I eat small amounts of Rice occasionally during the diet? Also, is it okay to drink one or two cups of green tea during my day. And last, is it okay to sweeten my shake with dextrose? Thank you for your time and for writing the book Dr. Robillard
Hi Norm,
I just got the IBS book & am looking forward to integrating the info! I recently realized I have SIBO-D, then I was fortunate to learn of the SIBO Conference, which I attended via internet. You mentioned you would be, also. So I am wondering what takeaways & impressions you have from it — whether you would comment here or create a new page about it. I learned a great deal & am glad I had the opportunity to attend.
Thanks, Jean
Hi Jean,
Great you got the book and also participated in the SIBO Conference. Unfortunately, I was not able to view the live event and will have to take a look at the recorded talks when I have a chance. I would love to hear your thoughts. I have seen Allison Siebecker speak in the past and most enjoyed her lecture.
I would have so much to say about it! A biggie for me is that there is a sense that this is a serious, lifelong disorder that must be managed with diet & treatment — and Dr. Pimental presented research that indicates autoimmune involvement.
Since I relapsed repeatedly on SCD, and did poorly when I tried a straight low fiber/residue diet & also straight FODMAPs — it will be interesting to see how I will do by combining yours w/ those diets. Right now, I’m on a very restrictive diet, and will add foods back in one at a time. I’ll keep you posted, but it might be a while before I know.
There was a sense by all that the conference was a real breakthrough event & they plan to hold it again next year. Maybe you could present at next years!
Fair enough. Thanks for the update.
I found this scholarly article about Splenda that you might be interested in reading. It makes me want to eliminate it from the Fast Tract Diet. https://www.ncbi.nlm.nih.gov/pubmed/18800291
Hey Brady,
I am aware of this study which was later acknowledged to be funded by the sugar industry – who doesn’t like Splenda much. Personally, I am not overly concerned with these marginal (when you have 20 million bacteria, a drop to 50 to 80 percent of the control is still 10 million to 16 million bacteria – does it matter?) or inconsistent (weight gain was higher at a lower level, then decreased at a higher level, then increased again at an even higher level of Splenda) results. And since it was done with rats, is it relevant in people?
But no one knows for sure. Despite extensive testing, FDA approval and use by so many people around the world for quite a few years, there could always arise some problem that no one expected. I certainly respect your decision to remove it from your diet if you think it could be a problem for you. In that case, dextrose or alcohol-free Stevia are low FP alternatives.
Hi Norm…. miss aloha here…
I’m really trying to get better on this diet. Can I do a green drink it’s organic powder and has no additives.. just greens and a little ground flax seeds. I did it for years once a day then stopped to see if it was creating the symptoms but didn’t make a difference. i’m just having trouble with vegetables.. and I love vegetables.. Also for all your readers that work out and are athletes I found an electolite powder drink with no sugar…! it’s made by the same co that makes emeg C….
thank you for your time and integrity….
Aloha, Angela
Greetings Dr. Robillard and fellow readers!
I thought I’d report a few ‘successes’ regarding dietary changes. I had been putting soy milk in my morning coffee, and found soy was definitely a problem for me (perhaps not for others). I switched to homemade almond milk, and found it was ‘too oily’ for my digestion. I have found that homemade cashew milk, which is very easy to make, works perfectly well in coffee and has the consistency of milk.
–
I’ve also switched from broccoli (and even spinach and kale) to bok choy -just the leaves, very well steamed. This seems to alleviate symptoms associated with some cruciferous vegetables. I’ve been reading about soluble and insoluble fiber. Tomatoes, for example, have a combination of both. If you tolerate soluble but not insoluble, or vice versa, this can make a big difference on types of veggies/ fruit that can be eaten.
–
I’ve purchased some ‘pure beef gelatin’ powder – it has a whopping 9g of protein per tablespoon, and is used as a natural thickening agent. It can be put in liquids, added to soups or smoothies, etc. I am about to try it (it’s not supposed to be difficult if you have IBS-C or etc.) but will use caution. If it is a successful experiment (or even if not) I’ll report back here. For those of you struggling with nutrition and weight loss, or who simply need more protein, the pure beef gelatin may be helpful as it’s not a solid and still delivers significant protein. We’ll see… jury is out on this as of yet..!
–
Small changes…. these seem very good. A writer, Marge Piercy, wrote a book entitled Small Changes. A second writer, Grace Paley, wrote a book entitled Enormous Changes at the Last Minute.
–
Hm. Both exist in life… I think the small changes are for SIBO / IBS, we are the experimental subjects we read about!
–
Also, as Mark Twain once wrote “you can die of a misprint…” – so in anything I post here.. caveats abound!
All best, LK
can’t wait to hear!!!
Me too!
HELP! I am writing this in utter frustration and confusion about what’s gone wrong. So I have been told I have SIBO (though did not have breath test, only stool culture), as well as yeast overgrowth, mild adrenal imbalances, and a genetic issue called Gilbert’s Syndrome. Over the past two weeks I started a cleanse where I eliminated alcohol, sugar, dairy, etc. I was having protein shakes for breakfast with ground flax and either hemp or pea powder. I got horrific constipation, so I have switched to the Body Ecology plan for the past week, but now I have awful gas. Like, clear the room type gas. Been eating an apple for breakfast, followed by nuts an hour later or an egg. Lots of veggies, buckwheat groats, cultured veggies like kim chi, still no alcohol, dairy, or sugar, as I am trying to knock out the bad critters. Any ideas what I may be doing wrong? Would you see this SIBO approach being a better fit and if so, why? Does SIBO also address candida? I am SO frustrated!!!
Thank you so much for all that you do! Andy
Hi Andy, Sorry to hear that. SIBO symptoms can be miserable. I don’t make it a habit of critiquing other author’s specific diet, but your symptoms don’t surprise me given a few of the foods you mention that have high fermentation potentials. I think think Fast Tract Digestion IBS is a book you should read and implement ASAP. (unless you also have heartburn, then read FTD Heartburn). The diet limits all the hard-to-digest but fermentable carbs that drive SIBO and all the symptoms you mention. Since yeast feed on carbs also and make gas, the same principle applies, i.e., the diet will help with yeast as well. We also offer counseling if you want to jump start the process.
*We are starting a special, today I believe, where you get a free book if you sign up for counseling. Write to us on the consultation tab if you are interested.
Thanks for the quick reply, Norm! I had downloaded the book some time ago (and am kicking myself for not trying this out sooner), but had a question based on some of the general info I have read. It’s my understanding that by limiting foods that are not easily digestible, you remove foods that sit around in the gut and feed the bad guys. However, does this not mean that you are eating more foods that enter the blood stream quickly, spike insulin levels, and then trigger medical issues associated with higher blood sugar? I also can’t get the standard message of “eat more fiber” out of my head. Can you address the blood sugar question and the fiber issue briefly?
Thanks again! Much appreciated! And I will look at the counseling tab for more info.
Hey Andy,
Low FP carb choices will be either lower in carbs or higher in GI. To strike a balance while controlling FP, the meal plans in FTD books contain approximately 75 g of carbs per day, in line with the recently updated ADA recommendations for diabetics. Basically you’re limiting blood sugar by carb level as opposed to eating slightly more carbs having a low GI. Having said that, people with diabetes or metabolic disorders may want to consume even fewer carbs per day, but anyone with gut issues should not be choosing high carb/low GI foods IMO.
I know the fiber message is deeply in”grained”. But fiber simply did not live up to the claims either in terms of general health benefits or GI symptom improvement. Most types of fiber will make IBS, GERD and constipation symptoms worse.
hi Norm…
Also wondering about Chia seeds as i have IBS -D.. and they absorb water… am i thinking properly?
thank you….
Angela
Angela,
If you want to try some and see, just be sure to add the fiber grams to your daily FP levels, because while the fiber might absorb some water, the more important consideration is it’s fermentability. If you go over the recommended FP levels, all bets are off.
are sweet potatoes in or out? and what are your thoughts on eco coconut kefir probiotics and bone marrow broths?
and I may be doing a sugar detox and eliminating all forms of sugar including fruit.
Good direct questions Stella. Let’s not waste time : ) Sweet potatoes within the FP limits, kefir, probiotics and marrow broths Ok. Let us know how your sugar detox goes.
Thank you. Im soo glad I found you. I just researched yesterday that fructose could be causing digestive illnesses says WebMD. That’s why I wasn’t getting better and my stomach felt like it would digest bricks, even when I was dairy and gluten free. Cutting out fruit will be challenging but sure worth it I believe, and my inner guidance system tells me this is what I have to do.
Happy to be in touch Stella. And you don’t need to cut out fruit, just stick to lower FP fruits or smaller portions of the higher ones. We just had a great breakfast with some cubes of cantaloupe on the side. Delicious!
Parsnips, celery root, carrots, beets, daikon, and turnip are not tubers. They’re roots.
Thanks SB! I made the correction.
Hi Norm!
I am very happy to finally arrive at diet that alleviates my symptoms through almost 20 years (African parasites, waves of penicillin cures, IBS alternating btw. moderate and severe symptoms, classical story sadly). Your ebook is just the kind of scientifically reasoned narrative translating into a quite easy to use dietary instruction I (plus the rest of the world I guess) needed. Even the logic of the program is simple, that a layperson as me had no problems of picking it up instantly. Thank you from the bottom of my heart. Symptoms are gone within a week, which is nothing but amazing. Still on the diet, of course.
Now my question is: I feel an intense weariness (in no way unpleasant, like when having symptoms in the old days a week ago, though, but at kind of comfortable sleepiness, that does not go away with sleep). Is this a known phase in the diet (perhaps stemming from an impaired uptake of nutrients, energy, vitamins/minerals or what have you?)
Further, I have ordered betain HCL from Sweden, plus enzymes, all Thorne. At least plan to go with the HCL. My thinking is low stomach acid as I experience some burping after meals and traces of undigested foods in the stools.
Do you have any thoughts on the weariness, respectively HCL/enzymes? Anything would be highly appreciated.
Hi Frank,
Very happy to hear your GI symptoms have improved on the diet. As for feeling weary, that’s a question I rarely encounter from people on the diet. To fully address this, I would need to have more information about your situation. We have a consultation program if needed, but here are a couple of ideas. One possibility is that you came down with some kind of viral illness and it will pass. Next, I would look at the ratio of fats, carbs and proteins and possibly try a few adjustments. The Fast Tract Diet does not limit the actual levels of overall carbs, proteins or fats. So those parameters can be adjusted still keeping to a low FP diet. Sometimes when people go on a diet, they limit calories from one food group but don’t increase calories from another and end up with a calorie deficit.
You could also try adding a vitamin/mineral supplement if you suspect you are not fully absorbing nutrients- undigested food is a sign of some level of malabsorption. This may be from residual gut damage from all the years you had symptoms- it should heal in time if this is the case. As for stomach acid, you could try betain HCL if you suspect that, but generally that’s not an issue for healthy people (but a possibility in elderly or certain H. pylori positive or people taking PPI or H2 blocker meds). Getting tested would not hurt.
Norm, this hitting nail on the head and timely. I just had multiple testsvto reveal a nasty strep ba
Bacteria infection, yeast issues (was dominant on gets but present) , major gluten intolerances, dairy allergies, etc. I am wondering if is sibo I am dealing with? Symptoms are similar to Candida but I don’t have heartburn, just bloating, bad gas, among myriad of other symptoms related to overall 5.8 body pH. How do I start? Will buy the book but may need some more hand holding. BTW, I don’t do many carbs now, but I do eat brown rice bread (yikes) and I did eat a lot of carbs in the past. This stuff happens for a reason – finding you!
I was also very low in good gut bacteria. Some of them reported as NO GROWTH! Strong allergies to Gluten, casein, dairy, milk
Great to have you here Chris. Give the IBS book a read and check out the forum for questions and discussions.
Norm, thanks so much for all your guidance. I’m just getting my 5-year-old son started. He has severe GERD. Of course, sweeteners help a lot, so I was wondering if Barley Malt Syrup is a good choice since it’s mostly maltose?
Good question Joel, The FP is based on 75% maltose (GI 100), 16% glucose (GI 100), 6% sucrose (GI 59), and 2% fructose (GI 20). I get about half a gram of FP for a 14 gram (about two teaspoons) serving. Not too bad at all.
Great. Thanks so much, Norm!
Hi again, Norm,
I’m wondering about tapioca starch. We got a gluten-free white rice bread (Ener-G brand) that has white rice as the first ingredient and then tapioca starch. My son has been eating very low FP for the past few days and is still having bad acid reflux, so I’m trying to figure out what’s causing it. Also, if a product says white rice, does that usually mean white Jasmine? We’re also trying Trader Joe’s brand of Rice Crispies, but maybe that was a mistake. Thanks!
Joel,
Unfortunately, most processed rice products are made with long grain rice with too much amylose. Often times the FP is relatively low due to the extensive processing, but you’re still better off with jasmine or sticky rice which can also be used to make a creamed cereal. Also, limit the quantity if symptoms persist. Pudding from tapioca is also not a bad choice.
Ok. We’ll cut out the packaged rice bread and cereal and see how that works. Thanks again, Norm – I really appreciate your book and your help!
Hi Norm,
Just want to thank you for an outstanding job on this Low Fermentation regime. I’ve been struggling with a flare of IBS/SIBO (the ibs had been in remission for some twenty years) for a couple of years now, and did not find much consistent relief with the SCD, FODMAP or GAPS diet. The often painful distension, bloating and chronic C drove me nuts, yet I couldn’t control it. Just 36 hours into this regime, and the worst of the bloating and all of the pain have subsided (hope this remains!). I also want to commend you for running such an excellent blog, responding to questions, etc. Much appreciated. If I could get this thing under control, finally, life would be much better (one can’t help but worry about underlying issues constantly, as bloating and pain may indicate more maligne ilness, too).
Regards,
Lou
Thanks Lou,
Very happy to hear that your condition is improving on the diet! Stay in touch. Reducing FP should help greatly with IBS C as methane-producing organisms, which are generally to blame, rely on hydrogen for fuel. Therefore reducing hydrogen with the Fast Tract Diet should reduce overall methane gas and help alleviate constipation. If you should have any more issues with this, please consider our consultation program. We have a variety of tools to deal with this issue.
Hi Norm, I have some questions for you. I dont know exactly what my diagnosis is because I havent been to the doctors but Ill explain my symptoms.
I have to start with the fact that I was prescribed 1 benzo and 2 atypical antidepressants for insomnia, I understand that a lot of benzo receptors are in the gut, thus my gut was compromised.
I became severely constipated, fast forward to quitting the pills and trying to heal my body with nutrition that included lots of fiber, especially during orthodox lent, eating beans that were not cooked/ prepared correctly, eating lots of nuts, back then wasnt aware of the anti-nutrients contained in these 2..
So my current situation is that I can not tolerate fiber, I get extremely bloated, have lots of flatulence and belching. Used to have cramps also but found relief with activated charcoal.
Its not a clear pattern also, sometimes I get cramps from eating say raspberry, other times I dont, but generally cant tolerate green beans, beans, cabbage, broccoli, cauliflower, garlic is absolute no no, seem to tolerate just fine potatoes, rice, pasta, avocado, meats, eggs, fats, dairy.
Tried gluten free and grain free, saw no improvement, actually maybe even worse.
Can not eat vegetables without bloating and can not lose weight either, I came to the conclusion that the 2 are somehow linked.
Now, I dont know what exactly is wrong with me, is it sibo/libo or what, and can I find it in the book?
It seems also like bloating runs in the family…my mother and her sisters couldnt eat salads without bloating and gas seems to run in the family as well.
I too had moderate bloating and gas in the past that became much much worse after the pills and the excessive nut consumption.
I am better off eating refined carbohydrates, I want to eat a healthy diet but my gut just cant take it.
Also, dont have problems with milk, be it pasteurized or raw.
Also used to spice my food with lots of black pepper, now Im trying to reduce it although I love it.
Thanks.
Hi Lu,
I feel for you. I can’t address your specific situation in these comments, but the symptoms you are describing are consistent with SIBO/dysbiosis and some of the foods you list can make things worse for sure. Fast Tract Digestion IBS will answer many of your questions. If you need more info, feel free to contact us via the consultation tab and also check out the forum on this site.
Thx for your reply, If my situation is illustrated in the book I’ll buy it..I just dont want to see again avoid gluten and/or grains because gluten/grains do not create problems for me.
Lu- Your situation sounds pretty much like mine. I struggle with mostly constipation with massive bloating and intestinal burning. Started just as a fiber intolerance, morphed into a fruit and veggie intolerance, then went into slow starch intolerance as well. You should look up FODMAPS, because this will go from your large intestine up to your small intestine and develop into SIBO. I follow FODMAP and SIBO diet together.
God bless.
Thx for your reply, Angela.
I checked the diets you recommended and I agree partially with them..I am so confused because I have no symptoms from dairy so dont know if its a good idea to avoid it since I dont get problems from it, same for grains..its tough.
Do you have improvement on your diet?
God bless!
High lactose dairy avoidance or supplementation with the enzyme lactase is recommended for people who are lactose intolerant. Sound’s like this won’t apply to you, but many other foods have potential to induce excessive fermentation by gut bacteria. The book uses a new system called Fermentation Potential to get excessive fermentation (and symptoms) under control.
Agree with most of your recommendation, I have used SCD, GAPs and FODMAP diet for many patients. I have always know that all starches are not created equal and resistant starches are recommended for those individuals with blood sugar issues. That being said, I am a little shocked that you would even recommend splenda as a sweetener alterative with studies indicating a negative effect on gut flora, gut pH (by increasing) amongst other side effects. Could you please explain your rationale. I only recommend stevia if a patient really needs to add something sweet.
Hi Dr. Nalbandian,
Thanks for bringing this up. I understand that some people are concerned about the safety of Splenda. I assume you are talking about this study: https://www.ncbi.nlm.nih.gov/pubmed/18800291. For people who are concerned with Splenda, I, also recommend Stevia, as well as dextrose (powdered glucose) and erythritol – one gut friendly sugar alcohol.
I personally feel Splenda is safe and use it myself. My opinion is based on the many published safety studies and regular use for almost 15 years in millions of people. I view the above study with a pretty big grain of salt as it was paid for by the sugar industry, done in mice (relevance to humans in question), has conflicting data (lack of a dose response) and has been discredited other scientists. You might take a look at this review of the study: https://www.ncbi.nlm.nih.gov/pubmed/19567260. Also, here are a few other links on the subject: https://www.ncbi.nlm.nih.gov/pubmed/22579627. And this: https://www.snopes.com/medical/toxins/splenda.asp. And the New York Times piece: https://www.snopes.com/medical/toxins/splenda.asp.
In the end I respect people’s individual choice on the matter. Luckily there are other alternative sweeteners.
Hello, great work on your book FTD IBS. I bought your book and am implementing suggestions to my diet. After 8 years now of suffering with GERD I have tried countless diets and varying treatments. A 2nd trip to ER with terrible *D* attack – landed me with a gastro at Cedars that treated me for SIBO with Pimentel regime. The good news with the antibiotic treatment is that it allowed me to finally get off PPI’s – but 3 years later I am still suffering with IBS-C mostly.
I believe I now may have candida as well and recently switched enzymes to Bitters since I read that may help and it does seem to be helping. But a try at probiotics only brought back those SIBO symptoms again! Now I am back on a berberine (Goldenseal does wonders for me). Will have to get off that soon and what I am afraid off is all the symptoms coming back slowly as they have in the past.
I feel it’s true what has already been said that SIBO won’t stay away unless you can control 2 things. Enough acid (if your problem is you don’t have enough) that may be my problem – and you tackle MMC because most us SIBO suffers struggle with that. For me I am going to switch enzymes to see if one with HCL will help a bit more than bitters but I am stumped on help with constipation (probably caused by slow MMC). Currently am using flax seed in my gf cereal and I read above that you constantly suggest doing away with any fiber. What are your suggestions for a possible transition? After only one day off of flax and I constipate badly. Have you heard of Triphala? The FP restriction alone does not seem to be helping in this area.
Thanks so much for your great book and time.
Hi Dr.Norm.
Finally i got you’re book and read it,started the diet and i do not understand the nausea on low carb diet.I can get past the tiredness the brain fog poor focus and motivation but the nausea is baddd.i read that on low carb many people experience nausea and bloating belching,well i am one of them.
So Dr.Norm my question is did in you;re experience did u noticed nausea on low carb?and should i stay on the diet and “fight” this nausea?i can do that but please tell me it’s gonna end someday.I am on low fat also i try to keep protein up(lean chiken breast) and some veggies fro you re book.jasmine rice for now is a no no,also dextrose(i weight train) i keep low!!what o u think?
Hi Bogdan,
While I can’t comment specifically on your situation without more information via our consultation program, I can provide some general feedback. The Fast Tract Diet is not high carb or low carb per se. But rather a way of eating that limits harder to digest carbs that can be fermented by gut bacteria as that process is the biggest single driver of IBS/GERD and other functional gut symptoms. That being said, higher carb low glycemic index carbs have a higher fermentation potential and should be limited (not eliminated). If you choose to minimize lower FP (but higher GI) carbs (for instance rice, dextrose, etc.), the calories need to be made up (typically by healthy fats). People who limit both carbs and fats get into a bind because eating excessive amounts of protein is not the answer. You end up not consuming enough calories which could cause a variety of symptoms including weight loss.
PS: Bloating is almost always the direct result of gut bacteria fermenting high FP carbs.
If you’re getting cold hands and bad sleep, maybe you should eat more food.
Norm,
Ive started reading your book in relation to SIBO, it is a fantastic find I think it really gets to the root of the problem everbody else misses and that is that anything that does not digest fully quickly and smoothly could cause problems even if they are considered healthy (beans broccoli etc.)
I also read “Fiber Menace” you might have heard of it…but that book changed my life and following that eye opening info I really improved lots of my symptoms.
Your book has just given me even a little more knowledge in the ongoing battle Thank you!
I want to also point out to you and all commenters on here that I was tested for stomach acid levels a while back and I was diagnosed with mild case of hypochloridia (low stomach acid) and ever since I started correcting this issue(use of betaine hcl and raising Sodium, correcting zinc and iodine defficiencys) my stomach acid levels are improving and so are all my symptoms!! better than ever!!.
Through much research and even talking to my GI specialist we both agree that a majority people that have any digestive issues have this low stomach acid problems! He sees it in Countless patients.
Again Thanks for the insightful book!!
Thanks Carson for sharing some important insights. Keep reading. There is a section that discusses low stomach acid and other underlying conditions that can predispose one to SIBO.
Hello Carson,
I was curious what test did you get for stomach acid ? I asked my GI for something like that and he shrugged it off and said that he doesn’t test for such things – it’s more Naturopathic.
I am going to seek out another GI in hopes of finding a more integrative Dr – but it sure is difficult.
Getting this SIBO under control has been the most difficult thing I have tackled thus far.
What is your opinion of coconut milk, coconut butter, and coconut milk kefir (dairy freee)?
Do u think fermented foods like coconut milk kefir, Raw kraut, and Apple cider vinegar can help heal sibo/parasites/dysbiosis, or do u feel it makes it worse? I’d love your take on this, as there is a lot of conflicting info
Thanks for all u do!
Hi Stacy,
I’m chiming in to say that in my experience, fermented foods and probiotics are key to repairing and rebalancing the gut. I don’t think following the low FP diet alone does enough. However, by following the Fast Tract diet, eating cultured foods, and taking probiotic supplements, I’ve been able to completely stop taking PPIs and acid reducers, eliminated reflux, and have much better digestion and health overall. This is one area I hope Dr. Robillard will research further and add to future additions of the Fast Tract series. You not only need to starve out the “bad” bacteria by reducing fermentables; it also helps to consume “good” bacteria that will out-compete the baddies for resources, so the excess die off. Look for foods and probiotics rich in various strains of lactobacilli, Saccharomyces Boulardii, Bifidobacterium infantis.
But hey, don’t my word for it. See what some others say:
https://chriskresser.com/beyond-paleo-6
https://www.simplywoman.com/probiotic-superfoods-that-can-change-your-life/
https://www.mindbodygreen.com/1-9331-1/top-10-probiotic-foods-to-add-to-your-diet.html
https://balancedbites.com/2011/03/bites-i-love-fresh-raw-sauerkraut-a-probiotic-food.html
https://www.amazon.com/dp/0553384198/ref=pe_385040_30332190_TE_M3T1_ST1_dp_3
Thanks Christina!
The controversy I’ve seen has been that if there is an overgrowth of bacteria in the wrong place, that probiotics/ferments can contribute to this imbalance by not going to where they need to go (ie, due to MMC issues, or colonizing where the overgrowth is, etc). Also, they can also be a food source to any underlying parasitic/dysbiotic situation, thus making the infections worse
Also, many people with dysbiosis have a hard time tolerating histamine foods like ferments
A hallmark sign of sibo/dysbiosis is not tolerating probiotics or ferments
However, I’ve also seen the sources u’ve sited and others whom feel ferments and probiotics are key.
Some say leaky gut is healed with probiotics and ferments… Others say it can make it worse….
So, it’s hard to know what to do!
Did u have issues tolerating ferments and probiotics at first, or did u experience relief right away? I’d love to see what ur daily diet/meals look like too and how much/what fermented foods u eat. I’m thrilled u are seeing results, so any examples u can share would be helpful indeed. Also, how low carb/high fat are u?
Hi Stacy,
I didn’t have any trouble tolerating fermented foods or probiotics right from the start. In fact, around the time I started Fast Tract and transitioned off of PPIs, I also started taking Nature’s Way “Reuteri” blend probiotic capsules, which I called my “anti-heartburn pills” because they seemed to help taken on-demand when I was having symptoms. They actually contain a small amount of prebiotics (fermentables) to feed the probiotics, but they seemed to help rather than hurt overall despite this. I’ve also taken MegaFoods brand probiotics, which don’t contain any fermentables, but I ended up switching back becuase they don’t seem to be entertic coated (which helps the probiotics get past stomach acid unharmed).
Many people say that fermented foods are more effective than pills; I’m not sure, so I do a bit of both. It’s not always easy to remember to include them in your diet, and they can be expensive if you aren’t making them yourself. Kefir is especially good because all the lactose has been fermented out of it, and 24-hr. (“SCD”) homemade yogurt is great for the same reason. I eat those with low FP fruits (strawberries, melon) or make smoothies (avoiding bananas and other high-FP fruits except occasionally). I started eating kimchi and sauerkraut with eggs, meats, even homemade fried rice. Foods like miso paste, pickled green beans, cultured beets, sour pickles, cultured cheeses (camembert) etc. are easy and delicious to work into the diet here and there. You can even ferment your own foods with Caldwell’s starter and a Primal Kitchen Boss Pickler jar – it’s simple and kind of fun: https://primalkitchencompany.com/index.php?route=product/product&path=77_69&product_id=64
https://www.picklemetoo.com/2013/08/02/review-and-giveaway-the-boss-pickler-from-primal-kitchen/
A continuous brew of homemade kombucha is cheap and healthy, too. It contains B vitamins and other nutrients that help with digestion and support the liver, gut repair, etc. It’s fizzy and the sour taste grows on you. I like sour beers for the same reason, although you do have to be careful about FP; don’t go there until you’re feeling better.
You asked about diet. When I first started Fast Tract, I followed the dietary recommendations pretty closely. I am a big home cook and didn’t end up using the recipes much, nor did I measure/weigh foods for FP religiously. I just tried to eliminate high-FP foods, strictly limit the moderates, and make the bulk of my diet low FP foods. Now that I have GERD under control, I still try to eat low-carb/low-FP, but I’m not strict about it. Jasmine rice is my main starch, but I’ll occasionally have a bowl of pasta, a noodle bowl with rice noodles, or a hunk of baguette or crackers with cheese. I drink more beer than I should…and sometimes I pay for it with heartburn. It’s a trade-off, but at least now the symptoms are under control and I understand what sets them off.
Hope this helps!
The thing is i really need calories because i weight traing and i train preety hard so yes i will try to get them from good fats.The thing is fats makes me even more nausea i think my gallbladder is meesed up(it runs in family).
After gym i take some dextrose and whey protein and have some chiken breast thorugh the day with some green salad and cooked peeled carots.
So if u have some ideeas of fat i mean i know olive oil is ok for gallbladder.I tried some raw fish but i get headaches and it’s not ok.
I am tired of waking up with brain fog,i think that is my biggest problem of all and that is why i started this diet and bought the book.I really need to be focus on my studies and exams so i cannot afford brain fog poor memory focus and flu like symptoms next day after weight training.I know these symptoms are all relating to bad fermenting bacteria but it was verry hard for me to give up te carbs.
So i am on this road and the “die off” is really bad like i need to be strapped to my bed,craving for sweets and big meals , killing me also the depression and fatigue..
I wait for a sign of impovement…If u have other ideas of simple meals ok for gallbladder post it ,it would be great!!
Hi Bogdan!
Maybe a coconut oil can be an option for you? It doesn’;t need bile to be absorbed, so it doesn’t affect gallbladder.
I have problems with gallbladder too (“lazy gallbladder”, low function) and i have GERD. It seems that coconut oil doesn;t bother me much but i am not sure though…
Maybe i should lay off the meat for a while or eat maybe 2 or 3 times per week.But i don’t know with what to replace the protein if there is no more meat.
I can tolerate maybe 2 eggs per day and i use wehy protein isolate i ask Norm if that is ok with this diet.
When i first got this stupid gerd thing i eat a lot of meat per day maybe 1 kilo chiken breast plus 2 protein shakes and as a carb i used brown rice and some dextrose and raisins.so it was preety clean diet for 3 years and i always keep asking myself how in the world i got this terrible disease that i can get rid of anymore.
Maybe it was the stress in my life at that time or the suplements(i took many suplements like creatine vitamins glutamine testosterone natural enhancers etc).
So maybe there are a few over here that lay off the meat as a protein source and the question is should i?the effects after eating meat are burping meat like taste imediatly after eating,belchind and after 4 hours u cand still find meat in my stomach..
It’s ugly..
I thought it was hypochlorhydria but i took betaine HCl made things worse..
So i must gut up and be strict on this diet as long as i can( like a warrior :))) );
Hi Bogdan. I feel bad for you as I know all too well how challenging GERD symptoms can be. You may need individual consultation allowing someone can evaluate the specifics of your diet. In general, you can lower your overall protein levels. Body builders often consume quite a bit. Typical protein levels can vary quite a bit (15-35% of calories). You might try lowering your protein levels and also switch out some meats for fish, aged cheese or even plant-based proteins such as tofu for example (noting that some people have concerns about soy-based foods). You would make up the calories with low FP carbs and fats, perhaps leaning towards healthy fats more than carbs.
Hi can you give me some guidance – I have sibo caused though surgery and radiotherapy. I also have a stoma and borderline short bowel so I have been told to follow a low fibre high fat high protein diet. I have to take in a lot of calories and do this by having a lot of fats carbs and sugary foods. I’m sure this is worsening my symptoms but I’m so confused what I shd eat that will provide enough calories and be nutritious. So far taking metronizadole which really helps with wind and bloating. I’m now starting to try Prescript Assist broad spectrum probiotic . I don’t understand the term FP either thank you.
Hi Ren, Sorry to hear about your current challenges, but there is much you can do to improve your situation. FP stands for fermentation potential. The Fast Tract Diet is consistent with the advice you have received, but low fiber doesn’t go far enough. I suggest you read Fast Tract Digestion IBS that explains how to limit gut fermentation while upping your calories. You can also get more individualized support under the consultation tab and connect with others in the forum.
Hi thanks so much ill get the book and give it a try. Best wishes
Thanks Ren. I hope you find it helpful.
i was told i have sibo and wondering if untreated what are the side effects other than feeling crappy and bloated ;) like, malabsorption….?
and what if i become pregnant and have not treated the sibo yet…….
i do plan on getting our book, but i just stumbled upon this site 10 min ago ;)
In addition to what you mentioned, SIBO can cause altered bowel habits (diarrhea / constipation), acid reflux, and malabsorption of various vitamins, nutrients and minerals that can have a significant impact on your overall health. Better to get it resolved before getting pregnant from a nutritional point of view.
Hi, I came across this site while searching for information about IBS because I think my nine month old suffers from it. I realize this information is geared toward adults but I am hoping it could help with my son’s issues. He has had issues with constipation and obvious distress/discomfort with bowel movements for months. The advice I get from the doctor is to give juice (pear or prune) and fruits etc. which helped initially, but he would go right back to having issues. Now I am thinking all the fruit and juice (and increase in fiber) is the opposite of what he needs. Recently he was on Amoxicillin for an ear infection and by the end of the ten day course he was having regular easy bowel movements and was happier than I had seen him in a long time. As soon as the antibiotics were finished he went right back to having issues and a more cranky state. Now he is on Lactulose for the constipation (which also worked initially but doesn’t seem to be making that much of a difference), but should he be taking that if he has SIBO? He is already on a limited diet being nine months old, should he be eating the rice and oatmeal baby cereals? I can’t stand seeing him having so much trouble, I really appreciate any help or advice I can get.
Hi Kim,
I think your suspicions are correct in that hard-to-digest fermentable carbs could be a big part of the problem. The same goes for modified formulas and cereals. As for lactulose, it’s 100% malabsorbed and can absolutely exacerbate overgrowth and symptoms. You can share the Fast Tract approach with your pediatrician to come up with a lower FP strategy.
I have had stomach issues pretty much all my life, however the last 4 years have been the worst. I’ve suffered from acid reflux, hear burn, flatulence, bloating, pain, nausea…diverticulitis..you name it I experience it! I tried I low fiber diet…but with my low bowl, its hard. I did the FOD diet, but didn’t see much improvement.. was gluten free and dairy free, but then I became constipated.
Now, I eat dairy and wheat in moderation, plus I eat root vegetables, hardly any fruit or sugar… coffee one a day, I feel a bit better, however… I’m still bloated and uncomfortable. I ate fries the first time in years… and a week later I’m still suffering. So mo fried food.
I think your finding is correct…
But in.my case what should I do? To be able to loose weight..and feel healthy.
So many gastro doctors just prescribe drugs for acid reflux, that’s just a bandage! I’m afraid of a leaky gut… and what’s going to happen when I age? I’m only 40!
I feel frustrated and alone.
Marilyn
I really feel for you Marylyn. Just one of the these painful conditions can be challenging, but when you have two or more issues going on together, it can be too much to bear. Good that you are under the care of a doctor to rule out any serious (non dietary problem). So many people suffer with functional gut disorders from following typical Western dietary guidelines. I recommend that you read Fast Tract Digestion Heartburn and follow the dietary and behavioral recommendations. You may also want to read chapter 6 carefully on underlying conditions that can contribute to SIBO and share this information with your doctor. If we can help please contact us under the consultation tab on this site.
hi..let me tell u my symptoms first :
diarrhea, acid reflux, skin problem, anal fissure, pain at pelvic area on and off, flank area on and off, pain at the left n right abdomen (on and off) , mucus in stool, indigestion.gas, bad breath.
i’ ve met specialist, he diagnosed I have Ibs, he only did colonoscopy, we didn’t analysis stool, breath, urine, blood and etc… I consumed all the medicine he gave, but after 3 days consumed those medicine, my symptoms get worsen..vomits, very frequent diarhhea, gas, headache, fatigue, lack of water.. after that I stop took those medicine.. and about the my pelvic pain, urine test showed its clean.also my blood pressure.it means my kidney healthy right? I’m really mad to the doc.. he wasted my money, all those medicine is quite expensive, im only a student! ever since, i never believe to doc.. I did research by my own, i really think I have SIBO.. I consumed supplements; peppermint-ginger plus shaklee, energizing soy product esp shaklee, my symptoms improved.. but till now, i still having skin problem, gas..my diarhhea had stopped, but sometimes constipate ( on and off ), sometimes I got anal fissure. I was about to take natural remedies to cure it like apple cider vinegar..it is ok? please help..im still studying.. I’m dying everyday.. I suspected my SIBO because of food poisoning untreated well 4 month ago.. and i never have ellergy before, i can tolerate all kind of food..i also have g6pd deficiency..what shoud I do?
Hi Emily,
Sorry to hear about your challenging symptoms. If you do have IBS / SIBO I recommend that you read and implement Fast Tract Digestion IBS. That’s a cheap and easy way to impact any SIBO-realated symptoms. In order for me to get involved with your individual situation, you will have to enter the consultation program.
Hello Norm,
I just came across your website and am so glad to have found it. I ordered your book this morning but am a little desperate for some help in the mean time. I was diagnosed with SIBO last week, specifically a heavy overgrowth of Citrobacter Braakii (and another species). I am on day 5 of the GAPS Intro diet, and am now concerned that some of the vegetables I’ve been eating (carrots, butternut squash and zucchini) might actually contribute to the pathogenic bacteria. Can you tell me which vegetables would be the best to consume given my situation?
Thanks so much! I look forward to reading your book when it arrives.
Amy
Also, if you have any supplement suggestions (I’m considering taking berberine), please let me know.
Thanks again!
Just discovered your book and plan to order it. I have a couple of questions I hope you can help me with in the mean time.
Been constipated for 30 years. Had my first painful attack 6 years ago in the upper right quadrant of my abdomen. After many attacks and many doses of Cipro, which stopped working, my doctor diagnosed diverticulitis. He removed a 6 inch section of my lower left bowel. Felt great until I started eating again after surgery. That’s when I realized it was food related. I cut out gluten which made me feel better. Been gluten free a year. I did some research and decided I probably had candida and bad bacteria in my colon so I began taking oil of oregano, garlic and thyme supplements along with probiotics. Also cleaned up my eating habits. Worked fine until 2 months ago. I started to feel like I did before any surgery and supplements. Pain is back, I feel irritated in the bowel region, have enlarged lymph nodes and I’ve had flu-like symptoms for a month. More research sent me to this website. I suspect SIBO.
My questions: I have been drinking a smoothie of almond milk (unsweetened) and a scoop of Garden of Life Raw Meal every morning for many months. Is that ok? Can you give me your opinion on the Raw Meal? It seemed to be ideal for getting extra nutrients into me. Should I continue it?
Also, I have been reading about biofilm in the small intestine. The theory is that that’s a good reason the bad bacteria still looms as it’s “protected” from my supplements. Should I begin taking supplements to dissolve the biofilms? Should I continue with probiotics?
Thank you.
Hi Kathy,
Gluten free is a good idea to try. I would skip the Raw Meal meal replacement. The FP (fermentation potential) for one serving (two scoops) is about 25 grams – too much. Current probiotics are not that great. You can try them, but I really think you would benefit by reading Fast Tract Digestion to tie it all together. Diverticulitis is also linked to SIBO.
Norm, I had an initial consult with you in January. I spoke to you about my long term problems with severe die-off symptoms and enquired about the lack of discussion about die-off in your book. You said that you would write something about die-off and post on your website. However, I have looked numerous times and cannot find anything. I have you written about die-off. It continues to be a major problem for me when ever I try probiotics, peppermint oil, or other herbal anti-bacterials. (I have been on your low FP diet for about a year.)
Hi Carolyn,
I do recall discussing this with you, but I don’t recall saying that I would definitively write something on this (sorry if I gave you that impression : ( ). As far as I know, there is very little hard science on this theoretical phenomenon (correct me if I’m wrong). While dietary changes involving fermentable carbs will alter bacterial populations over time, I am not aware of any findings demonstrating a sudden massive die-off invoking symptoms after dietary alterations, though it’s theoretically possible. Even if this did occur, I would imagine that a new equilibrium would soon be established with bacteria that can ferment the new dietary fermentable substrates becoming established. After the new equilibrium is reached, if you don’t change your diet (in a significant manner) again, why would this continue to be a problem?
PS: I feel bad that you are still having some GI issues. I took another look around and did multiple searches on the PubMed data base with the terms: bacterial die-off, herxheimer reaction, and herxheimer diet, etc. I literally can’t find a thing on this, though symptoms that could relate to die offs following broad spectrum antibiotics are reasonably well documented. I wonder if trying to stabilize your diet and making changes gradually might help if this is happening. Alternatively, something else might be going on.
Dr Robillard,
Guess that I was not clear. I do NOT have die-off when I change my diet. The nausea, extreme sleepiness, headaches, chills, cold feet, and flushing that put me in bed and prevent me from going to work for 3 to 4 days come within hours after I have tried to take any brand of probiotics, or non-prescription herbals such as peppermint oil, grape seed extract, berberine etc. Again, not related to change in foods.
These Herxheimer or die-off reactions are discussed in medical literature in the treatment of Lyme disease, syphilis, typhoid fever, and a few other diseases that involve the toxic reaction to killing of bacteria and release of endotoxins. Several of my medical doctors acknowledge that this is reported somewhat frequently with patients who appear to have SIBO and try to treat with probiotics and/or herbals and/or Rx antibiotics.
I would appreciate any comments that you have and/or suggestions regarding this reaction. Give up on probiotics and/or herbals?
Carolyn, it may be worth investigating histamine and salicylate intolerance (which can stem from SIBO and increased gut permeability) and can often be mistaken for die-off symptoms.
Most of the herbal remedies you mentioned are high in salicylates. And the probiotics you are taking may contain histamine-producing strains. (D-lactate producing strains can also make one feel worse – see Dr de Meirleir’s research.)
You could try making your own yoghurt from non-histamine/d-lactate producing bacterial strains.
I see Caroline. Yes, I am aware of reported Herxheimer reactions associated with antibiotics, but not with probiotics or herbals. But if you (and your medical doctors) think that’s a possibility, perhaps it would wise to stop using them for a while and see what happens.
Thanks for the rapid reply. I ordered your book and am looking forward to reading it. Hasn’t shipped yet from Amazon. In the mean time, I have been consuming ginger kombucha daily. Without having your book yet to consult, I am wondering if I should continue this.
Kathy, Do you have the nutritional facts for this drink? If so, what are the total and net carbs and dietary fiber?
30 calories /serving
7 g carbohydrates
2 g sugar
0 protein
Assuming there is no fiber or sugar alcohol present, a rough estimate of FP is 3.5 grams.
Greetings, Dr. Robillard and fellow readers. I have confirmed SIBO, IBS, and also slow motility… bad combination!! I have worked on dietary issues for many months. I thought I’d share a few ideas: I’ve found that high fiber is a definite “no-no” and there are ways around that. I also don’t eat anything w/ lactose – with various ‘workarounds.’ I was struggling with how to keep up nutrition each day and losing too much weight. I started to make chicken ‘gel’ – boiling chicken on the stove in a ‘fast boil’ for 2 hours, and refrigerating the chicken/ broth overnight. With that approach, a thick gel forms, which is enormously ‘soothing’ to the stomach and also a great source nutritionally. Also, I make cashew nut milk, specifically, as it is the lowest fiber of the nut milks. And… a product to mention (no affiliation whatsoever) is Cabot Cheese (VT-made) – there is no lactose in the cheese making process, and I am able to tolerate the cheese. Additionally, ‘beef gel’ that can be purchased in powdered form has a very high protein content and easy to digest. This, plus eggs, and steamed tomatoes (w/ skin peeled off) are staples of my diet. I’ve discovered taking the skin off most foods that I can eat (e.g. Idaho potatoes, blueberries, tomatoes etc.) helps as the IBS doesn’t get triggered. Overall, it is one food at a time and see how it goes. I’m sure most of the readers can relate to that idea!! Trial and error, within the limits of low fermentation potential, low fiber, and high nutritional value. One exception to ‘no skin’ is that chicken skin (boiled) is enormously soothing to the stomach and seems easy to digest. Of course- everybody is different – that’s the beauty of human life- and the glitch! :)
All best, Laura
Hi Laura,
Thank you so much for sharing your research and experience on the Fast Tract Diet. Very helpful indeed! I may have to experiment with skinless veggies myself.
Hi. I’ve been off PPI for about 8 yrs. now, I have them sent with meds every month.
Lots of ER visits with chest pain, all ruled out and pointing at stomach, first with h. pylori in ’98 . . . currently all symptoms point to severe water brash (excessive salivation) caused by GERD, constantly spitting out saliva to point of frustration. Little food, no stamps or cash, living on olive oil, eggs, challah, one chicken/wk and what is donated in wkly. box from JKshrOrg. On eve. meds for ImmDis; started PPI again today, out of desperation. Alone in Queens, NY. 1 cup of coffee in am, green tea rest of day. I think I might benefit from GERD surgery, female over 50, etc . . . nausea from eve meds, flatline all day —
Hi there! So happy to have found your website with all the great information. I had a question about SIBO for anyone. Do you have a lot of abdominal pain with it? I feel like I have this gnawing feeling around my belly button all the time. When I wake up in the morning it isn’t there until I eat and later in the day its so bad I’ve had to go to emergency a few times. Im 24 years old and never leave bed, they still can’t figure out whats wrong and they put me on hydromorphones for the pain. I am waiting to get a breath test and a smart pill at the end of July. I talked to my GI doctor today and she said she hasn’t heard of anyone having abdominal pain so bad they had to go to the ER with SIBO so I was curious if anyone can relate to me or knows that this pain can be associated with a severe case! I am so desperate for answers as to why I am hurting so badly and having so much trouble eating. Thank you so much for any responses.
Hi Norm
I stated your diet in January, I believe.
Definitely I feels better than before, when heartburn ruled and reigned over me. The problem still when I eat cheese, yogurt, cream and even lactose free milk. Can I use any substitute for milk, dairy is not for me.
I can not eat even the fruits that you recommend nor squash either. Sushi rice occasionally is more less okay.
Thank you, I’m thankful for your books.
Hi Megan,
The pain you describe is exactly how my reflux started. I would get this searing pain in my stomach, in the area around my belly button and where the ribs meet at the bottom. It was so severe I had to leave work several days. OTC acid reducers didn’t do much; Prilosec helped a little. I had an endoscopy showing a mild case of gastritis and some irritation. Prescription Prevacid helped quite a bit, but symptoms would flare, especially during periods of stress, and I’d get desperate and have to double up my dose. It was awful. And whenever I forgot to take my Prevacid? Searing stomach pain and (new-t0-me) acid reflux/GERD. It sucked.
Then, when I tried to get OFF of Prevacid because of some of the health risks of long-term use (brittle bones, pregnancy dangers), I had full blown GERD and even silent reflux (where you feel like you have constant post-nasal drip). Horrible rebound reflux–and I bet the PPIs had helped exacerbate the SIBO by eliminating my stomach acid.
The Fast Tract diet was the solution for me. It took a while, but the diet protocol combined with probiotic supplements and probiotic foods has gotten my reflux under control and completely eliminated the stomach pain.
How can I be sure? When I cheat too much and eat or drink too many fermentables, the symptoms come back. Let’s just say I am regretting the carby meals and beers I’ve been drinking lately!
Hi Christina
How long does it generally take for your symptoms of GERD to calm back down? I have been on the diet for a bit over a month, stopped taking ppi when I started tbe diet. It was going mostly ok, but about a week ago i had a flare up. It is still hanging around, despite being very careful with my diet……. Any advise/anecdotes welcome.
Hi Dr. Robillard. I just discovered I have SIBO — both kinds of bacterial overgrowth in very high counts. Its possible I have had this problem since I was a small infant. I developed pneumonia and severe gluten intolerance at age 4 months to the point I stopped growing. At the hospital they put me in isolation and discovered about the gluten problem thankfully. More than likely I was given antibiotics. I was also given gamma globulin to beef up my immune system. Of course no probiotics. This was after all nearly 65 years ago! when no one knew about the dangers of antibiotics.
I discovered years later I had been exposed to radiation from the Green Run at Hanford nuclear power plant coincident to my first getting so ill — and was exposed to another run of radiation when I was two years old plus likely plutonium from drinking boiled river water (my parents were working as archaeologists there in Washington State not that far from Hanford).
I was put back onto gluten by the time I was 5 since by then while being on wheat I was finally able to grow. After that I was ill a lot and often had this brain fog–but no one thought anything of it.
My abdomen seems like it has always been distended even though I am not otherwise heavy. Plus my sinuses are even now nearly always stuffed up despite whatever I have tried to do to remedy the condition. And I have also had more migraines than I’d care to recount. Even though I now eat a low histamine diet and use detox herbs pretty regularly I still get the migraines, though certainly not as often. I discovered last Fall Wormwood really helps my digestion, which was the beginning of my realizing that I had pinworms since the wormwood eventually brought the critters out.
Going off grains recently after getting rid of parasites seems to finally make my abdomen look more normal. So I finally suspected that I had SIBO and I was right.
Even though I do not have IBS or GERD etc. I have had very low energy and am an inveterate night owl. White tongue etc. RLS and jumpy nerves especially at night. Itchy Fragile scaly skin in my nether region and ears — though it has been getting better, especially since I got treated for seemingly intractable pinworms.
My question was why is it so hard to get rid of the critters?? The answer seems to be this SIBO. I do seem to need to use fiber however otherwise I experience constipation. But after seeing what you describe about the Fast Track, I am intrigued. Maybe it would work for me.
I was on a modified paleo/SCD diet since neither diet by itself worked for me that well. Honey and cheese etc. put me into a completely altered not very happy space. But combining the diets creatively seemed to be OK–though I used sunflower seeds rather than almonds (I seem to be sensitive to all nuts).
My doctor wants me to go on a SCD diet again now we have discovered I have SIBO.
But two years ago I discovered I have extreme sensitivity to Histamine/Amines. This makes going on a diet without white beans (my one reliable food) and eating bone broth and 24 hour yogurt instead problematical–though store bought plain organic yogurt is fine (for two days after opening the container).
However I am hoping that by taking refraxamin I will become a little less histamine sensitive and can thus eat more chicken. I will also be using antibacterial herbs — which should agree with me since herbs actually do agree with me very much and I had been taking one form or another of them for years due to my kidney sensitivity. I lost half of one kidney due to nephritis, likely due to the gluten I was eating plus having had a hobby years ago making wine. I have been using h for 40 years minus two years I thought I had salicylate sensitivity. The herbs in fact saved my life since otherwise I would have had to take antibiotics continuously for my kidney problem. As is, I almost never have a problem with them. Maybe once every ten years or so I get a run in with it. The last was when I was testing out my gluten sensitivity and discovered I had zero tolerance for gluten from the wheat family.
Already now I can eat fresh (and then quick frozen to stop the amines) chicken more often than I could previously due to having killed off most of the parasites. Using antihistamine herbs such as basil and rosemary and ginger really helps me tolerate the chicken better too. Cucumbers also help.
Interestingly, during the two weeks prior to my SIBO breath test I started eating rice again since I figured I needed to be able to eat something more than chicken once every other day, ditto with an egg–both of which I am sensitive to due to the high amines. Previously I had stopped eating rice for a while due to killing off the parasites protocol. I had no fiber supplements (or any supplements at all for that matter) those two weeks preparing for the SIBO test and was not constipated. So your theory seems to be very possibly true. Especially at the last when I was eating white rice.
So I want to buy your book and discuss it with my doctor. It seems so antithetical to everything I have believed about diet all these years, but who am I to go against true observation??
I was after all on a self imposed SCD/Paleo diet for two years following taking ciprofloxasin for what turned out to be simply a skin condition rather than an actual infection in my ears. I had terrible diarrhea every half hour for a month after the cipro. This was back in the Fall of 2009. To survive I used my herbal knowledge and drank olive leaf tea and lived on 24 hour yogurt for two months. Such fun and games. After that I went on the SCD/paleo diet for two years as mentioned previously. The itchy condition continued however.
Finally I thought I had salicylate sensitivity but in the end it turned out to be this histamine problem instead. I am grateful for the comparatively improved diet! Going on a partial GAPS diet helped me discover my histamine problem. Eating home made sauerkraut really brought out the histamine sensitivity to its utmost! But while I thought I had the sal sensitivity I was just eating the white rather than the brown rice…. And it was OK. Hmmmm!! So yes I want to buy your book and see what my naturopathic/acupuncturist/TCM doctor and I come up with. Any comments you might have for someone a little outside the box of the usual IBS GERD would be helpful.
Hi Pamela,
I think it was about 2 1/2-3 mos. of following the diet, taking probiotic supplements (Nature’s Way Reuteri or MegaFoods MegaFlora) and eating probiotic foods before I felt like the reflux and stomach pain were really fully under control. Definitely be strict with yourself and try to identify any “slips” that trigger indigestion. I never measured FP strictly because I tried to stick to low FP foods, but you may need to exercise portion control if you eat in the moderate and high range. I suggest avoiding them entirely as long as you can stand it.
And definitely explore whether probiotics might help you. Just looks out because some contain prebiotics (fermentables) that might cause problems. The Nature’s Way Reuteri actually contains some oligosaccharides (I think), but somehow never really caused me trouble.
Hi Norm! I feel like I know you! I’ve been following your blogs, podcasts, RS exchanges with TaterTot and Richard (love the civility and respect in these debates!), and I have just ordered the IBS book for me, and the Gerd one for my brother. I have been diagnosed with both SIBO (hydrogen type) and candida overgrowth in colon, so it’s challenging to determine proper diet, whether probiotics are best (apparently, good for candida, not good for SIBO), and whether I should tackle the SIBO first or the candida.
Ae you still against the raw potato starch idea? I’m really at a loss. Your diet sounds good for SIBO, but not so good for candida. Any thoughts? Thanks in advance! Your willingness to personally respond to all these strangers is pretty darn impressive!
Ha Jan. A great beach day and then your wonderful comment. Can life get any better? Probiotics have a mixed track record for both IBS and GERD which will likely improve as new / better strain combos are developed and tested. My general thoughts on SIBO and yeast is that both bacteria (SIBO) and fungi (yeast) ferment undigested carbs and produce symptom-causing gas. Theoretically either type of overgrowth should respond well to limiting fermentable carbs. So I don’t recommend raw potato starch to begin with. I recommend that people that want to experiment with prebiotics do so after they get symptomatic relief on the Fast Tract Diet. Thanks for following my stuff.
I have been thinking on your book for a while. This discussion is definitely helpful to me. Thank you Dr. Robillard! I have overcome alot of health problems (some of my story is here: https://www.familyhomehealth.blogspot.com/2014/06/food-as-medicine-for-incurable.html) Digestion and food intolerance is the one thing that I feel still needs some work. I seem to be sensitive to histamines, and have trouble with fermented foods or slow cooked beef broth (bad bloating/buzzing in extremities/insomnia). I also recently ate alot of white beans as an experiment and had bloating/heartburn/sinus drainage for about a day afterward. Actually it seemed worse the next day after I had been eating the beans. I was diagnosed with a mild case of SIBO recently through a breath test. I was told by my previous doctor that I had yeast overgrowth (which does seem to correspond with mercury poisoning which used to be an issue but many of those symptoms are gone). I was wondering what your recommendation would be. I have considered taking black walnut or maybe goldenseal. Although a previous commentor mentioned that goldenseal might be high in histamine. Would you say do the fast tract diet and then take some kind of herbs later? I have been reading recommendations to take the herbal “killers” first and then do something like the scd diet. I read that the scd diet can make the bacteria “hide” so it is best to hit it with the antimicrobials first and then do the diet. But my experiment with the navy bean makes me think that your diet might be more appropriate for me than the scd. Also probiotics are tricky with histamine intolerance. I was wondering what would I need to do to heal my intolerances completely. I took out dairy around 4 years ago, but would love to try some butter again but was waiting for my last symptoms to be gone before bringing foods back. Basically, how can I get my good bacteria to win all the time, and therefore not have problems with histamines or other foods?
Hi everyone! I have had all the symptoms of SIBO and I recently had a breath test, still awaiting the results but I was wondering what is considered positive breath test. Many websites say anything above 20, is this true?
That’s correct Megan, according to Pimentel, “a rise in breath hydrogen 20 ppm above basal levels within 90 minutes after ingestion of lactulose should be considered as diagnostic of SIBO.”
Here’s a paper on the subject:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3155069/
Hello! I just finished your IBS book and found it very informative. I have dealt with IBS for almost 25 years (I am now 43). Two years ago I was diagnosed with SIBO. I received the diagnosis without the breath test because the hospital where I had to have it done had never heard of the test before.
I have read through the other postings, and the symptoms list in your book, but neither are exactly what I am experiencing. Here is what happens to me during an “episode” (and I apologize in advance for the level of TMI in the description):
• I belch a sulphur taste and then immediately suffer intense fatigue.
• Over the next 4-5 hours the sulphur taste intensifies to an unbearable level, and flatulence is very frequent.
• Then the diarrhea starts – 15-30 minute intervals of constant flushing – pure liquid and the strong sulphur taste.
• Usually during this time the vomiting begins.
• This will continue anywhere from 5-20 hours.
These “episodes” occur anywhere from once in 6 weeks, to 3 times a week. I’m starting to worry about keeping my job with all the sick days I’ve had to take.
I tried a low-fat diet, a high-fiber diet, and finally a wheat-free diet. None have worked (in fact I agree with your conclusion that the high-fiber diet made things worse). I am going to begin a modified version of your Fast Track diet tomorrow. Modified because I am still staying away from certain foods so I am going to use your tables to keep my FP 20-30 grams a day, to start. I am crossing my fingers that it will help.
Have you ever heard of these episodic symptoms linked to SIBO?
Hi Heather,
Given the significance of your symptoms including bouts of vomiting, it’s important that you are under the care of a physician. There is lots of research going on concerning the role of sulfate-reducing-bacteria (SRBs) in gut health and chronic fatigue. Limiting hydrogen gas formation on the Fast Tract Diet should help control overgrowth of these types of bacteria. If you want some help delving into this deeper, please contact us under the consultation tab.
I found this article online about your book on SIBO. I am currently being treated for this although I have had no definite test results. My symptoms began suddenly almost one year ago. My husband and I went out for sushi and three days later I was in the hospital with shortness of breath and excessive gas. They said it was a panic attack. I know that it was not because I am no better. I have been to my Pcp, a GI, and my endocrinologist with no luck. ..currently my symptoms are excessive gas both upper and lower 100x per day, intermittent diarrhea, dizziness and just an overall weird feeling. HIDA scan, endoscopy, colonoscopy all normal…. I am an uncontrolled diabetic, have hashimotos and had a thyroidectomy last year, and hysterectomy. Does this sound like SIBO..also I am achy and itchy all the time…please help me
Given your symptoms and the fact that they landed you in the hospital, you should really be under the care of a physician. SIBO is consistent with excessive gas and autoimmune conditions, but shortness of breath is not a typical SIBO symptom. If interested, I can consult with you and your doctor through our consultation program.
hi norm,
I want to ask whether it is possible to SIBO caused a histamine intolerance. I have been diagnosed with histamine intolerance, lactose intolerance, and I suspect for SIBO. it, however, I have not yet been tested.
Thank you for your response.
aneta
Hi Aneta,
Interesting question. I’m afraid I don’t know the answer. I would be interested in hearing what others think.
nevertheless, thank you very much for your answer :-)
I was diagnosed with a mild case of SIBO and highly suspect histamine intolerance. I have alot of blog posts about it if you want to follow along on my health discoveries. Here is one of my post on histamine intolerance: https://familyhomehealth.blogspot.com/2014/04/waking-too-early-and-liver-health-low.html. I have low histamine menus on my blog also: https://familyhomehealth.blogspot.com/2014/05/a-menu-plan-for-low-histamine-low.html. PS I have bought Norm’s book and I have been working some on implementing it.
Hello, I’ve been dealing with SIBO for the last couple of years after falling off the GAPS “wagon”. The symptoms were somewhat sudden but I’ve had other autoimmuneish symptoms most of my life. I recently got tested for SIBO and it was positive, however, it was at the same time I found out I was pregnant. I’ve been hesitant to do anything but am clearly having worsening symptoms, mostly at night. I don’t get reflux much (although it has happened on occasion now that I’m pregnant). I do have unbearable gas, burping, etc. When the SIBO started a couple of years ago, I tried the apple cider vinegar and it seemed to do something because it made me feel pretty sick but as I’m sure you know, this seems to be a long term, committed solution to get relief. Anyway, my question is, given that I’m pregnant and that heartburn is not really the issue (although I’m sure it will become more of a concern later), which diet do you think may be more beneficial? Also, what do you think about the use of apple cider vinegar during this time? I will of course be talking to my doctor but I just thought it would be nice to get your perspective as you obviously have so much experience with this. Thanks for your time, looking forward to hearing your thoughts.
Hi Michelle,
Gas and burping are consistent with excess intestinal gas and SIBO. I recommend you read Fast Tract Digestion IBS or more information. A bit of apple cider vinegar won’t hurt if you want to try it, but it can irritate the esophagus. Take a small drink of water afterwards.
Hi Michelle, I’m pregnant with SIBO and wondering if you have any advice now that you’ve been through the process? I’m terrified of nutritional complications and the resulting health of the baby. I would love to hear your experience and what if any expertise you may have acquired in the process?
Bit confused about one key point. The test most often used today for SIBO is the glucose breath test, on the principle that small bowel bacteria will ferment it. Does this not run counter to the fundamental principal of your diet/book? Most “elemental diets” seem to face the same paradox, and based on experiences I’ve read, don’t seem to be too effective. Thoughts?
Interesting question Jon. This is why most breath tests now rely on lactulose. Glucose will detect SIBO in significantly fewer people precisely because it’s rapidly assimilated into the blood stream. But the fact that it can detect SIBO in some instances suggests that either glucose absorption is poor in those individuals or the bacteria comprising SIBO in those cases have advanced into the very early part of the small intestine. I suspect the latter is the most frequent cause. This also the reason that I recommend, in the Fast Tract Digestion books, limiting even the easy-to-digest carbs early on in the diet – for example only 1/2 cup of jasmine rice. I also talk about limiting even glucose in the troubleshooting sections if you’re not responding to the diet.
Dear Norm,
It is heart warming to see how everybody is trying to help each other.
I have just been diagnosed with SIBO too. I am already on the SCD diet for 3 weeks now and I feel improvement. I was recommended to still eat some rice to keep weight. But I always have troubles after eating the basmati rice. I read in your post about rice. I will try and see if sushi rice would digest different.
Because I prefer not to take Rifixamin the dietians have advised me to do the Elemental Diet 028 (Nutricia) for 2-3 weeks to starve the bacterial overgrowth and than return to the SCD diet. I find it hard to find good information on the Elemental diet. I have tried one drink and I can handle it. I was just wondering what the positives and negatives are of this diet. Can it make Candida worse? I have not done a Candida test or parasites test yet? How long would it take to have the bacterial overgrowth under control with your diet ‘The Fast Tract Diet’? Thank you for your answer. Kind regards,
Sofie
Hi Sofie,
Welcome to the site. The elemental diet can be quite effective for people with SIBO and Candida, but I would not recommend it for the long term as a whole foods diet is the healthiest in meeting our (complex) nutritional needs. SIBO should respond to the Fast Tract Diet within days. Full recovery depends on identifying and addressing any additional underlying factors that contributed to SIBO in the first place. The Fast Tract books and our consultation program can help with this process.
Hi Norm (if I may). I have schleroderma causing both gastroparesis & rapid emptying! I have constant bloating, vomiting and reflux. I take 40mg Nexium twice per day. I am also currently TPN fed through venus access so bypassing my gut (for the past 4 years). I have had SIBO for years and have had it confirmed by a breath test. I have taken two courses of Rifaximin, both of which have only given about a weeks relief from SIBO symptoms. I am now waiting for a follow up breath test but suspect either the SIBO was not sufficiently eradicated or they have returned. I understand that you have to wait for 4 weeks from the finish of the antibiotics before the breath test. I have also had a cycle of about 6 different antibiotics back to back which was also unsuccessful in providing relief. I take VSL3 probiotic. I now have a gastric pacemaker & hope to return to eating in however limited a fashion that can be and weaning off TPN. There is next to no dietary info available even though gastric pacemakers are becoming more common in the UK. Would you recommend your diet for reducing my SIBO? Any thoughts about my condition would be greatly appreciated as although I have several wonderful GI specialists none of them can recommend a diet as this situation is thankfully quite rare. Any guidance would be much appreciated.
Hi Jay, Thanks for sharing your challenging situation. You are certainly not alone. I am happy to hear that you have some good support from your GI specialists. You might discuss with them the possibility of transitioning first to an oral elemental diet and then to the Fast Tract Diet. The Fast Tract Diet is certainly supportive for SIBO, but your ability to tolerate solid foods will likely need to be closely monitored.
Hi, Have a query which may have already been answered previously:
I was diagnosed with Celiac disease about 2 years ago. Have been gluten free since (unless glutened myself by accident), but about 6 months ago I was also diagnosed as having Fructose Malabsorption aswell as SIBO. I am having trouble sorting a decent eating plan to deal with all the above at the same time – (and thats not so boring and tastes like cardborad!)? Can you suggest any ‘diets’ that would cater for ones needs? I find eating gluten free relatively easy, but the whole fructose/SIBO thing is another matter. Any ideas would be much appreciated. Thank you
Hi Rebecca,
What you’re experiencing is not unusual – 30% of people with celiac disease don’t make a full recovery on a gluten free diet. When the villi don’t fully recover, you can experience malabsorption of fructose and other carbs which feeds SIBO. Being extra careful to exclude gluten from your diet is important, but I think excessive amounts of difficult to digest carbs can be a big problem for celiac recovery. Recall that gluten free diets still allow unlimited amounts of dairy, fruits, corn, potatoes, rice, etc. Many of these foods contain too much lactose, fructose, resistant starch and fiber. The solution is the Fast Tract Diet being careful to exclude any foods/products containing wheat, rye and barley.
I discuss this idea in my interview with Patrick Timpone (at 1:19). We plan on releasing a volume of Fast Tract Digestion Celiac Disease one of these days. In the meantime, you can use Fast Tract Digestion IBS with the exclusion of gluten.
thanks for the book – great read. i suspect my sibo is returning and though i’m not on a strict diet i do generally try to stay away from FODMAPs. what are you thoughts on hemp protein powder? though it doesn’t give me any bloat or gas issues, it does suddenly seem to create an issue with hard stools.
Thanks Rm, I looked at the nutritional facts for Bobs Red Mill hemp protein powder. 2 tablespoons (14 grams) has 4 Total carbs, 3 grams of which are fiber. Using a GI estimate of 50, the FP calculator gives 3.5 grams. Not too terrible. But if it gives you hard stools, may not be worth taking.
Hi Norm
Thank you so much for your prompt response. Unfortunately i have been told that I won’t be able to tolerate an oral elemental diet as I cannot tolerate the volume needed to support me. I can only manage 3-5 mouthfuls of food (eg. yogurt) before feeling unbearably full and bloated. Here me out on this but in theory if I don’t eat anything for 3 weeks and am fed by TPN is this not the equivalent of the elemental diet in that the bugs won’t be getting fed and should therefore surely die? If I during that time had a 14 day course of Rifaximin coupled with Neomycin would that not zap the little nasties? In the past I have only had 7 days of Rifaximin which clearly didn’t do the job. If this is the ravings of a desperate lunatic please feel free to ignore me!
Even with TPN, bacteria in you gut will still feed on sugars which comprise mucus in your gut. But you are correct, growth will be depressed. As for antibiotics those bacteria that are susceptible to the antibiotics will die, others are not affected by the drugs and still others will become resistant. That’s why antibiotics are not a good long term solution.
.. sorry Norm I meant to then say I could then progress with the Fast Track diet to keep them at bay increasing the amount of food that I can tolerate slowly but surely. Thanks for the book, it makes rational sense to me.
Thanks for the quick reply. Below is a link to the brand i use, which at least suggests that it provides more fiber than the Bobs Red Mill version.
https://store.nutiva.com/hemp-protein/
Are there any protein powders that are dairy and gluten free that you would recommend?
Also, it’s been a couple of months since I read through your book, but is the FP calculation explained within? Is it necessary to do those calculations, or can people (generally speaking) just stick with the low FP foods at the back of the book?
Thanks again.
rm
also, what are you thoughts on probiotics and their potential to make SIBO worse? do you recommend the use of them, and if so any particular brand/type? if this is covered in the book, just let me know and i will go back for a reference.
thanks
rm, Probiotics and the FP calculation are covered in the book and there is an FP calculator on the site – see link above. But you are correct, you can also use the tables in the back of the Fast Tract Digestion books.
hi norm,
I want to ask you that is possible the symptoms SIBO includes occasional mucus in the stool? I also have problems for a long time, a few times a month to appear mucus stool, or mucus is just same, while stool is normal. I have diagnosed lactose and histamine intolerance. I do not eat lactose and avoid the histamine food.
Thank you very much for your answer.
aneta
Absolutely Aneta. Here is a link where mucous in the stool is discussed as a symptom of SIBO. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2691494/
thank you very much for your answer Norm. sorry, but I have not found discussion on symptoms of SIBO in that article.
“One hundred and fifteen of these subjects fully complied with Rome II criteria, i.e. (1) 3 mo of continuous or recurrent symptoms of abdominal pain or irritation that may be relieved with a bowel movement or coupled with a change in frequency or related to a change in the consistency of stools; (2) two or more of the following symptoms present at least 25% of time: (a) change in stool frequency (> 3 bowel movement daily or < 3 bowel movements weekly); (b) noticeable difference in stool form (hard, loose and watery stools or poorly formed stools); (c) passage of mucous in stools; (d) bloating or feeling of abdominal distention; (e) altered stool passage (e.g. sensations of incomplete evacuation, straining, or urgency)."
thank you Norm, I found it. But I thought it would be more described. thank you Norm, and I apologize for so many questions. Have a nice sunday :-)
Hi Norm,
Yesterday I was taking two tablets which contained lactose monohydrate (in weight maybe 0.3g) but I reacted as I would have eaten a very high FP meal. As I was eating very low (ca. 15FP the whole day) yesterday the only trigger could have been these tablets. Is lactose monohydrate a very hard to digest sugar besides it is lactose?
Thanks,
Mark
…and I’d like to add: these tablets had been solved already under the tongue. So I can’t imagine that the sugar traveled much through the intestines. So definitely a small intestine problem?
Hi Mark,
Lactose monohydrate is used in tablet manufacturing. It’s made by crystalizing lactose out of solution – so it’s essentially lactose and, in sufficient quantities, can lead to symptoms in lactose-intolerant individuals. In this case, it was a very small amount so you may be very sensitive to lactose or it was something else that caused your reaction.
Thanks Norm.
Hmm…I can’t say that I have noticed a strong sensibility to lactose (though it’s hard to tell because I am chronically constipated and have motility issues and don’t experience a lot of symptoms from food like gas, bloating or diarrhea). When I haven’t consumed milk products for a while and I consume milk I do usually get diarrhea the first time but when I consume it regularly after that the reactions disappear. Lactose breathing tests have always been negative.
Anyway I am trying again to get rid of my constipation with FTD for the second time. This time I am aiming more for 5-7FP per meal than 10 FP at the last try. Medications don’t work for my constipation and since being constipated for the last five years the stool always floats on top. I think it might be because of too much gas in which case the FTD should be effective eventually. Do you have experience value by now if people with IBD-C are taking longer to see results? Because I remember you once wrote that with FTD you should see results within the first 5 days. However the only obvious reaction from fermentable carbs ist that my exzema flares up (this is how I noticed the reaction from the tablets yesterday because my sking got pretty worse today) and gets much better with FTD.
Sorry for the long text. Have a nice sunday.
Hey Mark,
Constipation can be challenging because is has many causes. I recommend reviewing the chapter on underlying causes with regard to motility. And there is a strong correlation with methane producing M smithi. Contact us if you need some one on one help.
norm,
thanks for the answers to my questions last week. i went through most of the book again this weekend. couple of questions:
for SIBO specifically, is there any particular brand/strains, etc. of probiotics that you recommend. i’ve read that it can make sibo worse.
also, i didn’t notice quinoa on the list of FP foods. how does it score in general?
and last, any protein powders you can recommend (gluten and dairy free)?
thanks for your help!
rm
Hi Rm,
Though I can’t trace the glycemic index of quinoa to it’s original source, the quinoa.net site lists quinoa as having a GI of 35. If that is the case, a quarter cup of quinoa (dry) would have 28 grams net carbs and 3 grams of fiber. That would give an FP of about 18 grams. You can always try it and see how you feel – while controlling FP for other foods in your diet.
I am doing a more in depth evaluation of probiotics, but not sure when this information will be ready to post. In the interim, I recommend probiotics with strains that don’t produce gas from carbohydrates, for instance probiotics containing Lactobacillus acidophilus and Bifidobacteria. Here is a brand that contains these two organisms: https://trubiotics.com/choose-trubiotics.php
For protein powders, stick to brands with little or no sugar or starch. There should be very little, if any, carbohydrates listed on the nutritional facts sheet.
Hello Mr. Robillard,
I have read your book about GERD few days ago after cca 4 month with acute issues related with GERD. The main of my symptoms, the most bothering, is the persistent feeling of ‘lump’ in my throat. What is interesting, I have no hearthburn. As I was googling and reading on web about GERD, it seems that the cause of GERD is hypochloridia. Therefore I bought some HCL pills and pancreas enzymes, but the after a couple weeks, the ‘lump’ was still there. Then I read that the cause of GERD could be bacterial overgrowth due to much intake of some corbs and that the effective treatment could be paleo or scd or gaps or fodmap diet. But it was a little confusing, becouse I had been on paleo for all of 4 month and reflux was still there. The other diets are contradictory to each other with respect to kinds of carbohydrates. But I gave try to paleo with fruits and no complex carbs. This was not effective, fruits also caused and probably causing the ‘lump’ feeling in my throat. Finally I encountered your site and your book. So I am trying FTD now and hope that will effective, the concept make sense.
What I would like ask you is, how the high fat intake can influence the overall time, which chyme with fiber and carbs (and fats) last in intestines? I am asking because carbs intake alongside with fat decreasing the GI and it seems that this combination causes that malabsorbed carbs which was eaten with the fat will stay much more time in intestine and thus this combination allows more fermentation. What do you think about such consideration?
The second question is, wheter is it good idea to switch to entirely no (almost zero) carb and no fiber diet for couple of weeks to boost the effect of your approach? I suggest that this cause that the bad bugs which are after my SIBO will die much more quickly without any food. Am I right? Any “side effects” there?
And the last question deal with probiotics. Is it good choice to using some probiotics supplement alongside with FTD? Could not it leads to even larger bacteria overgrowth?
Thank you much. I am very curious about how I will do on your diet and what my ‘lump’ in throat will do…
Regards
Ondra
Hi Ondra, Thanks for reading. If you haven’t done so, you might want to read these two blog articles on acid reflux on this site. Fat can lower GI a bit and hence raise FP, but you’re still better off consuming low FP foods.
Early on in the diet, lowering fermentable carbs is always a good idea. I would not worry about going too low. Your gut microbes are also fed by animal products as well as sugars linked to mucous your own body produces.
I am doing a more in depth evaluation of probiotics, but not sure when this information will be ready to post. In the interim, I recommend probiotics with strains that don’t produce gas from carbohydrates, for instance probiotics containing Lactobacillus acidophilus and Bifidobacteria. Here is a brand that contains these two organisms: https://trubiotics.com/choose-trubiotics.php
Norm,
Thank you for all of your help. I had found a similar post on quinoa somewhere else on the site and got the feeling it was on the higher FP side – nonetheless, thanks for the answer. I must say that following the low FP food list has seemed to quickly make a difference in my bloating and gas after meals, even with certain otherwise high FODMAP foods (i.e. cauliflower). That said, and I may be simplifying things too much, but it generally seems that higher GI foods are preferable to yield a lower PF. i’m curious on your thoughts as it relates to spikes in blood sugar due to consuming higher GI foods (i am not diabetic and have no risk factors that i am aware of).
Also, can you opine on the following products? One is the probiotic i used to use and the other is a brown rice protein that provides a decent amount of protein with very few carbs and essentially no sugar.
and curious if you have an appropriate low FP gluten free bread you can recommend.
https://www.renewlife.com/probiotic-supplements/ultimate-flora-RTS-daily-probiotic-15-billion.html?utm_content=Ultimate_Flora_Daily_Probiotic_15_Billion&utm_source=bing&utm_medium=cpc&utm_campaign=TM_Probiotic&utm_term=ultimate%20flora%2015%20billion
https://www.nutribiotic.com/rice-protein-plain-3lb.html
thanks again for all of your help!
rm
Hi rm, Sorry, due to ongoing projects, I won’t have time to comment on the supplements you mentioned, but I did want to comment on your question about blood sugar spikes. Yes, low FP carbs have either low carb levels (blood sugar safe) or higher carb counts but higher glycemic indices (can raise blood sugar more quickly). If you choose the latter foods, they can raise your blood sugar. The best way to deal with this is to limit the actual amounts of these foods. The recipes in Fast Tract Digestion limit total carbs to about 75 grams per day. People who tolerate more carbs may consume more. People with metabolic syndrome, diabetes, etc. should limit the overall carb counts appropriately.
i understand. thanks for the reply
Hi Norm,
I have one hypothetical question. Patients with CF have often SIBO. because they often have blockage of the pancreatic ducts by thick mucus, which blocks the release of the amylase. and so carbohydrates are not absorbed and are a food for bacteria in the small intestine. would not help people with SIBO (without CF) preparations containing amylase? then the starch faster diversified into glucose and it could absorbed before it would eat bacteria. it is bed theory?
thank you for your answer., aneta
Great idea Aneta. Older research suggested that healthy people produced “adequate” amounts of amylase. But newer research shows that amylase gene copy number varies widely between people. That means that amylase enzymes levels vary widely as well. Supplementing with amylase therefore makes a lot of sense, as it could be deficient in more people than we previously thought.
I ask this because a lot of people have diagnosed with SIBO or have a symptoms, but they have not specific cause (eg CF or obesity). These people helped supplements with amylase…maybe…
What do you think? do you not recommend it?
I’m sorry, I ask so much, but I dont have yours books, but comming soon :-)
Excuse my English, I’m learning only a short time :-(
Thank you very much for your willingness to answer for my many questions, I appreciate it :-)
aneta.
Yes Anita, I agree with you. It is worth a try taking amylase if diet alone does not solve the problem or you suspect you may have a deficiency. As you will see in my book, I talk about amylase.
Hi Norm
Can you tell me why Dr Mark Pimmentel (sp?) states that we should carry on eating in a normal fashion whilst taking Rifaximin? Doesn’t this mean feeding the bugs that we are trying to get rid of? I am not sure I understand the theory behind this?
Hi Jay,
The strategy is based on the idea that actively growing bacteria are more susceptible to antibiotics. There is data supporting the approach, though I don’t have the references handy.
Dr. Robillard — I am desperate to help my 16 yo daughter who has been suffering with what I believe is SIBO for several years. Last year she developed a sinus infection and was prescribed Augmentin. She had great results and was symptom free for 5 months following the Augmentin. Then, problems resumed with a vengeance. She also was prescribed Rifaxin with little benefit. I would like to try your diet for her but I see that (at least week 1) contains many dairy foods. She is very sensitive to dairy since SIBO began. What can I do to help her? I really appreciate your help.
Hi Michelle, Low lactose dairy foods are used in many Fast Tract recipes, but there is no specific requirement for this and dairy foods can be replaced without consequence. I hope your daughter get’s well soon.
Hi Dr. Robillard –
Question for you: why would someone still have problems digesting low FP veggies if following the FTD-IBS diet plan? I’m following your diet plan (Oh thank heavens you wrote your book and developed this website. I had reduced symptoms in 24 hours and much more energy) but still having troubles with the veggies. I keep my FP starch to 1/2 c of jasmine rice/day so definitely not going over my FP daily allotment. Maybe more time to heal? Many thanks for your books. My husband found immediate relief with your heartburn book and I have had tremendous improvements with your IBS book. I could never figure out what was wrong with me (massive stomach pains, gas, bloating) and I was getting worse. I’m lactose intolerant and have fructose malabsorption so your diet plan has been an absolute dream.
Thank you! McCourt
Hi McCourt, Good that your symptoms have improved, but it could take awhile and some diligence to remove the most persistent breakthrough symptoms and perhaps further limit some troublesome veggies, even if low FP. For instance, some people react to even small amounts of onions, particularly if raw. Onions contain chains of fructose that can be a problem even in small amounts. Technically, those fructose-based carbs should be reflected in the FP value, but if you find onions (or other specific vegetables) cause you trouble, you might just need to listen to your body and reduce, or even eliminate them for awhile.
You are so kind to respond to my question. Thank you Dr. Robillard. I will be patient and continue to try every few days with small amount of veggies. Have a great weekend!
Hi Norm,
at first I would like really thank you very much for your research and your book. It seems that your conclusions about GERD and SIBO are absolutely right. I am keeping almost zero carb and fiber diet for six days today and my GERD symtoms are almost gone.
But I still cannot stop thinking about what had occurred before I entirely shifted to this zero carb and fiber diet. I had been keeping low carb (and high fiber due to a lot of veggies) diet for about one week and it was seemed that it works, symptoms had relieved. However, then, when I had took one small beer I immediately felt that symptoms are slowly coming back.
Next day I had been still keeping low carb diet, but with a bit of onion. Other day after I had wanted to try what will kombucha intake make, because I had been thinking, that add some good probiotics would be good choice at this time to helps good flora with struggle against the bad one bugs.
I am not sure what exactly was the trigger, whether beer, onion or kombucha, but after aforementioned sequence of food intake (there should be emphasize that overall FP during these days was not excessive), my symptoms radically striked me again.
So, the question from the story is, whether is possible that the yeast which contains both beer and kombucha may contribute to SIBO (only bacterial or yeast overgrowth as well?) and encourage the coming back of symptoms?
And my second consideration is regarding to gut flora restoration process after some time on FTD, when the bad bacteria have died. Given the fact that bad bacteria have died or at least the level is decreased, there opens a space, which could be colonized by good bacteria. What could be the proper protocol to due restoration at this level? Is it possible that SIBO could be caused in individual case by overgrowth of some of good bacteria strains? If so, I assume, that probiotics intake could be harmful in such cases and therefore one must be very careful with probiotics intake during SIBO healing, or it is all much more difficult?
Thank you very much for your notes!
Regards
Ondra
Hi Ondra,
Yeast from beer is likely not an issue (except home-made beer) as commercial beer is filtered. I suppose it’s possible that yeast from kombucha could persist and produce some gas. Interesting idea, but I am not aware of any studies on this.
As for restoration, it’s not always good vs. bad bacteria so much as bacteria out of balance or out of place (in the case of SIBO), but there are times certain undesirable strains of bacteria such as Campylobacter, Klebsiella pneumonia show up in higher numbers and can be problematic. There are hopes probiotics will help, but the clinical results are mixed. Newer / better probiotic blends and better testing of current probiotics will likely show better results as time goes on. Whether or not you take a probiotic, limiting FP is important to allow your body’s immune system, and other control mechanisms (motility, etc.) to clear out overgrowths and restore balance.
Note: I re-read your question and realize you are asking if probiotics can become part of the problem as bacteria die off. Some probiotics can cause bloating (which might relate to your question), but I don’t think its from a diet-mediated die off, because, at least on the Fast Tract Diet, there are still considerable fermentable carbs and animal-based fermentable material as well. Also, the host mucus feeds gut bacteria as well.
Hello, just got diagnosed with SIBO. My doctor recommended a diet similar the the one in Breaking the Vicious Cycle. Within the table of “Can Not Have” is beer. I took a beer brewing class a year ago and am researching recipes that use honey instead of sugar for priming the beer. Everything will be fermented. Most recipes call for wheat, malt, barley etc. Any thoughts on why brewing my own beer would be bad for my SIBO?
Thank you.
Lois
Hi Lois. Have a look at the nutritional facts for non-light beer. They have about 12-13 grams of carbs per beer which includes unfermented sugar and starch. The FP (Fermentation potential) is about 6 grams, which can add up if you consume more than one beer. I don’t know how to brew light beer, but I understand its a bit tricky. You might just limit consumption to achieve low FP goals.
Hey Norm,
I’ve had a rectal itch for years, have tried everything, and it’s now as bad as it’s ever been. Need help desperately.
I’ve cut out most of the carbs in my diet, but a few things remain: organic brown rice, kiwis (green apples made my symptoms virtually unbearable), and sweet potatoes/yams. Should I eliminate these as well? If so, what can I replace them with? Getting a sufficient amount of food has been a challenge after jettisoning the majority of my intake.
Hi Tyler,
You’re certainly not the first person to experience this condition, which can be caused by a number of primary or secondary causes:
https://www.medicalnewstoday.com/articles/168728.php
There is no guarantee that the Fast Tract Diet will address this condition, but it’s definitely worth a shot. The best advice I can offer is to get a copy Fast Tract Digestion IBS and give it a shot. Some of the foods you mention will have to be limited or removed.
have you heard of someone having a rectal itch in conjunction with a tingling in the toes and at the tip of the penis?
also get periodic breakouts of red blotches on each side of my nose right by the nostrils
I’m reading about your Fast Track Digestion IBS and am very interested as it seems to possibly be the answer to my many years of struggles. Curious though: does the diet cure the root cause or is this a way of eating that will need to be followed forever? If foods not on the list are eventually added in, will the SIBO symptoms return? Also, is buckwheat ok on the diet? Thank you!
Hi Celia,
Fast Tract Digestion uses the concept of “fermentation potential” (FP) and pro-digestion techniques to put the breaks on IBS symptoms. As discussed in this article, IBS is linked to small intestinal bacterial overgrowth which can be caused by consuming too many hard-to-digest (high FP) foods in general, the inability to digest specific carbs such as lactose or fructose, or involve other underlying factors discussed in chapter 8. So the answer is “it depends”. In most cases, a dietary strategy is required long term.
I take a 15 billion live organism probiotic daily. Is this helping me, hurting me or having no impact on SIBO at all?
Norm,
I have had some bad responses from eating jasmine rice, which I make sure to heat very well before eating and chew thoroughly. When I cut it out, the symptoms go away, but I have to eat a very low carb diet, and I feel very low energy, even supplementing with sodium as recommended. Have some of your other readers experienced this? If so, do you have any recommendations to resolve this? I may just gut it out and go VLC for a couple days, but I hope there is a better alternative I can try first.
Thanks,
Brian
Hi Brian, In cases of poor or damaged digestion, even simple carbs can be troublesome. Recall that some people with SIBO can be diagnosed with glucose. VLC for a week or two is a great idea in this case. Then try a small amount of jasmine again and see what happens.
Thanks Norm, I’ve started VLC and symptoms are disappearing.
Would Greek yogurt (not the low-fat kind) be a ok substitute for rice in small amounts? I’m looking for additional carbohydrate sources that are not starch but yogurt has lactose, so I was wondering if this would have less heartburn potential.
Hi, I am 20 this year and I have had horrible flatulence for over two years. It began in my second year of college when I was getting an average of 4 hours of sleep a night and was heavily dependent on coffee. This led to Acid Reflux and like loud noises from my stomach at random times. I would get hungry abnormally. I went to see a specialist who put me on strong antacid and prebiotics for two months. This made no difference to my monstrous flatulence. It not nice. It’s even worse in terms of etiquette for a girl.
I noticed that controlling my diet affected the odour. However, sleep over rides whatever I try to control thorough my food intake.
Meat products are a no-no, just like coffee and chocolate. I seem to be unable to digest dark chocolate. Cream, butter and cheese are other things I have to avoid. Noodles or rice cannot exceed more than the size of my fist. Or else the gas produced that day is really phenomenal. Like the sort that can concentrate a 6000 seating hall in 45 mins.
I wish I were kidding. Please at least give me the benefit of doubt.
If I don’t sleep at all or have irregular sleep on any night, it’s will be like a gas faucet. My stool samples show negative in bacterial or fungal infestation. No parasites in the liver as well.
I find my future or the possibility of any social life or job, let alone a career very very bleak and struggle everyday to come to terms with how disgusting I now am and must be. Doctors give no hope at all on the matter. Only look amused and incredulous and give terribly disheartening replies when I ask about a possible solution. Beans, cabbage nor radish affect me. It’s regular food I have a problem with. I no longer have acidity. It’s just.. Is is SIBO or any bacteria related thing?
Can that be affected by sleeping habits?
I also don’t have lactose intolerance according to tests. Nor I have Celliac’s disease. I am, understandably quite desperate to get rid of this. I would like to normal. And I was hoping the book would help. Is it possible for me to have SIBO based on the above observations ? Or is it something else? My doctor say I show no signs or bacterial overgrowth based on stool samples only.
Hi Adrita,
Intestinal gas is almost always due to the overgrowth or imbalance of microbiota. In the case of excessive flatulence, the imbalance is most likely in the large intestine and heavily dependent on carbohydrates. The Fast Tract Diet should address this issue effectively.
Hi Norm,
I have a particularly nasty case of SIBO. I was diagnosed, using the breath test about two months ago and took the Xifaxanfor three weeks. It barely worked at all. The doctor I went to here in Los Angles, is Dr. Rabhar, part of the Cedar’s Sinai team. I have a long history of a botched appendectomy when I was 20 years old. I am now 65 years old, but because I have really taken care of myself and eaten organic for as long as there has been organic, been physically active, do bio-identical cremes from plant based and a very clean base (Bill Altmiller at IHHS@aol.com) and have been a follower of a modified Weston-Price diet, people think I am a good 15 years younger than I am. Right now, I am experimenting with diet, to some degree and making my mistakes (the SIBO is still quite active). My job, as a small business owner, in a Hollywood entertainment company has its share of stress. I had my hips replaced by Dr. Brad Peneberg, three years ago and I am quite certain, I have had this condition of SIBO since. It was probably controlled, up to that point, since the botched appendectomy, when my ileocecal valve was damaged. I want to modify my diet and try herbs that will help. I also wanted to ask you about ozone therapy and your opinion.
Hi Susan,
Given that you have confirmed SIBO and that antibiotics were not successful, I recommend you read the Fast Tract Digestion IBS book. As an alternative, we offer individual consultation. I know of no scientific studies linking Roundup to SIBO or ozone for treatment.
Hi Norm,
One other point is a question I have regarding the chemical in Roundup and if this is a possible irritant that has caused this massive outbreak in SIBO.
By the way, before I made my way into my present profession, I spent three years as an executive recruiter. I recruited professionals for the biotech industry, back in the early to middle 1980’s, before it was totally taken over by Big Pharma. I found it very interesting to speak with and consult with microbiologists, molecular biologists, immunologists who were studying and looking for cures for cancer, AIDS and Alzeimers. I have a basic understanding of how our bodies immune system works or does not work, as the case may be.
Hi Norm,
I wonder if pan-fried potatoes do have a higher FP than simply cooked potatoes given that in your table french fries have a relatively high FP. Though we don’t know which potato cultivar was used for the french fries I guess.
Good question Chris. I don’t know the answer, but using low FP potato varieties to start with will likely yield better results.
Hi Dr. Robillard:
Reading this thread, you have referenced ‘weaning off PPIs’. First, do you mean to include all antacids with that including H2 blockers?
I was on Dexilant for 3 years. For the past year I’ve been on Pepcid 20mg/2X a day with an occasional Prevacid on days when I’m really bad. Honestly Pepcid is lame (kills regurgitation only) and does not do anything more than take the edge off. I feel pretty bad most of the time (pressure in chest behind sternum, bloating after meals, burping, constipation). Thus trying even HARDER to fix this with diet although at this point, I’m feeling grim about that.
Context: I’m 48, workout regularly, average weight. Diagnosed with reflux and IBS (which I did not have pre-Dexilant btw). Mild esophageal deterioration, no parasites, no food allergies, no hernia. Have tried Paleo (makes me dizzy/increases reflux), Fodmaps (works pretty well with IBS but no impact on reflux). I’m trying to avoid Elaine Gottshalk’s diet although I feel like I’m getting close to broth and chicken being the only thing I can tolerate (that said, on certain days ANYTHING I eat makes me bloat up – it’s weird). It’s depressing.
At day 5 on Fast Tract, I’m having Paleo like symptoms (dizziness/reflux) and can’t even imagine LOWERING the H2 blocker. If anything I feel I should double up or switch back to a PPI. The only thing I can think of that I’m doing wrong is eating too much fat. I accidentally bought higher fat cuts of meat this week. Today I’m moving to skinless white chicken – we’ll see. Any suggestions? The rice (which tastes fantastic!) seems to be contributing to constipation so after two days I sadly dropped that. My only starch the past few days is half a russet potato (cooked fresh each time). Still, I’m having really bad reflux and IBS symptoms. I’m also hungry. I’m staying under FP35.
Second question, given that I’m having such bad symptoms while on the diet do I need to be off any ant-acids/Pepcid for the diet to work? I couldn’t tell from reading. I’m tempted to try it but I really hate that acid feeling, already feel SO bad from sternum pressure – I feel like going off will make me explode. I looked at the text again last night and it seemed to say “when you feel relief from symptoms you can try to reduce”. I’m clearly not there. I’m not using your recipes b/c the GERD trigger foods seem to be very prevalent. I’ve been eating eggs, meat, cooked spinach/chard, cooked summer squash and zucchini and cooked carrots. I have a little scale and am weighing stuff. I had 5P of russet potato the last few days. That seems to feel okay. Also eating nuts (weighing them) and mozzarella cheese sticks for snacks. In desperation, I had Lactaid ice cream last night (measured it out) which helped me feel better (ice cream always helps me for some reason) but I still had a lot of symptoms overall the past 5 days. More so than usual? I think so. I’m keeping a journal. I seem to get worse as the day goes on. I always wake up okay but by lunchtime I just deteriorate.
Third question, the book says the average result is 1-3 days many people felt complete relief of symptoms. My body could easily be more messed up from so much PPI use. I want to give the diet a fair shot but also don’t want to torture myself. 2 weeks? Thoughts?
Anyone else reading have a similar experience? Should I stick it out? I don’t want to throw in the towel too early if some of you found it just takes a little longer! I really want to get some relief with diet but it’s hard to keep the faith when you feel so crappy. And I’m dizzy when I stand up – I do not like that. Is there some sort of die off period with this diet? Could it be that?
It’s so confusing. Given there is ‘nothing wrong with’ me other than reflux, I don’t get why my whole digestive system feels so bad and why it won’t calm down. My stomach’s never been fantastic but it truly tanked during the Dexilant years. That depresses me. I was shocked I didn’t have a hernia since I am not overweight, etc. But no dice. Any input is welcome.
I take the following for my digestion per my Doctor:
20 mg Pepcid 2X day
1000 mg Mastic Gum (Jarrow) 2X day (supposed to help gut, seems to totally help)
Align probiotic 1X day
DGL as needed (really doesn’t work)
Additional symptoms: chronic congestion and coughing/mucous. And I was diagnosed with Asthma last year. Also I get rashes (again starting only a few years ago). And yet, not allergic to anything. Not fun.
Thanks!
Hi Alexandra, Sorry to hear about your persistent symptoms. I was in your shoes once with chronic GERD on PPIs. Please consider re-reading the trouble-shooting section in the book that has been updated in both the ebook and print book. It can take longer to address symptoms in cases where damage is more significant resulting in more persistent malabsorption. Cutting fats is almost never the answer. I would up the fats and cut more carbs personally. While the diet works best with adequate stomach acid, you’re right that it’s hard to stop the meds if you’re still having significant reflux. We can help with this issue and your other concerns and challenges if needed via our consultation program.
Hi Norm,
I just ordered your book for IBS and currently using the tracker. I have been on Prevacid and Pepcid for last 14 yrs since my gallbladder was removed. I was always told that being overweight was the reason I had to take PPI’s. If I lost a lot of weight, of course, I could reduce them. I was on a round of antibiotics back in Nov and got severe heartburn, itching, mouth burning, etc. Had upper endo and Dr. said mild case of gastritis from Ibuprofen use. He increased my Prevacid to 60mg/day. Ugh He did the breath test in Jan and I have SIBO. He prescribed Xifaxan, which I was too scared to try. I was on strict diet from gastritis and was able to get the itching, and most IBS symptons to disappear, so I opted out of Xifaxan treatment. As soon as I felt better I tried regular diet, now all my symptoms are back! Not as severe, but annoying. I am scheduled for knee replacement in 5 weeks and terrified of not being able to take asprin (for clotting) & opiates for pain. So glad I found what is wrong with me, and hoping your book provides more help, but how long does it generally take to get rid of the bacteria with diet and do you recommend taking Xifaxan at first to get things started or just do diet alone? Thanks for any input! :)
Hi Norm,
I just got diagnosed with SIBO recently and I’m only 15 years old. I struggle with abdominal pain, gas and some diarrhoea. Its really confusing being diagnosed with something with food issues because I thought that I was healthy eating gluten free, sugar free and organic foods and very low amounts of dairy (only goats cheese) .My doctor who focuses on bringing natural therapies into traditional practices suggested the low FODMAPs diet and the GAPs diet. I read what it said about the FODMAPs diet promoting resistant starch? so maybe this diet isn’t for me? I guess its a process of trail and error. I am considering getting your book but I feel sorry for my parents having to pay for so much (doctor appointments, supplements, tests, more appointments etc.) with my condition. I hope you reply as I really would love your input. I am going to read more of your articles and hopefully get a better insight into my condition.
Also, which book would you recommend for SIBO patients?
Hi Kayla,
I recommend you read Fast Tract Digestion IBS. You might also be interested in the forum.
Thanks, i did buy the book off amazon so hopefully it’ll arrive soon :)
Hello Alexandra! I have the same name and also difficulties with implementing the FP diet. It doesn’t work for me fast too.
My situation includes not only reflux (with erosions) but also slow gallbladder.
I tryed with FP diet but it seems not to be so fast in my case. For some time i had to stop this diet. Now i decided to come back to it but with some modifications. I can’t say if it helps because it is too early…
So just to ask you – did you check the function of your gallbladder? It can make the situation more difficult to manage, because it provokes the growth of bad bacterias (there was a science work about it). In this case you need not only count FP but also improve your gallbladder and liver function.
In the of additional gallbladder problemes i advise you to read “Save Your Gallbladder and what to do if you’ve already lost it” by Sandra Cabot (Author), Margaret Jasinska – it is very informative as additional to FP diet.
Weirdest breakthrough that I’d like to share with your readers and ask if it might shed any light on my problem. I happen to buy some raw goats milk and consume the whole half gallon in an evening. Normally drinking milk seems to intensify my gas problems but I noticed that I felt way better that night when I went to bed. Normally bed time is unbearable for me with gas, bloating, etc. Not only did I feel great that night but the effects lasted almost a week. I decided to get some more and see if it continued to help. Sure enough, after my symptoms started to return, I drank more and it has continued to lessen my symptoms for more than a week now. The obvious answer would be the probiotics in the raw goat milk but I really feel like something else might be going on. I consume a variety of probiotics in fairly large quantities otherwise but nothing has helped or been as lasting as this. Any ideas on why? Any similar experiences?
Michelle,
Wow and thanks for sharing this! I think you’re exactly right. Raw milk has lots of lactose-degrading probiotic bacteria present that also produce lots of lactase enzyme which is released when the cells die. This benefit is lost in pasteurized milk products. I hadn’t been recommending raw milk due to food safety concerns over pathogenic bacteria such as Listeria, etc., but recent data suggests that raw milk is much safer than originally thought. I will address this in the next edition.
Hi Norm,
I am about trying some herbs as support. Do you think that Allicin has less fructan/carbohydrate content than garlic?
Regards
Chris
Hi Chris,
Allicin is an organosulfur compound which means it contains no carbohydrates including fructans. Shouldn’t be a problem. Just keep in mind as a supplement the naturally occurring compound is chemically modified to make it more stable (not sure how this is done) and present in a much more concentrated dose than in fresh garlic.
https://www.jigsawhealth.com/faqs/allimax-supplement-facts
https://lpi.oregonstate.edu/infocenter/phytochemicals/garlic/
Hi, this book of yours sounds pretty cool. However I’m a vegetarian and sometimes it seems like most things I need to survive are on the forbidden list. I’m 6’6″ and I don’t think I can be happy on a diet of eggs and sushi rice, or whatever…I think you know what I mean…. As a vegetarian I need a lot of carbs. Or so it seems. I mean my symptoms – mostly wind and slight discomfort – annoy me, but I don’t know if they warrant a complete rethink of my diet, depending on what that entails, which might make me more miserable than the symptoms themselves. But having said that, I’ve noticed that cutting down on sugar and fruit and milk and bread seems to help. So I’m a bit of a waverer I suppose…. Does your book cater for hungry vegetarians like me? Thanks, Jim
Hi Jim,
Hungry vegetarians are one of my biggest challenges. If your problem is “wind and slight discomfort”, perhaps you need not make significant dietary changes, but some vegetarians I have worked with have dramatic and painful symptoms where dietary changes are absolutely required.
I have been partnering with a nutritionist and seeking input from more vegans to come up with more ways to crack this nut. The biggest challenge seems to be (I have never been a vegetarian, so I am in the learning mode here) that legumes represent the major source of proteins for most, if not all vegetarians. Legumes however, contain not only protein but also lots of fermentable fiber (verbascose, rafinose and stackyose) and a good bit of resistant starch as well. Perhaps some people can limit other fermentable carbs such as fructose and lactose and consume some level of legumes without too many symptoms, but likely modification of these legumes is needed to reduce the amount of these fibers and starches for vegetarians with the worst symptoms. One way is soaking as a recent paper reported a significant reduction in these fibers after soaking beans Another approach that is likely even more powerful is fermenting where these fibers and starches are actually consumed by bacteria during the incubation period.
Your input and ideas are welcome. What are some other proteins sources available for vegetarians?
Hi Norm,
I’ve had bloating and other gut issues on and off for a couple of years now after a few courses of antibiotics to get rid of a parasite. I’ve lost some weight too. I’ve had heaps of tests done with nothing sinister showing up. High yeast/fungus keeps coming up in stool tests but the GP doesn’t seem to think this is an issue.
Bloating is the main problem which is almost constant, and worsens after certain foods like apples and pears. I had some Kombucha recently and the bloating was so bad I got heart palpitations for two days. Stools went gassy, pale a greasy few days after too.
A couple of people have suggested this sounds like SIBO. Would you agree? I’ve tried cutting out sugar and carbs which is kind of helping but I keep caving in to the cravings.
Do you think your book would help someone like me?
Thanks in advance!
Jason
Hi Jason,
I can’t comment on your situation here, but bloating in response to sweet beverages and high fructose fruits is indicative of malabsorption and overgrowth of gas producing gut bacteria. The book is devoted to this problem.
Norm,
Short question if you don’t mind:
Does propylene glycol belong to the sugar alcohols?
Thanks again!
Hi Mark,
No propylene glycol is not a sugar alcohol.
Norm,
I just stumbled onto this site. I ‘m taking the SIBO test tomorrow (at home version) on the recommendation of my Holistic doc. I’ve had severe bloating, stuffy head, and not able to even tolerate much water. Makes me dead tired with sinus like symptoms. I’m 12 years post op from Nissen Fundo wrap. Saw a dietician recently and I reviewed a recommended Fodmap diet that my GI didn’t explain well. I’ve had tons of tests, ab scan, CT ab scan with dye, etc. All negative. Also a PH probe test, and motility test. Negative.
Tonight I had grilled salmon and short grain brown rice (as recommended) and I feel completely bloated and horrible.
I just stumbled on this site. Are you the author of some book for sale on here, and are you a real doctor?
Thanks,
Brian
Forgot to add, that my serious digestion problems started last November. I had an adverse reaction to SynviscOne (Hylan HF-20) and I was on everything under the sun. Pain meds, anti inflammatory, predisnon, cortisone shots………………..The only few periods I felt better is when I was on anti biotics………….
Hi Brain and welcome to the site. Yes, I have written a some books for sale on this site. Here is a link to the book page: https://digestivehealthinstitute.org/buy-books/
Here is a link to my bio:
https://digestivehealthinstitute.org/about/
Here is a disclaimer from the consultation page: Norman Robillard holds a Ph.D. in microbiology and has authored several books on digestive health, but is not a medical doctor. His advice is focused on balancing gut microflora through diet and behavior modification. This is not nutritional counseling. This advice should be used in conjunction with discussions with your own doctor.
Here is a link that describes how my diet approach differs from the FODMAP and other approaches: https://digestivehealthinstitute.org/2012/08/17/sibo-diet-and-digestive-health/
I was diagnosed with SIBO one year ago, I did the SCD diet for 6 months ,in this time I had my Knee replaced and knew I was not going to be able to eat the hospital food took my own, i am looking forward to my new book on SIBO and the calculator which I used already, now I am still having symptoms so this book is really going to help. Now the question I am asking is Has anyone experienced, with SIBO, a smell either coming from your body and always present, now I think it is a gas from my SIBO , two things make me think this, when I have more sugar or starch the smell is magnified,and everything smells like, this a pungent sweet smell , I also have leaky gut which has created a lot of food sensitivities so my food list is very short, and sometimes I eat something not,knowing if it will affect me. Other symptoms from SIBO are brain fog, arthritis, and overall tiredness, I am anxious to see if anyone has this smell . thanks for reading
Hi Norm,
What are your thoughts on coconut water kefir?
I had SIBO but have managed to wipe it out (i believe) when I had a surgery in May this year that required a bowel prep.
Problem was that I then developed at least once weekly diarrhea – that I tried to control with probiotics. Sacrcharomyces finally stopped the ‘D’ but then developed constipation…ugh. So someone suggested kefir. Since I never liked milk – I came across Tonix coconut water kefir at Whole Foods. I took 2 tbsp as suggested – only for 3 days – and I developed terrible burning and pain in my stomach so I stopped taking it. I read such good things about kefir – and that you should start slow. So after things settled down – the following week I tried 1/2 tbsp again only for 2 days – and at first I had perfect bm – but SOON after came the diarrhea again – with extreme fatigue. So again I read that it was ‘die off’ and should keep at it. Following week – went to 1/8 tsp – again for only 2 days – as the D came back again but this time even more fierce.
Meantime I noticed that I lost about 10 pounds! I read that bacteria can develop into water weight or something like that. I also noticed I did have less pain in my back plus good skin.
But when I attempted 1 last try – the diarrhea quickly came back, plus I just haven’t been feeling well. I am now a bit worried and hope that I didnt make matters worse.
I also notice alot of discomfort at night – in my lower abdomen like some fighting is going on :) or maybe cleansing wave?
In any case – can you get ill from coconut water kefir?
Thanks for taking the time to answer so many questions. I did buy your book – and have been following your diet – which also definately helped with the SIBO.
Hello Norm,
i have colitis ulcerosa and I just got a flare up after staying well for months because of coconut milk. Last week on Monday I started with coconut oil as a new part of my diet. I also ate more Brokoli and salad everyday. I noticed that it was not digested very well because I always saw small amounts of indigested parts in my stool. Thursday I noticed bloody stool and friday I ate coconut milk and that was the trigger for very bad symptoms. I also fall into depression when my gut is irritated. Not because I cannot deal with it but it seems to be linked. I cannot do anything other against this than getting my gut relaxed.
So now I try to calm my gut and feel well again. I am trying a ketogenic diet since 12 days (because of that I ate more broccoli and salad which I think also was a little trigger, but the big trigger sure was coconut milk).
I try this diet because have problems with mood fluctuations and know many people who solved this problem with this diet. I noticed that this diet can be combined with your concept.
So I now try to find some very easy to digest vegetables. Can u give me some help with that? Can I look at the fodmap list for these ones? Because: I do not eat any starch and now I can also avoid sugar alcohols…
What do you think of stevia? Can I use this for my diet?
And please tell me some good vegetables which I can eat to let my gut heal!
I really need help. I was at so many doctors now and they can´t help me. They just make me really angry because they talking with me, like I have only psychological problems. But thats not the case. When I am feeling well, my life is great. But with my colitis flaring up (also if it is just a little) I always get depressive. This is linked together and for me I found out that 95% of the trigger are foods. Maybe 5% is when I get really angry with somebody but this is really really seldom because I have nice and authentic relationships.
But because of my depression and gut symptoms, I loose connection more and more…I cannot eat with my friends and when I m depressive I don´t want anybody surrounding me seeing me like this….
Kind regards and thanks for your help!
Hey Norm, you have a pretty interesting article. You pretty much helped me to get information to finish my homework. Thank you!
Hi Norm,
I just finished reading your SIBO/IBS book. Terrific! Thank you for writing it.
I have three questions:
1) Do you recommend your low FP diet for people with systemic infections, such as Lyme, in addition to SIBO? I am concerned about the potential for raising blood sugar and feeding infections in the blood.
2) if you only consume low FP carbs, does that reduce immune system activity given that the immune system is stimulated by carbs feeding bacteria in the gut?
3) What modifications would you recommend for someone with SIBO, Lyme, dysbiosis and other infections both in the gut and the rest of the body?
Thank you so much in advance.
Hello Norm,
I purchased your IBS book over the weekend and read it that night.The book is so informative and makes so much sense.
I have been having issues for past five months and with its progression,I fully believe I have sibo.My GI doesn’t go along with this ,as I “am to young”.I am 28.I know I need to find a new doctor but I can’t get in for months.My current doc agreed to try xifaxan, said to treat ibs and if I do have overfrowth she said it would come back anyway ( again very discouraging to hear after months) My symptoms started after a very stressful family event and than seemed to snow ball.Started with little nausea,than stomach upset,had some loose stool,loud stomach rumbling,developed lpr,added gerd like symptoms,constipation and abdominal discomfort.My throat is raw and sore from lpr,I can have what seems like lpr without food. There is much more but I feel bad complaining,but I feel like I’m going at this alone and not sure of a few things.
Read to eat normal during antibiotic? I am doing this while implementing some of the book past couple days.
Read about L Glutamine? Now or after antibiotic and when do I take?
Iberogast? Now or after
With all the mixed literature on probiotics,I’m not taking any now.With me being constipated dominant good choice?
If I do have methane dominant sibo will this diet cure it? I read if c dominant that usually means methane?
I’m overwhelmed after reading and feel uncertain how much to eat.What can I do so constipation doesn’t worsen?What should I eat every meal to help
I apologize for the long post and I understand your very busy but if you have any thoughts on how to tackle this I would be so thankful.
Thank you for your time
Ashley
I apologize for this but wanted to add along with other symptoms I have had coated tongue for few months.Been cultured and nothing ever found.
Also weight loss and possible not gaining as easy as once did. When I was healthy I was one who could look at food and gain weight.We just went on vaca to Hawaii for two weeks and was eating most things BC I felt some symptom relief from augmentin was on for sinusbinfection. I gained three pounds and I think it was just water.
Thank you for listening
Ashley
Hi Norm,
I am in a study about FMT and its effectivity in IBS. From the top of my head I remember you once wrote an article here that eating FTD after FMT might be a good idea. I just don’t find this article anymore. Do you have a link?
Thanks and all the best!
Hi Mark,
This is exciting news. Please keep us posted on your progress! I have posted articles and links on FMT for Crohn’s but don’t recall an article discussing FMT for IBS. The topic has come up in some comments on the blog though. Here is one example in the article on Antibiotics for IBS:
https://digestivehealthinstitute.org/2012/09/18/antibiotics-for-my-ibs/
sydneygal says:
March 1, 2013 at 3:50 am (Edit)
You only talk about one side of the equation. There is therapy that replaces the good bacteria after the you’ve killed the bad & the good with antibotics. It’s called fecal microbiota transplant therapy (FMT).
Reply
Norm Robillard says:
March 1, 2013 at 4:59 am (Edit)
Hi,
Good point about FMT. The article is focused on antibiotics alone because they are increasingly being employed (without FMT) off label for IBS treatment. Also FDA approval is being sought for this treatment – without FMT.
FMT is a fascinating topic itself, but still in the experimental phase for C diff and there is even less experience using this approach with IBS. I agree, it may well emerge as an excellent therapy for IBS. For FMT, antibiotic pretreatment makes perfect sense. I do wonder if some people will relapse after FMT unless the issues that caused IBS in the first place are not addressed.
Reply
sydneygal says:
March 1, 2013 at 5:11 am (Edit)
Yes, that is frightening that antibiotics are prescribed without a gut flora replacement plan – that’s what got us into this mess in the first place! I am soon to have FMT for a myriad of gut issues, so I am only just starting the journey. If it doesn’t work, then I might have to resort to helminth therapy….now that’s equally fascinating!
Reply
Norm Robillard says:
March 1, 2013 at 12:58 pm (Edit)
Good luck and please report back on your experience. There is a growing interest in the states on FMT for IBS but few doctors offer it and the costs are quite high.
Reply
I do think the Fast Tract Diet would be supportive after one completes the procedure as too many of the wrong types of carbs could lead to an overgrowth of carb-loving, gas producing bacteria of the Firmicutes enterotype which will be present in the transplanted donor material.
Sure, I will keep you informed. Though I am the only one with IBS-C all others (15 people) are having IBS-D. Right now I am taking 800mg Rifaximin for three weeks and then I am getting two transplantations in two days. Once via coloscopy and the other one via enema the day after. I never experienced any effect from Rifaximin, I wonder if that is a negative sign and indicates that gut flora is not an issue.
So in terms of diet you suggest eating FTD? More in the lower or upper range like 30FP a day? I don’t want to starve the good bacteria of course but I also don’t want to feed the bad one. :)
Great Mark,
I assume you will also be receiving a PEG colon cleanse prior to the procedure. Is this the case? As for the diet following your procedure, first and foremost you should follow any recommendations in the protocol. But if are no recommendations, I would think keeping FP under 40 grams would be reasonable.
The fact that rifaxim didn’t help is only meaningful in my view, if no other means are employed to get rid of your current microbiota. That’s why I would be surprised if there is no colon cleanse before your procedure. .
Yes, I am getting a regular colon cleanse prior to a coloscopy. The thing is that PEG/Macrogol isn’t efficient enough to cleanse my colon anymore. The doc said I should combine it with sodium picosulphate then. Chances are that this will still be not enough to empty my colon. I then will do some enemas or taking Docusat – it’s all not very efficient unfortunately.
I am thinking about booking some hydro colon cleansing sessions before. Do you think that might be helpful?
During the transplantation process they want me to take loperamide so that I hold the transplants as long as possible.
They recommend to eat as usual so that any progress can be credited to the FMT and not to a new diet. The last months I was eating FTD (not strict). Right now while taking Rifaximin I do eat more carbs because I read that the antibiotic kills active bacteria. But FP below 40 sounds good to me and isn’t much different. I will definitely follow that.
Thanks!
Thanks for the details. The most important thing is to follow the protocol as closely as possible for the most meaningful study results. Introducing variables can make the findings difficult to interpret. Your study director can advise you more than I can on this, but if the study does not call for additional cleanses, I would not do it.
Good luck. I hope you have an epic response.
Hi Norm,
Your book is a blessing. Thank you! I was diagnosed with chronic idiopathic pancreatitis two years ago (I’m 44). Looking back, I suppose I’d had acute attacks as a child and as a teen, but not knowing any better I’d curled up in a fetal ball and tried to sleep it off. High triglycerides are a probable indication of pancreatitis and so an ultrasound endoscopy revealed an inflamed and marbled tail-end (the lipase or fatty end). After reading your book and Nora Gedgoudas’ Primal Body, Primal Mind I realized my problem was carbohydrates. Despite being advised not to eat any fat and to subsist on bland carbs by my primary and GI physicians, I eliminated all grains (I used to be a chronic rice eater) and began ingesting 5 tbs of coconut oil a day (after reading The Coconut Oil Miracle by Bruce Fife, ND), bone soups, root veggies, limited protein and organ meats once a week. The turnaround was remarkable. No more headaches (I’d suffered a permanent low-grade headache for two years), my triglycerides dropped from 260 to 76 in two months, my HDL rose and my borderline blood sugar issues were normalized. I had the energy level of a 25-year old. My pancreatic enzyme levels are normal and I still take pancreatic enzyme pills with every meal. My goal is to stop dependance on the pills. I still feel throbs in the tail end of my pancreas from time to time.
Only one issue persists: the bloating. I wake up with a flat stomach and even after a sip of warm water my belly begins to bloat. After meals the bloating is instantaneous. I began the low FP diet some months ago (so grateful for the carb), but the problem lingers. My naturopath thinks it may be SIBO and/or gut infestation and I’m awaiting my breath test/stool results from the lab. I’m wondering if you have any experience with treating chronic pancreatitis though the FP/FTD and if there is something else I could try or is missing in my diet plan. Thank you once again for your wonderful book.
Hi Sanjay,
Great job and thanks for sharing some very helpful ideas for pancreatitis. Continuing enzyme supplements make sense as no diet will reverse a deficiency. One thing you might consider for improving morning bloating is to give some thought to what you ate the day before. Perhaps some fermentation in the large intestine is persisting.
Norm you are very kind to reply to all these questions. I also forwarded this post to your email inbox, so my appologies for the double post. I am currently reading your book on my kindle. I suffer from SIBO, candida and possible leaky gut and am working with a holistic doctor to correct the underlying bacterial imbalances, including avoiding sugar and alchohol and adding in specific probiotic and herbal therapies. Until now tho I have consumed some high fiber, high FP foods such as yeast-free whole grain spelt bread and brown rice cakes (??) with some regularity so I am eager to try the suggestions in your book.
What is your take on the SIBO research linking it to moderate alcohol consumption? I would love to enjoy an unsweetened alcoholic beverage with my husband on occasion after I correct the SIBO and candida overgrowth!!!
https://www.sciencedaily.com/releases/2011/10/111031114949.htm
And this excellent article on gut health which I have excerpted and included the link. It seems like binge drinking is very bad (which I know you are not advocating!) but how to know a safe limit?? Thanks for reading!!
Alcohol’s effect on the mouth, throat, and esophagus
“Alcohol’s impact begins as soon as it enters the mouth. The mouth, like all parts of the digestive tract, is populated by bacteria. Many of these bacteria are deemed commensal, meaning that like beneficial gut flora, their presence helps keep this part of our bodies healthy, as well as aid in the digestion of food.
An oral cavity replete with healthy colonies of beneficial bacteria keeps potentially pathogenic organisms at bay by creating an environment that is less conducive to their growth (many times by regulating mucosal pH), and by outcompeting these potential trouble makers for attachment sites.
Now I’m sure most of you have had rubbing alcohol applied to your skin before receiving a vaccination. And the reason for this is to disinfect the site and prevent infection by whatever bacteria happens to be residing on your arm or butt prior to the needle prick.
Alcohol is a very effective bactericidal because it easily disrupts the lipid membrane that encases bacteria. Sadly, however, the alcohol you drink has no magical ability to differentiate between beneficial or harmful oral bacteria. It just goes about its business popping bacterial membranes without a care in the world.
While oral bacteria, like gut flora, is fairly resistant to bactericidals, much as gut flora is somewhat resistant to short courses of antibiotics, there are limits. Limits that are dose dependent, and therefore partly explain the horrific state of dental and oral health that afflict many who abuse alcohol.
Alcohol, apart from effects on oral bacteria, causes direct injury to the mucosal lining of the mouth, throat, and esophagus, inviting inflammation and bacteria that thrive in inflamed conditions. Chronic and acute alcohol intake damages the salivary glands and causes interference with saliva secretion. (5) As saliva contains lactoferrin, a glycoprotein that inhibits the growth of oral pathogens, the risk of oral dysbiosis rises with increasing alcohol intake. (6)”…….he goes on with more info!!
https://gutcritters.com/alcohol-and-the-gastrointestinal-tract-2/
Hi Bearsmom,
I’m glad you asked this great question. I saw the article and have sent for the paper in it’s entirety. Even before reading the whole paper, based on the info in the abstract and the Science Daily piece, I just don’t buy it. Here are three reasons why. First of all, it’s a small study and most of the people that were tested were moderate drinkers (as stated in the article: “An overwhelming majority (95 percent) of the 198 patients in the study drank a moderate amount of alcohol”). So the control group that didn’t drink is pretty small (5%). Secondly, the study is observational – simply asking what behaviors people with SIBO have in common. You could easily end up concluding that driving as opposed to taking the bus causes SIBO. These studies can’t prove something. They can only generate a hypothesis to test. The last and most important reason has to do with what an alcoholic drink is. It can be a shot of whiskey, or a glass of dry wine, but many people drink beer (resistant starch), sweeter wines (sugar) or mixed drinks (lots of sugar).
As a long term sufferer of acid reflux (also linked to IBS and SIBO), my body can tell the difference between light and non light beer and zero calorie mixed drinks or whiskey on the rocks and sweetened mixed drinks. These are the reason I focus on fermentation potential and don’t limit alcohol itself in the Fast Tract Diet. By the way, alcohol is absorbed rapidly into the blood stream starting in the mouth and stomach before it even reaches the intestines. One more reason to be skeptical about moderate drinking and SIBO.
Also while on the topic of acid reflux, check out my article on a GERD Diet that Works Without Drugs where I cite a much larger case control study involving 3153 people that concluded that alcohol “did not seem to be risk factor for acid reflux”.
Thanks for your prompt reply! I have to say I am excited to think that I may be able to enjoy a drink or two again some day! Do you find tho, that the conditions that allow for SIBO, also promote candida overgrowth? (i.e. Lack of acid-forming probiotic strains, slow gut motility, stress, poor diet, antibiotics, NSAIDS, history of birth control use, etc…). So would it be safe to assume that many with SIBO, also have candida albicans overgrowth? (Dr. Jeffrey McCombs has a GREAT video for anyone interested that suspects they also have candida overgrowth-called The Science of Candida-not trying to promote his plan! https://www.candidaplan.com/). With Candida risk in mind it seems one would want to avoid table sugar and excessive alchohol consumption (particularly of sugary alcoholic drinks) and yeast-fermented beverages!
Hi, Dr. Robillard. I communicated with you last year. I have been doing the low FP food choices for a year and it is definitely helping. I have a question as I’ve seen info lately about the “SCD” diet and how it is making a comeback, it was used pre-discovery of gluten issues, and apparently had a very good rate of success regarding people being able to ‘heal’ from celiac with the SCD. I am wondering about your views on the SCD plan.
Also, I am struggling with very low weight due to food intolerances, and I’ve started using Vivonex. Any thoughts on that product? It does have maltodextrin. I seem to tolerate it well, as I continue to find the best approach to actual food, I need the caloric supplement and the amino-acid protein base. The question of how to digest protein and fat is one that I struggle with – so the low FP is part of the bigger picture but these other issues tend to add up to needing nutritional supplements, which I’m generally averse to, but have to do.
Thanks for any thoughts on the above. Laura
Hi Laura,
I cover both the SCD and elemental diet (such as vivonex) in this article (https://digestivehealthinstitute.org/2012/08/17/sibo-diet-and-digestive-health/).
Short term Vivonex should be no problem. Maltodextrin digests as easily as glucose (FP = 0). Long term, the goal should be a real food diet to avoid nutritional deficiencies and maintain a health gut microbiota. The Fast Tract Diet, while low FP, does contain 30-45 grams/day of fermentable material that feeds a healthy gut microbiota.
Hi Dr. Robillard
Splenda alters gut microflora and increases intestinal p-glycoprotein and cytochrome p-450 in male rats.
https://www.ncbi.nlm.nih.gov/pubmed/18800291
This study about splenda really concerns me. Our microflora is still such a black box, I wonder why you are listing sweet desserts that include splenda so often in your book? People with SIBO, likely have candida albicans overgrowth and other microflora imbalances and generally low counts of beneficial bacteria. It seems that we should all be steering away from our sweet tooth and needing to add splenda to everything. Even whipped cream? I mean, whipped cream is so good without ANY sweetener!!! Also, small amounts of maple syrup or maple sugar or brown rice syrup, I feel safer about giving this to my kids or ingesting myself. My holistic doctor that has worked with complex SIBO patients for nearly 20 years says that she has seen adverse health effects and symptom relapse with use of stevia and splenda and other artificial sweeteners. Thanks so much for any thoughts
Hi Bearsmom,
Thanks for posting this question. I understand and respect that some people are concerned with the safety of Splenda, the fact that it’s not “natural” and / or the possibility that it could upset the microbiota. For this reason, I provide several alternatives to Splenda including stevia, glucose, erythritol (the one gut friendly sugar alcohol), maltose, rice or barley malt syrup or even small amounts of sucrose containing sweeteners. I personally think sucrose and sweeteners containing sucrose are by far the worst sweeteners in terms of gut health and general health.
With regards to the paper you cite, I’m a bit skeptical. First off, this study was funded by the sugar industry – who doesn’t like Splenda much. Also, there is a question about what the changes in micro numbers really mean (when you have 20 million bacteria, a drop to 50 to 80 percent of the control is still 10 million to 16 million bacteria – does it matter?). Also the weight-loss data follows no dose response, typically a giveaway for results that are not meaningful (weight gain was higher at a lower level, then decreased at a higher level, then increased again at an even higher level of Splenda). Lastly, the study was done with rats raising the question of relevance to people.
Personally, use small amounts of both Splenda and stevia, but this is a personal choice. I understand and respect your concern and decision to use an alternative.
Hi there Norm
I just came across your site today and have ordered your book. I have had tummy pains gas and bloating for nearly 2 years now and 2 months ago had a colonocopy and endoscopy to see what was wrong. They found mild gastritis. About 3 weeks after this all of a sudden the acid reflux started 24 hours a day. Acid is pouring into my mouth and my mouth and tongue feel all burnt and I have a constant white coating on my tongue and my throat feels like it is burning and closing up.. Could the procedures have given me an infection. I have been eating a paleo diet for 4 weeks now but it is no better and I am desperately near having to start PPI’s as I cant stand it anymore. As it will probably be close to a week before I get the book can I just confirm that the following foods are ok to eat before I get the book and can research a little more
Berries.
all meat
Coconut and olive oil
nuts
Femented regis
All vegis except root vegetables.
Broths
Avocados.
I am also seeing a gastro on thursday and wondering if there is anything in particular I should ask him or tests to run.
thank you so much and I look forward to getting your book
Hi Laura and welcome. The foods you list are fine. Gas and bloating are consistent with SIBO. You might consider lactulose breath testing. You might also get checked for H. pylori, if you haven’t already, given the finding of gastritis.
I am a little wary of coconut oil as the “perfect” oil touted in the Paleo community. With severe digestive issues I personally would start with olive oil, maybe even butter or tallow and then test the coconut. It is highly anti-microbial which is why it makes people feel better, but when one is really out of balance and has dysbiosis, I think coconut can be very strong. This is just advice from my holistic doctor that has seen it do damage if used regularly in some people.
Dr. Robillard thanks for your forum I just registered. And thanks for your thoughtful replies. I had been posting questions under my full name but just joined the forum and picked a new forum name. I am going to do a long post in the auto-immune section, as I myself suffer from Interstitial Cystitis (IC) a painful bladdder condition, which is now in the holistic medical community strongly associated with SIBO and leaky gut, even if it is not looked upon in the same way in the western medical community. It is estimated that 4-10 million people in the US have this condition. With the strong association to SIBO it is quite possible your diet could have quite an impact on the IC sufferers that look into your approach and could be an important tool for western doctors and holistic doctors alike. I have only tried your diet for a few days and so far still have a lot of bloating (my worst symptom, I rarely have heart burn). My SIBO is pretty severe and I was thinking I should try the 70% Fat diet that you recommended to some people for the first week to see if I can get my symptoms more under control. Do you have a sample or suggestion of where to look to calculate maximum protien intake and fat intake? What would the 70% fat meal look like? THank you I am really praying I can get some relief from this bloating, I have had it for 2 years.
Dr. Robillard
Sorry for all of the newbie questions! I was looking around in the forums and saw your response about the Soil Based Organisms, in particular, Prescript Assist as an augment for treating SIBO. I was hoping you would be tracking this!! My holistic doctor uses lactobacilli and bifidobacterum and L.bulcaricus at times but NOT SBOs. The more recent data suggests that maybe it is an option but my doc does not seem to be inclined to use this approach, maybe because the SBO’s even though we have evolved with them are less know. Here is a clip from an interview with Chris Kresser, a popular holistic health practitioner, blogger, etc.. saying that he has better success treating SIBO with SBOs than the acid forming probios. I welcome your thoughts!
https://chriskresser.com/treating-sibo-cold-thermogenisis-and-when-to-take-probiotics
“Probiotics are actually a mixed bag with SIBO because SIBO often involves an overgrowth of D-lactate-producing probiotic species, and that causes a buildup of D-lactate in the gut, and a lot of the symptoms associated with SIBO are caused by that. So, you want to avoid in many cases taking any probiotics that have D-lactate-forming species like Lactobacillus acidophilus, which is, of course, one of the most common probiotics that people take. There’s a D-lactate-free product sold by Custom Probiotics that’s helpful.
I’ve also found soil-based organisms to be helpful when SIBO is present, and the one that I like the most right now is called Prescript-Assist, and I just added it to my store if you go to ChrisKresser.com and you click on the store link in the upper right, I’m now selling it because I’ve actually had a lot of success with it myself and with my patients in my practice. I recently learned about it. A few months ago, I started doing some research about it. There’s one study that was double-blind, placebo-controlled that lasted for quite a long time, especially for probiotics. A lot of the studies are pretty short in duration. And essentially the theory behind it is that we evolved in an environment where we were continually exposed to these soil-based organisms. Our ancestors were not scrubbing their vegetables and fruits before they ate them. They were taking them out of the ground and maybe wiping them off a little bit and eating them. They weren’t buying them in the store after they had been scrubbed, and they weren’t scrubbing them themselves. And the other thing is that the soil diversity and quality has changed a lot since the industrialization of agriculture, and so we’re just not exposed to the same number and types of soil-based organisms to the same extent that we probably were for most of our evolutionary history. And as we’re going to discuss in a lot more detail in a later question, there’s a lot of evidence that these soil-based organisms have profound immunoregulatory effects. In other words, we evolved with them over a long period of time, and our immune systems have a symbiotic relationship with them and function much better in their presence. And so the soil-based organisms are a different approach than the lactic acid-forming types of probiotics, and I’ve found that they’re better tolerated in people with SIBO. As a fairly unrelated side note, they tend to work better for constipation than a lot of other probiotics. Oftentimes, probiotics can make constipation worse, so the soil-based organisms and Prescript-Assist, I think, is a really good choice for people with SIBO.
And then another probiotic that can be helpful with SIBO is Saccharomyces boulardii, which is a beneficial strain of yeast, and I’ve had some success with that as well.
So, there’s more to it, but that’s a really good place to start, all of those things that I just mentioned: Lauricidin, the biofilm disruption, some of the botanicals, soil-based organisms, and Saccharomyces boulardii.”
I want to do a probiotics article one of these days, but there is so little positive data published that it’s not an exciting task presently. Some good results for diarrhea, less than stellar results for most other gut conditions including GERD and IBS. The SBOs formulation Prescript Assist has some positive IBS data published and some people report encouraging results. That’s why we added a link for the product. But the most troubling symptoms of IBS/SIBO were not addressed in the studies leaving a bit of a question mark.
I really think probiotics will be great one day, but first we need to identify, produce, preserve and deliver the most critical strains. This is no easy task as many of the strains that appear to be critical to good gut health are very sensitive to oxygen and many gut strains have never even been grown. FMT in a pill might solve some of these problems – but (anaerobically) collecting, preserving and delivering will still be a challenge.
Chris’s talk about D-lactate was interesting. This issue has been best studied in people with short gut syndrome. The inability do degrade D-lactate (something most humans can apparently break down. https://www.ncbi.nlm.nih.gov/pubmed/9556700) may also be a prerequisite.
Carbohydrate malabsorption, entereal (tube) feeding of too many carbs and lack of motility (such as short gut) is typically involved. In one published case, the solution was bicarb to address the blood acidity and limiting the carbs in the enteral feeding. https://www.ncbi.nlm.nih.gov/pubmed/15927940. In an other case antibiotics were added. https://www.ncbi.nlm.nih.gov/pubmed/18242965. In one case, Lactobacillus fermentum was isolated.
I am unaware of reports on someone without short bowel syndrome having D-lactic acidosis, or of someone suffering from this after taking Lactobacillus acidophilus – but you never know. At least the symptoms are pretty obvious to spot – people affected appear drunk.
Some more background info: https://www.amc.edu/academic/gme/programs/Gastroenterology/documents/wang_crohns.pdf
“In individuals with intact small intestine, few carbohydrates and starch reach the colon. Delivery of glucose is markedly magnified when the small bowel is removed, bypassed or diseased.
In patients with short bowel syndrome, glucose reaches the colon, and when in combination with bacterial overgrowth (usually gram-positive anaerobes, eg. Lactobacilli)– D-lactic acid is formed.
Episodic metabolic acidosis can occur after meals with neurological symptoms including altered mental status, confusion, dysarthria, cerebellar ataxia, and concentration/memory difficulties.
D-lactic acidosis should be considered in short bowel patients with an anion gap metabolic acidosis, a normal serum lactate; characteristic neurological findings and acidosis following food intake.
Diagnosis is confirmed with special enzymatic assay measuring serum D-lactate.
Treatment involves sodium bicarbonate, low carbohydrate diet and antibiotics (usually Vancomycin, Neomycin or Metronidazole) to decrease bacteria overgrowth.
D-lactic acidosis should be considered in all patients with short bowel and/or other malabsorption syndrome whose acidosis corresponds with food intake and resolves after cessation of ingestion.”
Thanks Norm, that is very interesting. I wonder what specific symptoms have occured that he has observed. My holistic doctor uses microdoses of Natren megadophilus initially because otherwise it is too strong for most of her patients. Eventually tho it seems to be beneficial, and bifido as well? In my experience, bifido has direct action on gut motility (although I can’t recall the study that proports this). It might be worth mentioning in the constipation thread as it has helped me. Also, digesta-lac, by Natren. She uses always single strains so she can track what is going on. For some reason, her IC patients generally respond really well to small amounts of lactobacillus
Dr. Robillard can you comment on this notice from the Environmental Working Group?
Thanks!
https://www.ewg.org/foodscores/content/arsenic-contamination-in-rice
I did find this post by Kresser that says that white rice has much lower levels, and for adults, organic white rice (at a few servings per week) has a relatively low risk, but brown rice is NOT a health food these days.
https://chriskresser.com/arsenic-in-rice-how-concerned-should-you-be
Interesting article. I don’t have much to add. Something else to keep an eye on. Heavy metals are a concern. For instance, lead has been found in calcium supplements which is not surprising since lead and calcium often are present together in the environment.
Luckily, the Fast Tract Diet limits rice serving sizes well below what many people normally consume. And the recipes involve a rinse step.
My daughter (15 years old)has celiac disease and after being gluten free for 4 years started experiencing all SIBO symptoms. After trying all different foods we came to conclusion that a diet close to your Fast Track Diet works best for her. So when I found this website I was happy to see that we are on the right track. She can eat buckwheat, oatmeal, and potatoes without any symptoms. But rice, especially brown rice, any gluten free flour make her sick. So we avoid all pastas, bread, pizza, anything baked, rice. I will try Jasmin rice and see if it is better for her.
But she is a kid. She needs to socialize with her friends and go away to college at some point. So my question is: for how long should she be on this diet to cure? Is it life long diet or she will be able to eat some grains after a while?
Thank you.
Hi Marina
You might want to look into the link between celiac and SIBO. It is interesting. From what I understand from reading this forum, once the microbial load is reduced, digestion is improved, she should be able to have a few more of those foods in moderation. If it were my daughter (and I have two, one with digestive issues), I would encourage her to keep most of these healthy choices for life. Not that she can’t have pizza or icecream sometimes. But eating poorly, is how my holistic doctor puts it: “Living out of balance with nature” and for a lot of people there is a price to pay with your health. I wish I could tell my kids, “Sure, go eat the standard American Diet with abandon and dont pay any attention to the signals your body is giving you–don’t worry about it.” But instead, I am trying to raise my girls to make really good food choices, avoiding processed sugar (and for my younger one, steering her towards the healthy choices offered in the Fast Track Approach, because she has mild GERD at age 7. ) They have learned to read food labels and ask questions. They still have treats when they are out, but we mostly eat healthy fruit for dessert at home and don’t use sugar in our baking, but healthier alternatives. If your daughter learns this diet well, she will FEEL BETTER, and be empowered to make better choices, and this will reduce her stress in social situations. My guess is she will have setbacks, and then learn for herself and she will be fine. One of the things that I wish someone had taught me, is what a good bowel movement is. I wish I had known that having gas all the time and being irritable before eating is NOT normal. It is common, but not normal. I wish someone had told me that having painful periods and needing to take NSAIDS is NOT normal. I hope your daughter can learn to recognize the signs of impaired digestion so that she can get herself back on track. Knowledge is power. I wish your daughter a happy, healthy life and I hope this diet will help her. Don’t stop asking questions!!
Dr. Robillard,
I have SIBO and have lost 30 pounds in a few months. I am 5’5 and 89 pounds. I am unable to gain any weight, have only lost weight. I cannot swallow solids and have gas in my esophagus up to the throat 24 hours a day. This makes it hard to eat, but I ignore it just to get calories down me. I eat 2,000 calories a day in a Vita-Mix. I eat grass fed hamburger, and 4 jumbo eggs a day, in addition to jasmine rice, and quinoa and brown rice pasta, baby food green beans and carrots, and butter and whipping cream just to keep some weight on. This is a huge amount of protein and saturated fat for someone my size, but I don’t have a choice due to weight issue.
I don’t have a doctor that treats this condition in my area. I live in Central California. I did manage to get my Dr. to prescribe a pediatric dose of Rifaximin. He didn’t want to, but I had tested positive for SIBO. I could only take a 1/4 of the dose 75 -150mg. and have been taking that for 2 months. Only a low pulse dose due to diarrhea side effect (increasing weight loss). However, it does not seem to be effective at keeping the symptoms at bay anymore and things have been getting worse. The smallest, imperceptible amounts of anything, including vitamins, herbs, etc. bring on a huge reaction. I also have heavy metals I am dealing with.
Is there anything you can suggest to save me?
Cynthia, jumping in ahead of Norm here, it sounds like you need to get the book (I got it on my kindle) Fast Track Digestion:IBS and read it ASAP. This diet can be a much better appraoch than antibiotics for control of SIBO. Many (MANY) of the foods you listed would NOT be recommended for SIBO control, but there will still be many of the foods you listed that will be allowed. Also, come over to the Forum available at this site for more support!
bearsmom, thank you so much for your response. I am only able to certain foods without a reaction, and although some of these foods are bad, I have to try to keep the weight on. I have just lost another pound and the doctors don’t know what to do. I upped my dose of antibiotic and my symptoms are a little better today, but the weight loss really concerns me. I will definitely get the book. Also, I would love to join the forum. Do I just click on forum? This is new to me and I’m not very computer savvy.
Hi Cynthia, I see you are very concerned about weight loss. I dropped 55 lbs while trying to figure out how to gain further nutrition – it certainly can be scary. While I don’t advocate this for everyone and certainly you *should* be monitored by an MD and a nutritionist, etc. – the Vivonex TEN elemental nutrition is protein in the form of amino acids (already-broken down proteins) and vitamins etc. – it is a ‘total’ nutrition in the form of 300 calories per packet and 11 or so grams of protein in a packet. People DO take upwards of 3 or 4 packets a day when it is necessary, but ONLY with medical supervision. It is very important to be supervised on this, because you can throw your body into electrolyte and other imbalances if you are “refeeding” too quickly etc. – so please DO NOT take my words as any form of medical advice. I’d only suggest that an “elemental” liquid nutrition easily absorbed at the top of the small intestine may help you with the weight loss. I’ve gained 3 lbs and I”m thrilled, and I”ll continue iwth the Vivonex along with actual food, until I can gain back enough weight so that I’m not in the ‘scary zone.’ BTW Dr. Robillard does include elemental nutrition in his book, but I don’t want to suggest that he’d agree or disagree with my comments. So, everybody is off the hook!! However, it took me quite some time to FIND elemental nutrition, to find which one would work, and to then get monitored. Starting the process of inquiring might perhaps help you to be less scared of the zone of weight loss… there are steps you can take, of course including the low FP that Dr. Robillard advocates. I’ve been following Dr. Robillard’s food plan, and it has helped enormously, as well. Good luck. Laura
Hi Norm!
I wanted to follow up on my progress with the Fast Track Diet and ask a couple of questions! For SIBO-related health conditions, your website and book are hands down the most accessible, practical and helpful of anything I have read in 2 years of constant research. You are gracious to acknowledge the work of Siebecker and others regarding SIBO, but I think your work may ultimately have the greatest Public Health impact, and I am gratefull for it!
I would love to do a consult with you, and I may in the future. However, two years of a rediculous amount of unreimbursable medical expenses (Western doctors are useless for treating my health condition) are making it difficult to afford a consult, but maybe next year if I don’t get all the improvments I want :) trying to troubleshoot on my own.
My main digestive symtoms are burping, constipation, and bloating (lucky me, I have the constipation version of IBS!). For anyone reading that has bladder symptoms, I have SIBO-related Interstitial Cystitis (IC, a painfull bladder condition) and IBS-c (both are closely related). Briefly: I lived with mild SIBO for most of my adult life. It wasn’t until my peridontist insisted I take 2 rounds of broad spectrum antibiotics within one year as a PROPHYLACTIC for dental implant work, that the “dam broke” as my holistic doctor put it: SIBO and candida thrived, which led to leaky gut and IC.
When I started your diet I immediately had a reduction in gas and bloating by about 80%! It really helped me connect the dots of years of symptoms of malabsorbed carbohydrates! I was so encouraged so I have continued with the Fast Track Diet. After nearly 4 weeks on the diet, trying to manage my slow bowels with magnesium, I am still having gurgling after lunch and dinner (probably in part from the darn magnesium but I need to keep it in for now), minor gas, a little burping after each meal, and sometimes minor bloating after dinner. I am trying to address underlying motility and (possibly?) stomach acid, etc.. working with my holistic doctor.
To further reduce the FP and get the best baseline, for the past week I took out the low FP fruit, nuts, and recently, jasmine rice. I only consume 1/2 cup of full fat greek yogurt (listed in the first two week diet plan) and a bit of cream in my coffee and maybe one slice of cheese as my dairy. Otherwise having modest protien, lots of fats and low FP veggies. The thing is, since removing the rice and fruit, I am really afraid of ketosis. After several days of no jasmine rice or low FP fruit, I can already see my sleep is suffering. It is more disrupted and my energy is poor and having mild headaches (the carb flu I expected from a low carb version of your diet). I have seen you address the ketosis concern on this thread. But I am confused about your response and was hoping you could clarify for me.
For one reader that was worried about ketosis, your wrote the following: “You can consume plenty of carbs if desired. In the recipes, we kept the overall carb counts to less than 100 grams per day. You can consume more as long as the FP levels are maintained. For instance, jasmine rice has an FP of zero so there is technically no limit to serving size. We recommend limiting servings size to 1/2 cup initially – for the first week or so. We do that in case people have advanced SIBO where bacteria are present in the earliest part of the small intestine. In those cases, even the simplest / most easy to digest and absorb carbs might feed these bacteria. By limiting both FP and the total amount of carbs early on, your control systems (stomach acid, motility, immunity, etc.) can clear out the bacteria.”
Norm I have been very carefull about my rice consumption for two-three weeks, keeping it to only 1/2 cup per day, but still have minor symptoms which makes me worry the SIBO is still active. My questions are:
Should I continue consuming rice in the small quantities you suggest and expect continued gradual improvement (so I can stay out of ketosis)?
Or
After nearly a month on the diet, do I need to assume the FP for rice and fruit is higher for me because of my advanced SIBO and keep them out for a while? If so, this means I will have to go into ketosis. How long would you recommend I do this before re-introducing the rice? (can you tell, I do not want to be in ketosis? LOL)
THANKS for everything Norm!!!
Hi Bearsmom,
You wrote: “After nearly a month on the diet, do I need to assume the FP for rice and fruit is higher for me because of my advanced SIBO and keep them out for a while?”
I think that is the correct interpretation. Following all of the troubleshooting tips in the book for food prep and behaviors to ensure optimal digestion and absorption is important. Cutting overall carbs is one of those strategies that you may need to use. I personally adopt quite easily to ketosis as do many of my friends including experts in the field, but of course not everyone is the same. But I would not be put off too much by temporary ketoadaptation symptoms – feeling tired, etc. Your body needs to make a significant metabolic shift to fat burning. Many enzymes are down regulated while others are up regulated. Give it a week and you should be fine. If not, then a consultation might be a next step.
Hi Laura, thank you for the information, unfortunately, I am so sensitive to minerals, vitamins, etc. that I have a major response, sometimes 2-3 of not sleeping, or shut down of digestion (vagus nerve). So, I have to start out with a supplement the size of a grain of salt. I am going to try adding a grain of Berberine to help kill the SIBO. I was able to get my MD to prescribe me some Rifaximin, but I am not under his care since he doesn’t know what SIBO is. I Skype with Melanie Keller at the SIBO center and she is helping me with the dosage of 75-150mg. of Rifaxmin, but I don’t like to take antibiotics and I have been taking this low dose for almost 3 months. Hope I can incorporate some herbs and just get rid of this for good. Life used to be so good.
Hi Laura,
By the way, how much do you weigh now and how tall are you, if you don’t mind my asking?
Hi, Cynthia. Sorry for the delayed reply, I just saw your question! I’m 5′ 2″ approx and I was down to 93 lbs. I had been a ‘chunky’ (for my height) 145 lbs. My ‘good weight’ is about 110 lbs. I am now back up to about 98 lbs. with the Vivonex. I tried Rifaxamin and didn’t tolerate it at all. I also tried 2x rounds of Doxycycline, which seemed to offer relief short-term (a month) the first time, and nothing the second time. So far, it’s been dietary changes, the Vivonex, and also L-Glutamine, 10,000 g a day (approx 2 heaping teaspoons) diluted in room-temp water. Vivonex Ten has less fat content (and tastes much better) than Vivonex Plus (more fat content), for anybody who has fat digestion issues. I can tolerate 2 – 3 packets of this a day, which adds 600 to 900 calories, and about 36 g (amino acid/ protein) a day , plus a full MDV basic vitamin profile. This is enormously helpful for problems with weight loss. L-Glutamine is documented medically (you can look up articles on PubMed) to help with tissue healing and is used post-surgically, among other types of uses, to help with intestinal repair. It is tasteless and I have no negative reaction to it at all, I can tell it is also helping with gut healing.
I wonder if anyone has used pro–kinetics if you have IBS-C related to SIBO / IBS? I’d like to find one that is easy to tolerate and try it.
I AM taking domperidone (a compounded drug, by prescription, and PS not covered by insurance companies), as an alternative to Reglan, and I find Domperidone very easy to tolerate and a life-saver with regard to motility issues that arise with IBS-C and SIBO.
Each person has his or her own particular ‘cocktail’ of the preferred everyday treatments…. and I know we all ‘tweak’ this constantly, since there’s no absolute regimen that works for each (biologically customized!) body!
I also use a terrific set of relaxation tapes daily. This helps with pain control.
I offer these ideas not as any type of ‘prescription,’ and I am not a medical professional. Please note that I deeply believe each person should be thoughtful about his or her own ‘messages’ from the body, and that it’s so very important to share what works with one another, and to hear Dr. Robillard’s wonderful, sage advice and clinical experience. I also follow the Fast Tract as best I can, with a few IBS modifications etc. It works very well and is quite helpful. I can gain significant nutrition following the plan, with fewer symptoms than a year ago.
Onward and upward to us all, and thank you, Dr. Robillard, for your commitment to helping heal individuals with SIBO, and other digestive issues. Thank you, too, for providing this wonderful forum for sharing.
Clinical research often starts with amassing anecdotal experience and then looking at ‘what worked’ and deriving information for design of new research studies. The more we share, the more information researchers have to go by, and we are all in this together, in a continuum of helping one another.
Sincerely, Laura
Hi – oops – correction to the above! I take L-Glutamine, 10 g a day, not 10,000 (wrong!!). Sorry! Laura
Hi bearsmom, I too suffer from the bladder problem and constipation, but sometimes diarrhea, probably from the antibiotics. The more constipated the worse the bladder symptoms. Magnesium and some fiber in the diet really help, as does walking about 100 steps after each meal (for me). I also wanted to let you know that when I first started having digestive problems in June, I was unable to eat more than 400-600 calories a day which essentially starved the SIBO, since I was only eating protein. I couldn’t eat anything else. After 3 months of this, you would think the SIBO would be gone, but in August, I started being able to eat a lot of food, including pasta, and vegetables with no problem and started gaining some weight, then 1 month later everything changed and the symptoms started up again and I started losing weight. I think is is very necessary to keep taking some sort of microbial herb and rotate it with others, until your motility is stable and the intestine is healed and strong, but thats just my opinion from my own experience. Hope we can all beat this soon.
Hi Cynthia! Thanks for the info! Maybe we should contact eachother through the institute so we can compare notes and talk off line? My first thought is why were you eating pasta? I thought that was for the most part, a no-no on the Fast Track Diet? Do you think that is how you got the SIBO again? ABX and herbal ABX will not fix SIBO because the underlying issues have not been addressed. I treat with a holistic doctor that really only treats IC and digestive issues. She is not a proponent of ABX. Could you consider trying the diet alone and not the abx? The ABX can create a lot of other imbalances in the body, even if they tell you it only targets microbes in the small intestine. It may create resistant strains, as Dr. Robillard has alluded to and may not kill all the bad bacteria. And the relapse rate for ABX is so high? I really don’t understand how doctors can prescribe them! If we talk off line I might be able to help you with a targeted holistic approach that would compliment Norm’s diet. My doctor also knows precicesly which probiotics are safe for IC, and how to dose them properly to avoid pain. The underlying issues that lead to bladder symptoms include leaky gut, severely compromised mucosal tissue throughout the body, weakend organ systems and immunity. My doctor can help with a lot of this in a holistic way. Contact Rhea she has my email. She could get us in touch! Also come post at the IC section of the forum here. We can support eachother!
Hi Bearsmom, I actually cleared eating the pasta with Dr. Keller she is a SIBO expert, she said to try it because I was desperate to maintain my weight. However, Dr. Keller and I have never met since she is in Oregon and it is very expensive to speak with her each time. I am one of her most difficult cases. She is not sure what to do with me, given my sensitivities. After reading the posts here I am trying to determine what is the most offending food I am eating to cause the 24-hr gas up to the throat making it hard to swallow. I eat the same thing every day, so it could be the two jars of baby food green beans or peas, or the two jars of baby food squash, or the 1/4 of whipping cream or the 2 ounces of brown rice and quinoa pasta. I would have to replace the pasta with more jasmine rice, I already eat a cup of it a day and I am going to try to reduce or eliminate the pasta and substitute it with another cup of jasmine rice bringing me to two cups of rice a day. There is just no way around it, I need to take in 2000 calories a day. I might try substituting butter for whipping cream. The baby food makes up about 8 grams of fiber per day, and for now I will keep using it. Why baby food? Because it is already pureed and easy to add to my blended food. The grass fed hamburger meat and 4 jumbo eggs I will also keep, I know these are fine. As for the antibiotics, I hate taking any, that is why I am on a low pulse dose, just to keep the SIBO under some control and my weight on. My doctor says with my current calorie intake I should weight over 100 pounds, but SIBO apparently damages the intestine and can affect absorption of calories and nutrients. I am in a tenuous situation since this leaves me malnourished. I am much more comfortable taking the herbal remedies, an infants dose to start, one herb at a time. I am not like most people and need to experiment.
I understand exactly what you mean by underlying cause and for me one of the reasons was not taking enough thyroid medication which really slowed my gut. I had radioactive iodine for Graves disease 14 years ago and now need to take thyroid meds. I already knew my colon had a lot of pathogenic bacteria and that bacteria can travel up into the small intestine when there is a motility problem. Plus, my stomach was taking a long time to empty. I have also had IBS for years.
I would love to speak with you off line. Let me know your thoughts on the food I am eating. Which ones do you think are the worst offenders?. Also, have you tried colostrum which is supposed to seal leaky gut? The Doctor said some people do well with it and some don’t depending on their reaction to milk. What do you think was the underlying cause for you getting SIBO?
This is very debilitating, I now spend all my time at home or at the doctors office. It is very hard to treat someone who has a reaction to everything and there isn’t a lot they can do for me, and so I rely on God to guide me through this. Look forward to hearing from you.
Cynthia, Hopefully by next week, we can be in touch by email! I know what you mean about healing being a full time job. I really think the foods that SIBO doctor told you to try (pasta!) contributed to your SIBO coming back. I know “brown rice pasta” is listed in the tables of Fast Track Digestion: IBS, but that is a specific brand, and honestly foods like that will have a higher FP than is even listed in the table, assuming one has severe SIBO which I think you and I would agree that you do. I think it would be so much easier if you could design your diet completely around the scientific data in the Fast Track Diet. For now. If you diverge and follow other doctors recommendations (about diet specifically, not necessarily other things) it can be very confusing. Norm has often said these trials need to be done in a controlled fashion. And if you have issues from there, then we can trouble shoot. My first thought is that you need to get to a better baseline so you will know which foods are bothering you. This is what I had to do. For only 1 or 2 weeks, I am taking out ALL grains and starches, nuts, fruits and increasing my fats and not my protiens. The pasta is not going to be good for your SIBO. Also the peas are listed as a HIGH FP food, so I would take those out. Do you tolerate summer squash (yellow crook neck and zuchinni?), butternut squash (that one might be hard) and avocado? Those are nurishing and lower in FP, although you don’t want to go crazy with them but they can help with your weight. Certainly some grass fed butter (such as Kerrygold butter) and tallow (just the good fat in your beef) would help you keep on the weight. What about small amounts (tablespoons of full-fat greek yogurt?) In terms of digestability, this is going to sound funny, but whole cuts of fatty beef (and fish) are probably easier to digest than ground meats. This is mentioned at the website gutsense.org. You might go have a look at this website, it is very interesting, if only for the great info on the functional anatomy of the gut. We actually have to chew VERY WELL whole cuts of meat, whereas, with ground beef, I think I don’t chew ground beef as well and swallow larger chunks. I always feel I digest ground beef poorly and early on it was giving me heartburn (I think). Just something to play with. You need the fat, so fatty cuts of steak will be best for you. If you could stand taking out the rice for 1 or two weeks it would allow the cleansing waves in your small intestine to take out more bacteria and then you could try the 1/2 cup of rice that Norm recommends and see how that goes. Norm has also recommended to rest the gut 1 or (early on) 2 times per week, by not eating breakfast. You don’t necessarily have to eat fewer calories that day, just rest your gut in the morning so it can rid the upper SI of bacteria, in case there is an issue there. We can talk off line about some of the specifics about herbals. Let me know your thoughts! come over to the Forum because I think it is a better place to talk detail than this thread. Under Auto-immune conditions, the IC tab. See you there!
Hi Norm,
I am just now finding your site and reviewing. Thankful to come across the work you are doing. I was diagnosed with SIBO in 2012. Really got it under control last spring after series typical antibiotic treatment. I think both the SCD and FODMAPs diet helped the most. I am not 100% there yet. Seems to be coming back this holiday season. My biggest challenge is in finding a doctor/medical guidance that KNOWS Sibo. I live in Southern Maine and have seen GI’s from Portland to Boston. Curious if you would recommend a specific practice. Currently with BI (they are fine, love to order tests, outside of breath test, and prescribe medications). Appreciate your insight. When I saw you went to UMASS- Amherst (as did I) and Tufts, I felt it was worth the ask.
Happy Holidays,
Christine W
Hi Norm! Are you following this research study for the erradication of Methane microbes? VERY EXCITING. I think they are in Phase 2. I wish they were done!!
https://www.syntheticbiologics.com/2014-06-25-Synthetic-Biologics-Reports-that-Licensor-Cedars-Sinai-Finds-Eradication-of-Gut-Methane-Improves-Insulin-Sensitivity-and-Lipid-Profiles-in-Study-of-Pre-Diabetic-Obese-Patients
Hi Norm.
I’m a 19 year old girl, and I’ve been having trouble with my digestion for approximately one-two years now, though I think it’s been something going on since I was a kid (I had a lot of sudden cramps as a child, but I don’t recall any other problems). My most reoccurring symptoms have been mostly severe bloating, constipation, flatulence, cramping and some exema/mild acne around my mouth, on my scalp and on the upper part of my arms/upper part of back. I’ve done the CDSA 2.0 test and know that I earlier had an overgrowth of E.coli and Citrobakter Freundii and also no growth of lactobacillus species.
It was treated with Flukonazol and Uva-ursi, which is a treatment I wish I hadn’t done because of latter research on the two.
I am to take the SIBO breathe test in a couple of days, but I’ve been pretty positive I’ve got SIBO for a long time now due to my symptoms and the broad research I’ve been doing. I’m also diagnosed with IBS, but that has seemed pretty irrelevant, because every person with my symptoms fit into the “ibs-box”.
I’ve had a positive result in relieving my symptoms with a combined FODMAPs and SCD diet, but still it all takes very much time and the difference in trigger foods is so vague that it’s very hard to tell WHAT food is causing my problems (all though I know that proteins and fat are a lot easier digested for me, especially because I supplemented with Pepsin&HCL a half year ago). So basically what I’m trying to say is that inconsistency in what I read and in what different experts recommend is the most frustrating part of this SIBO-thing, well except for the symptoms in my everyday life.
It’s a lot more to tell really, but I’ll try to get to the point.
I’d love to order your book, but I’m from Norway and it doesn’t seem to ship all the way here. Another thing I’d like to ask you about is if you have any experience to share on herbal antibiotics. I’ve been using Neem for three weeks, olive leaf extract for three weeks (and seemed to have die-off reactions from it, but now it’s kind of worsened and hasn’t gone away still one week after the use of olive leaf) and I’m planning to do some oregano oil as well. This has truly been symptom relieving, especially with my bloating and constipation, but then it seems worse again now that I take nothing. Do you have any knowledge on this matter which you could possibly share with me? I’ve read the most of this thread, and I must say I find it very informative and helpful.
One last thing. I am a heavy sceptic and I’m a bit scared that the more I dig into the issue of my digestive problems and different diets, the more I turn it into my reality and make it worse. I’m under the impression that the power of placebo/nocebo is overwhelmingly strong in the case of IBS (a new “popular western problem” maybe), and I think there are huge amounts of money in it for alternative doctors and holistic health practitioners (please don’t take this personal) – which honestly makes it hard for me to trust all the diets and helpful people out there and all the books that “have the best diet!”
Also treating SIBO is extremly pricey, and I am too young to pay it off properly myself, which is why most of the treatment and research is done by me alone without a health care practitioner. Would you possibly have any general advice for me? It would be highly appreciated.
I hope this wasn’t too much of a brassy and messy post, I’m having a hard time expressing myself on the subject in a few, clear words. I really do appreciate finding this site and the information you provide, and truly appreciate the research you are doing.
Have a wonderful new year!
Mirea
Hello Mirea!
Sorry that you have to deal with all these in such a young age. I hope you will take back your health soon!
I just want to advice you to buy a Kindle edition of the Norm’s book. I am from Russia and for me it is easier to order electronic books because not all sellers send items to Russia.
Happy New Year!
Wish to all of us Health in 2015!
Hi Mirea! I wanted to let you know that I have been working on ridding myself of SIBO. I bought the kindle version of Norm’s book and it has helped me. I wrote a blog post on what I am currently doing diet wise here: https://familyhomeandhealth.com/2014/12/can-eat-sibo.html. I will also be posting on more specifics on my SIBO treatment in the future. I hope this helps!
I would like to thank you both Alexandra and Kristie for your quick, encouraging answers. I appreciate this a lot! I’ll check out your blog post asap Kristie, thank you!
Regarding the kindle version I’ll look definitely look into it, but I must admit I am having a hard time reading books electronically on my iPhone/computer.
and another quick question for Dr. Robillard;
https://eatingoffthefoodgrid.blogspot.no/2013/10/resistant-starch-and-sibo.html?q=Resistant&m=1
This blog post supports Resistant Starch in the case of SIBO with pretty good research (that’s what it looks like to me, at least) and suggests that the RS moves too fast through the small intestine into the large intestine to actually cause SIBO. but it feels contra intuitive compared to the fast tract approach you present – do you have any thoughts on the subject you could share?
As I mentioned earlier,all the different research and inconsistensy on the internet makes SIBO very tricky to deal with “the right way” on my own.
Cheers and thank you again,
Mirea
Hi Mirea,
Your not alone, SIBO is incredibly common. I am convinced that limiting fermentable carbs is the best approach for getting SIBO under control. You can buy the Fast Tract Digestion print books on this site here (https://digestivehealthinstitute.org/buy-books/) and it does ship to Norway.
The resistant starch link you cite was excerpted from a mini debate between myself and Tim Steele. You can read the entire debate in the protein power link at the beginning of the article – it’s in the comment section. I highly recommend you read my two part blog article on Resistant starch here: https://digestivehealthinstitute.org/2013/05/10/resistant-starch-friend-or-foe/
I also discuss RS in this interview with Paleo Magazine. https://paleomagonline.com/paleo-magazine-radio-eps-38-resistant-starch-take-two/
You may be interested in this article effectiveness of herbal antibiotics for SIBO: https://www.ncbi.nlm.nih.gov/pubmed/24891990
Hi Norm
I appreciate your thinking that moderate alcohol consumption can be safe and does not negatively impact SIBO. I get very frustrated with my holistic doctor in her stance that any alchohol is bad for the liver, and therefor should always be avoided. In our culture this seems so extreme, especially if one is moderate. She claims her patients suffering from gut heatlh issues will likely relapse if they drink regularly. But she does not track the particulars: Are these people drinking sugary alcoholic drinks? Are they consuming excessive amounts of sugar, and consuming sugar along with fermentable carbohydrates? There is nothing scientific in her assessment of relapse, and patients are likely to be exposed to multiple risk factors. She has this blanket recommendation that creates a lot of stress and conflict for me! Are there studies that show that moderate alcohol consumption is damaging to the liver? And even if there is, is it safe to assume that this research would be confounded by diet? Thanks for any thoughts!
Hi Bearsmom,
I am not aware of studies showing moderate alcohol is bad for the liver. But good point about having awareness of other dietary factors (especially sugars and other carbs) that could be involved. Unfortunately, most of these studies are observational studies based on questionnaires about what people consume. These studies may help generate hypotheses, but don’t offer much more. And hasn’t moderate alcohol consumption been associated with longer lifespan?
Hi Norm.
I’ve struggled with GERD and IBS for over 12 months now as PPIs didn’t work. Tried your Heartburn diet a year ago when had GERD and worked amazingly well but 2 weeks later while GERD symptoms had mostly gone was got bad IBS for a week. GI said it was probably gastroenteritis. In Feb last year, I tried the diet again and got great relief and went off PPIs. Have been following the diet on and off for a year. Trouble is that when I start to feel better and add back things like croissants, I get symptoms back bigtime. Also, while I have been back on the diet again for last 4 days which usually makes me feel amazing, I have strong IBS symptoms today on day 4…yet am following the diet to a T plus taking Probiotics twice a day. So, my question is: shold I be following the GERD or IBS diet? I don’t have diabetes, cystic fibrosis, celiac or any diagnosed underlying conditions. Can you suggest anything?
Megan
Hi Megan, Gastroenteritis can have long lasting effects triggering SIBO, IBS etc. Eventually things should improve if you are following Fast Tract Diet, limiting fermentable carbs and using pro-digestion behaviors outlined in the book.
Eventually, you may tolerate some (not a lot) of the foods you crave such as croissants, but you really should go by what your body tells you. It’s possible you will be sensitive to most wheat and other grain-based foods for the foreseeable future.
The important thing is understanding the types of foods that can trigger symptoms so you will have more ah ha moments after eating them.
Either FTD Heartburn or FTD IBS will be fine as the underlying principles are the same. They both employ the Fast Tract Diet and include the food tables.
Hello Norman,
I have just purchased your book , am 2 weeks into the diet plan and already feeling better. I have just a couple of question but will start with a quick snapshot of my symptoms.
I became ill 14 months ago and after many tests (results normal) was referred to a gastroenterologist. He suspected SIBO which linked to food poisoning I had 2 years earlier. I then developed a chill in my left kidney and bingo, SIBO took over. I lost over a stone in weight, developed intolerance to fructons, gluten and wheat. I have suffered swollen veins, an erratic heartbeat and one day I eventually collapsed – which I believe was toxic shock reaction. I felt starved and suffered Fibromyalgia and depression. If I had a gun I’d have shot myself. How on earth people live with this hell for years is beyond me.
My consultant prescribed Rifaxmin and recommended the FOD map diet. I made some improvement and gained 5 Ibs. I was later prescribed VSL#3 probiotic. This too has helped but some symptoms remained and so it occurred to me that SIBO was still resident, so what to to do to drive it out? I decided to do some research and came across your site. I figure a microbiologist should know how this bacteria survives in the human body and how to drive it out. Your book makes absolute sense and has without doubt saving my sanity and my life. So thank you from the bottom of my heart.
Q. I found 20 fp per day not effective enough and was still dehydrated so have reduced between 16-18 per pay day. How long do you recommend? 2 weeks of more?
Q. I have read that L-glutamin can repair damaged intestines. Would this be helpful or interfere with natural recovery . How much and when is advisable to introduce ?
Thank you again.
Tracey
Hi Tracey,
Great you are reading the book. Keeping FP low, embracing pro-digestion behaviors described in the book, cutting overall carb levels early on, avoiding antibiotics unless absolutely needed along with drinking plenty of water is a solid approach.
L-glutamine may be generally beneficial, potentially improving leaky gut and protecting against infection. Doses of 3 to 30 grams have been used, but I would stick with the lower amount since L-glutamine is an amino acid supplied by dietary proteins so you will already be getting a good amount on the Fast Tract Diet.
Hello,
I was diagnosed with SIBO several years ago, after a lifetime of IBS, chronic stomach pain, bloating, and other health issues like PCOS. I have tried the SCD and other diets, but my body seems to become immune to them after a while. As a last resort I tried the Neomycin and something else, and my test results were improved. After a few months my test showed the SIBO had increased again, and I was sicker than ever. Do you have any recommendations or advice? I have spent thousands of dollars on doctors, treatments, etc, and am desperate. Perhaps the SIBO is not the issue? Any advice or feedback would be so appreciated!
I can imagine your frustration Jessica. We can help, but to offer individual advice, you will have to enter our program.
Thank you for the info Norm, I will look into it!
Jessica
Ordered the ebook two weeks ago for my teenage daughter. It has been very helpful as the SCD and FODMAPs diets were leaving her symptomatic and frustrated. My concern is that she loves raw veggies much more than cooked. I keep telling her that cooked are easier to digest, but she points out the small difference in the FPs for cooked vs raw carrots on your chart and crunches away. Is too much raw going to hinder recovery even in FPs are kept in check? Are the FPs for the other veggies on your table for cooked or raw (cabbage, peppers, broccoli, etc)?
Hi Bonni,
This is a good question that I am often asked. I don’t think it will matter that much for lower carb veggies (the carrot example shows it’s a matter of a couple of grams). It would matter much more starchy vegetables such as peas, corn, plantains, grains, most root vegetables, and tubers that contain more starch. In those cases, I recommend well cooked. You can always cut back on serving size and switched to cooked veggies if symptoms persist.
Hello Norman,
I’ve purchased plant based digestive enzymes, took one just before my meal and instantly became bloated so I wonder what caused this. The manufacturer is Nature’s Best (UK product) and contains; lipsase, amylase, protease, glucoamylase, cellulase, bromelain & papain. Tablets shell contains rice bran. I won’t if you could advise?
Thank you,
Tracey
Hi! I’m doing great on the Fast Track Diet after years of disappointment with OTHER diets. My digestion is now as perfect as I can imagine and I now know which foods can trigger symptoms! It all makes so much sense. One question: Is Acesulfame K a safe artificial sweetner like splenda is? Thanks for studying these issues for the rest of us!!
Hey Darryl, Glad you’re doing well on the Fast Tract Diet. Sorry that I have not researched this sweetener sufficiently to offer an opinion on its safety. When in doubt, I lean towards natural non-sugar sweeteners.
I have SIBO and have just read your book “Fast Track Digestion” IBS.
I went to buy Jasmine rice and discovered there is brown and white.
Can you please tell me which one you recommend?
thank you for your time.
Hi Sandra,
Since there is not glycemic index data available (that I know of) for brown jasmine rice, I would stick to white. Once your symptoms are under control, you can experiment with the brown.
Hi there,
I have had SIBO for about 2 years. I have been treated with Rifxamin twice and SIBO came back shortly later. Diet seems to be the best answer. However, I still have SIBO and now I am pregnant so SIBO symptoms are worse. The GI doc and perinatologist are concerned and not sure how to help me gain wait… I am loosing weight and getting skinnier. Thus, the concerns are for my health. And if the baby is getting proper nutrition… I know OB docs say babies are super great “parasites” but it can’t take from me what I don’t have such as fat soluble vitamins or B vitamins). I have tried multiples but ugh I can’t keep them down and make me vomit even if I take it with food.
That said, do you have suggestions for me to maintain or gain weight?
Suggestions for any kind of safe treatment or ways to manage SIBO while pregnant?
This is super new territory for my docs and I could tell they were at a loss. Not reassuring when I have other health complications as well.
Any suggestions are appreciated, but I know most folks don’t like to advise pregnant folks. If you know of any helpful information please pass it along.
Thanks!
Hi Andrea
Congratulations. Firstly I should say that i have never been pregnant so it is far from my area of expertise. I have however had SIBO for a number of years because of another rare condition. I vomit and have severe acid reflux whenever I eat anything at all. I have had two or three rounds of rifaximin with neomycin and metronidazole in for good measure. Neither of these things have worked. I hate to say the FT diet hasn’t worked either but I think thats because I have a very complex condition that is not going to be solved by diet alone. Anyway to get to my point. I am fed via TPN, this is a liquid feed given intravenously via a portacath. This sounds scarier than it is but its only a position of last resort if you became dangerously underweight or there was any thought that your nutritional intake could not support your baby – the doctors would then consider this, probably after giving you all sorts of other oral dietary supplements (e.g. ensure) which may or may not agree with you because of your SIBO. Not sure whether than helps you or not but in the hope of sharing info….
Hi Andrea,
SIBO can definitely make it difficult to absorb sufficient calories, minerals and vitamins. If you have not read FTD IBS, I suggest you do as this issue is discussed in the book. Limiting hard-to-digest carbs and the other strategies in the book are very important in for controlling SIBO. When SIBO is controlled nutrient absorption improves. Because the diet limits some carbs, other easier to digest (low FP) can help replace the lost calories. The rest of the lost calories can be made up with increases in protein, but especially fats. Vitamin and mineral supplements may be part of the solution, especially while SIBO is active.
Hi Andrea, I’m wondering how your pregnancy went with SIBO? I’m 8 weeks in, and struggling with all these issues. I haven’t lost weight but I’m concerned about nutritional malabsorption and other complications such as bacteria-related toxicity and inflammation in the gut. If you have an acquired advice which you could now share I would appreciate it!
Hi Andrea!
Congrats on your pregnancy! I hope you can come over to the forum and post diet questions you can get some on going support. Have you read the book Fast Track Digeston:IBS? I think it will help you get the diet dialed in. You can reduce your fermentable carbohydrate consumption and limit portions of safe starches but still eat enough food to keep you going. You may find you need a snack and once you read the book you will know what safe snacks you need. I think pregnancy hormones slow down paristalis as you go through the pregnancy and I am sure that is not helping. The intro diet (modified to suit your palate) would be a good guide. I think this approach is a safe one for pregnancy and post partum as long as you eat enough food. the sooner you start the better, as this will Reduce the SIBO and help you start to absorb more nutrients from your food. My understanding is whatever nutrients your body had already stored at conception are what the baby has relied on. Vitamin supplements during pregnancy when you have SIBO may not be very helpful. You can have a look at SIBOinfo.com, as Dr. Siebecker has listed some safer vitamin supplements that might be tollerated even when you have the overgrowth. I hope you read the book and post specific diet questions in the forum. Lots of people to help you. Best of luck!
Dear Norm, have you found that the Fast Tract Digestion diet is as successful for people suffering from GERD with hiatal hernia vs. those without a diagnosed hiatal hernia?. My hiatal hernia was confirmed in 2009 via an endoscopy and I have been suffering from GERD symptoms on and off since 2009 (I am 52 yrs old), although up until mid 2014 symptoms would come and go with no change in my diet or meds. I had another endoscopy in 2013 which found antral gastritis but no oesophagitis. I started taking PPI meds in November as my symptoms became constant and more intense but wasn’t convinced by the rather vague explanation from my consultation as to why taking them for 3 months and then trying to cope without them was going to make a difference especially as I have had a hiatal hernia for many years and my symptoms go away for months and then flare up. My symptoms did infact came and go on the PPI meds but were not so intense. I decided to stop PPI meds 2 weeks ago and have been following the Fast Tract Diet guide (not the actual receipes but using the FP guide). My symptoms have increased in some ways but also lessened in others. I am going to persevere with the FTD diet but was wondering whether you think it could be as effective for someone with a hiatal hernia? Thanks
Hi Katrina,
Thanks for reading Fast Tract Digestion. Having a hiatal hernia is a bit like wearing tight clothes or being pregnant. Because the hernia is essentially the top part of your stomach being pinched above the diaphragm, there is often extra intragastric pressure (pressure in your stomach) that can trigger reflux. The Fast Tract Diet is designed to reduce this intragastric pressure at the source – gas produced by overgrowing bacteria in your intestines which is fed mostly by unabsorbed carbohydrates.
There is every reason to believe that the FT diet will help even in the presence of the hernia, but you might have to be extra diligent reducing FP points even more, following the proabsorption behaviors in the book or even lowering overall carbohydrate consumption to reduce the gas pressure as much as possible.
Hi Norm, thanks for your prompt response, is there a specific chapter in your book that covers proabsorption behaviours, or is it generally avoiding the key five culprits of SIBO. I bought some wheat, gluten and milk free brown bread but it contains tapioca and potato starch, and rice flour, as I am still trying to get to grips with what I can & can’t eat am not sure if that is OK because of the starch?. I live in London, if anyone knows of a dietician or nutrionist there who is knowledgeable about the Fast Tract Diet please let me know, thanks
Chapter 12 in FTD IBS and Chapter 10 in FTD Heartburn include the pro-digestion information. Try the bread in small amounts (one slice per meal) and chew each bite to completion. Generally little or now bread is recommended if symptoms are still present, but rice, potato, tapioca based breads are better than wheat-based for most people.
Norm, I cannot thank you enough for having done the research on this and publishing your book. I have lived with IBS all of my life. After going through a bout of C-diff after an operation, my IBS became considerably worse. I tried every diet out there: SCD, GAPS, low FODMAPS, low histamine, low salicylates, etc. but nothing worked long-term. I’ve tried every probiotic as well. It felt like all I did was think about food and its effects on my digestion, pain and bloating. After finding your web site, ordering the book and following the diet for the last two weeks, it is the best I have felt in 7 years. Sincerely, from the bottom of my heart thank you. I finally feel like I have my life back.
Hi Lisa,
Thank you so much for your positive feedback! Helping people get well and feel better is what this grass roots effort is all about. The word is spreading : )
How come honey, which is high in fructose is allowed on your diet in the fast track book?
Hi Anna, The book actually says to limit fructose-containing foods including sucrose, honey and maple syrup. But technically no food is illegal. It’s all about counting the FP grams for the serving sizes of any food and making sure the overall FP points are within the limits for individual meals and overall daily totals. For example, if you have one teaspoon of honey in your tea in the morning you will add about 3 grams of FP. Not too bad, but it can add up if you use too much.
Yes, i’m realizing that even the “low” foods can really add up if you count the grams. For example, butternut squash is rated as low, but when I calculated the FP grams for half a cup of butternut squash soup, it jumped to 33, so it does not leave much space for other foods in the day, if you have half a cup of soup for lunch. It seems like the grams add up pretty fast.
You mention that one of the underlying conditions for SIBO is low stomach acid and one recommendation for this is to take Acid supplements like Hcl. However, these supplements are usually taken with the consumption of protein and are not recommended to be taken with fruits and vegetables. The same goes for digestive enzymes. Plus, even if someone has enough acid, you say in your book that these FODMAPS are simply undigestable carbs, so why does stomach acid matter? Isn’t it the case that even with the proper amount of stomach acid, the ferment able foods are not digested by the body because of their very nature, or are digested slowly?
I have an irritated stomach lining (gastritis) so I dont want to take Hcl, but, I have found that chewing gum for half an hour after meals helps prevent heartburn. However, based on your book, sugar free chewing gums should be avoided bec of their sorbitol or other type of sugar content, so what kind of gum can I chew?
Also, I hope your next book will get more into treating underlying conditions that cause sibo.
Hi Norman,
After reading your IBS book – i wonder what do you think – is it possible to diagnose SIBO using glycemic index and glucose meter. I live in eastern Europe – no doctor here ever heard about SIBO – no way to test for sibo here. My question is – how can i be sure that eating sushi rice /or jasmine/ is not feeding bacteria in gut /upper part of bowel / – in you book on page 202 you give GI of jasmine rice 109 – so lets say i eat specific amount of sushi/jasmine rice /maybe 50 gr/ and measure blood glucose 1 hour later and if it reaches specific value – does this means that rice is properly absorbed and so there is no bacteria at least in the upper part of small intestine. I guess this will not work for lower part of intestine. I need reliable source of carbs in order to avoid thyroid problems.
I will be thankful if you tell me your opinion.
Hi Pesh,
Interesting idea. Breath hydrogen is inversely related to blood glucose response, so technically you should see a smaller blood sugar spike if you were experiencing SIBO/malabsorption. Here’s a link where they measured this. As for thyroid problems and low carb diets, I have read no studies showing that a low carb diet damages the thyroid. I would be interested if you have a source supporting this contention.
Hi Norm,
Thought I’d direct you to a Anthony Colpo’s site where he talks about the dangers of Low Carb diets and the thyroid. It is certainly an issue with T3.
https://anthonycolpo.com/is-a-low-carb-diet-bad-for-your-thyroid/
Here is his summary:
“All the above mentioned studies examined the effect of altering carbohydrate intake on thyroid hormone levels. The results are virtually unanimous: decreasing carbohydrate intake to low levels results in diminished levels of T3 and/or increased rT3, something most aspiring fat-burners wish to avoid desperately.” (Of course, diminished T3 and increased rT3 is vitally important to us sluggish thyroid folk too!)
I try to keep my carb intake at 125 grams per day. It’s still ‘low’ but adequate for thyroid health.
Also very important for thyroid health is to greatly reduce Polyunsaturated Fats – Omega 6 AND Omega 3. The love affair with Omega 3’s is due to our way too high consumption of Omega 6’s. These 2 fatty acids need to be in balance with each other. The healthy way to achieve this is by reducing Omega 6’s not increasing Omega 3’s. I do take a quality fish oil (because I don’t eat much fish) but minimal amounts. Fish oil is still a PUFA.
Saturated fats support thyroid health.
I can’t recall where I got this info but here it is nonetheless:
“Omega-6 fatty acids may suppress thyroid signaling. Corn oil greatly suppresses the liver’s response to T4 when compared to lard; safflower oil suppresses the liver’s response to T3 when compared to beef tallow; and linoleic acid suppresses the response of brown fat and the liver to T3. In fact, in the 1970s researchers were considering omega-6 lineleic acid as a treatment for hyperthyroidism.”
Thanks Lana, I’m with you on the omega-6 issue, but I recall reading that lower T3 was a normal adaptation to lower carb and not a problem. But I’m curious about what Anthony has to say. Let me check it out.
Yes, if you listened to the Safe Starches symposium, that was the argument of Ron Rosedale which did make sense. Paul Jaminet had a different take – which also made sense!
Just in terms of symptoms – low T3 and high rT3 is no fun.
But perhaps if a person had no issues, ate a perfect diet, was calorie restricted and very low carb – it might work regardless of the T3 issue!
For myself, I’m sticking to moderate carbs – which is probably the wise choice for those of us with thyroid issues.
My newest research is on Oxalates. Oh my goodness Norm! I might have to stop nibbling on chocolate. :(((
Thank you for the link Norm- exactly what i needed!
Regarding thyroid – i get this idea from Ray Peat /www.raypeat.com / – i have not read any studies. Also when i try to eat only meat and eggs /FP = 0 / my hair begin to fall – but it is possible to be because i did not eat enough fat.
Hi Pesh
I am not sure I can answer your question regarding the glucose meter. However, I personally never took the lactulose breath test because A. I did not want to consume lactulose, and B. the results would not likely change my approach to controlling symptoms. For me, the best way I see to control my digestive symptoms for the rest of my life is to limit fermentable carbohydrates. I started with the sample diet in the IBS book. After two weeks, it was clear that I was not even tolerating the amounts of fresh cooked rice outlined in the sample diet. So I restricted this further, I looked at my fruit and nut consumption, and more carefully counted my FP points, including the FP of vegetables. After 3 months of this I am able to add back some rice without lots of symptoms. For me, if I experience indigestion symptoms or gas or bloating, this is a sign my FP for the day was too high, or I was not ready for a new food I introduced. Everyone is different and some people can keep fruit in, or low lactose dairy, or both, whereas others need to remove these and test them later. I think starting with the diet in the book and keeping a symptom journal is important. You will know pretty quickly if you are not digesting the rice well yet.
Norm
Adding to my worries about staying low carb for very long (which I might add, I have had to do, as my underlying reasons for SIBO are quite stubborn and persistent) is the series Paul Jaminet wrote a series about his own discoveries about low carb diets (GI cancers and fungal infections, in particular). Of concern was the issue of mucous insufficiency with low carb, and higher risk of GI cancers. I know a woman who was a strong advocate of low carb diets and was just diagnosed with a rare stomach cancer. (N of 1, I realize, but still….) The second article in his series goes into this. He also has his own theories about why people experience constipation on low carb diets (mucous issues). He advocates a relatively low carb diet (300-400 calories from what he calls “safe starches”). My plan is to reintroduce carbs, per your suggestions, when my body will tolerate them. I realize Jaminet tends to lump all potatoes and rice in the same catagories and that this issue is more nuanced when it comes to resistant starch and SIBO. https://perfecthealthdiet.com/2010/11/dangers-of-zero-carb-diets-ii-mucus-deficiency-and-gastrointestinal-cancers/
Hi Norm,
I’m waiting for your book to arrive (I live in france and it’s taking forever!) I have atrophic gastritis due to SIBO and based on the hints I’ve come across on this site I’ve been trying to expand my very limited diet. I was doing great having reintroduced squash, mushrooms, melon and strawberries, when I began to have pains in my shoulders (I get this when the gastritis is flaring) and loose stools. Obviously I’m not following the diet yet as I don’t have the book, but I consider my carb intake very low (no potatoes, no rice etc) is it all down to quantity? and I know I should wait for the book but I’m impatient to get well.
Hi Kerry!
It would be helpful if I knew what you were eating (types of veggies, amount of fruit, are you eating low lactose dairy, how often are you eating squash, how much, etc…) If you come over to the forum you can post in the Fast Track Diet section of the forum and ask specific questions. I think it is helpful to start with the sample diet in the IBS book, unless you know there are foods you are not tolerating. You also will want to learn how to calculate the FP for a given day’s worth of food so that you know you are within limits that are working for your body. Getting down to a specific level and then giving your body some time to adjust is helpful, while keeping track of food intake and symptoms. I think the hope is that this diet not be so limiting. I found I did have to limit carbs at the beginning but now can have a few and feel better when I do. I hope you can come to the forum!
Which Protein powder is safe to take? I follow the diet, but at 85 lbs, need to gain some weight or at the very least, more strength!!
I am lactose intolerant.
Hi everyone,
for about 2 years that i suffer from horrible abnormal bloating, constant tingling sensation in my stomach and upon all of that i developed a hard lump that goes outside the skin of the stomach in the upper area that started to appear when all the issues in my stomach appeared and it gives me horrible nausea. I went to countless doctors and did all the tests and even laparoscopic surgery to check if the lump is a hernia and it’s not and the doctors don’s know what could it be they say everything is “normal” all the tests are ok and they told me maybe it’s IBS but i think it’s much more than that, the hard lump and the pain and gas and bloating keeps on appearing i have no idea what could it be but ever since it has started my whole digestion is ruined. everything seems to irritate me. i tried the fast tract diet which helped a bit but still this thing doesn’t go away and it wakes me up almost every night with horrible nausea.
Does someone know what could it possibly be ?
Hello Dr. Robillard,
I just stumbled upon your site and just got your book so I haven’t had a chance to read it. I am currently on a combined SCD and low FODMAP diet. I’ve been diagnosed with SIBO even though I have no IBS symptoms. I have regular complete physical checkups and all of the doctors I have seen over the years have always told me that I am a picture of perfect health so this diagnosis was quite a surprise. I went to see a naturopathic doctor because I wanted to try a different approach to health care based on all the literature and health and nutrition podcasts that I have been reading / listening to. Another reason I went to see her was because I have some persistent rashes that all my other doctors said was eczema but no one is trying to figure out the underlying cause of my eczema. In any event, I have been on this diet (gluten free, dairy free, no sugar of any source (including honey), no grains) for five weeks and I have experienced zero difference and my rashes are the same. To make things worse, this diet is causing me constipation – I used to be so regular you can set the clock by it! I am taking the HMF Intensive probiotics, Candida complex, B12, zinc and E supplements. I am at the point where I am thinking of giving up the diet but I will give yours a try. If you have any recommendations or insights, I would appreciate a response. Thank you.
Hi Dr Robillard,
I’ve had digestive issues involving loose stools first thing in the morning, plus bloating, burping etc since I contracted giardia 2 years ago. I took antibiotics for the infection and subsequent testing have shown the giardia is gone, but the symptoms are still there. I’ve also developed problems with shortness of breath which seems worse first thing in the morning, which doctors just tell me is anxiety – this is particularly distressing as it feels I’m not being taken seriously. (For example, this morning I don’t have a stressful day ahead, but my stomach muscles feel contracted and it fels like I have to struggle to take a deep breath.) I’ve been gluten free for a couple of years. ECGs and a heart monitor show my heart is working normally, apart from a benign arrhythmia I’ve been aware of for a few years. An endoscopy shows I have silent reflux and the gastro specialist spent literally three minutes afterwards telling me I have irritation around my esophageal sphincter and suggested a PPI, which I’ve refused to take as this wouldn’t be addressing the root cause. I’ve been seeing a functional practitioner instead who did an extensive stool test (“BioScreen” here in Australia) which showed I have a 97% strep overgrowth and low E Coli. Intensive probiotics don’t seem to have made much difference to these numbers and neither has following a sugar free diet (as sugar free as I can, I still have pancakes made with banana, egg and a little psyllium husk). I’ve done the hydrogen breath test for SIBO which came back negative, but is it a foolproof test? If it’s pretty foolproof, what testing would you recommend from here please? The whole thing is starting to dominate my life which is probably feeding back into the whole thing and maiing me pretty miserable. Thanks.
Hi there,
I have SIBO and candida after years on a ppi. I am currently unable to digest protein—any thoughts? Reflux is still an issue (but doctors said ppi was slowing the motility), and I’ve tried enzymes and betaine hcl, and it just burns me. Would love ideas on how to deal with eating meat or getting protein and wonder why this is so, so difficult.
Hi,
I have been diagnosed with SIBO and IBS and LPR. It’s been over 2 years trying to deal with this. First I went on a gluten free diet which helped with bloating. Next, I tried the “Dropping Acid” diet with PPI’s, which didn’t work. I just finished reading your book and have started your diet. After 3 days I still have all the typical and constant symptoms of LPR. I hope this diet will finally solve my problems. How soon should I see improvement?
Thanks,
Leigh
Hi again,
I forgot to add that I am 5′-4″ and 104 lbs. I struggle to keep weight on. Sugar gives me massive headaches and stomach aches.
Thanks
Hi Leigh, As you will see from reading many people’s experience in the discussion group on this site, but also those posting on the Fast Tract Diet Official Facebook Group, it can take anywhere from 1 to 3 months for LPR symptoms to subside on the diet. This is likely do to the more subtle nature of LPR. Reflux must be controlled for some period of time while your vocal cords and other organs impacted recover. Don’t give up. People are reporting much success.
I have Celiac Disease and despite being gluten free have all the symptoms of SIBO. I did the FODMAP diet recommended by a Dietician and this did help. However I then went back to my normal GF diet and all the SIBO symptoms came back over time. I have only just realised that these symptoms were due to SIBO and having researched lots of diets now have found yours. I have also recently read Amy Meyers Autoimmune Solution. She recommends supplements of Probiotics, l-Glutamine 3,000mg daily and Acetyl-Glutathione 600-1200mg daily as well as vitamins and Omega 3 and herbal supplements. Have you read this book? If so, do you feel the doses of l-Glutamine and Acetyl-Glutathione would be harmful? Are these safe at these levels and are they necessary?
Thank you for your time. Much appreciated.
Hi Norm
I am mainly vegetarian and only include a little chicken now and again, would your book/diet be suitable for me and give me all the nutrients i need?
Many Thanks
Kind Regards
Trudy
Hi, Norm.
Just got your IBS book & have been using the app for a week– symptoms are gradually declining, praise the Lord and many thanks to you.
I have an autoimmune skin disease, lichen sclerosis, and have been following the Paleo Autoimmune Protocol diet for about three years. It has helped tremendously with my symptoms. Last fall when I traveled a good bit, I started to relax the diet, including small amounts of rice, nuts and eggs, and after a few months of this relaxed version of the diet, I developed psoriasis. While researching it, I found that there is an association between psoriasis and SIBO and tested positive for methane-producing SIBO via the breath test. (In retrospect I think I have had this for about 15 years, as I can remember several periods of near-constant burping and it started after a round of Cipro.) I then started a low FODMAP version of the AIP diet, which is pretty close to taking all joy, flavor & variety out of eating. I was also taking herbal antibiotics for SIBO. After twelve weeks of this and absolutely NO signs of symptom abatement, I ditched the low FODMAP part & the herbals since they made no difference. At the same time, I received a Hashimoto’s diagnosis that manifests as hypothyroid. I came across your site and implemented what I learned from it & the app, and it is helping the SIBO symptoms, unlike anything else I’ve tried (in addition to diet and herbals, that includes prokinetics; stimulating the vagus nerve through gargling, abdominal massage, meditation and PEMF (my husband looks askance at all of these things!); avoiding probiotics; using soil-based probiotics;intermittent fasting….)
My question is this: I am eating jasmine rice (usually two 1/2-cup portions per day) because I don’t want to go into ketosis and lose weight. I can see mild break-outs develop on my facial skin (but the lichen sclerosis symptoms are still nonexistent). I am thinking I still have significant gut healing to do, even after 3 years of AIP, because I didn’t address SIBO, and that the rice is showing up on my face. Will including the rice & thus impeding the gut healing process be an impediment for healing the SIBO? Or can I first tackle SIBO, gradually add more foods back in (including more starchy vegetables) and then address gut healing (& take rice out)?
Thanks for your insight & for taking the time to respond to everyone.
Tess J
dIs there evidence that a VLC long term is ok for microbiome? My LDL small particles keep elevating but trying to stay VLC due to sibo and also diabetes.
Hi norm,
Am going to buy your book after what I have just read above, it all makes perfect sense.
I do have 2 questions however;
Would you say your diet eventually cures or corrects sibo or just puts the symptoms into remission?
Also , what is your view on probiotics?
Thanks!
Lewis
Hi Norm,
I read your e-book. It was quite enlightening. Fast track diet is the way to go. Still wondering why I came across your work late. This is 2016! Its never too late though. Thanks again norm.
Hi norm,
I just want that one person and others here to know that I also suffered sulfur burps every so often. It was when my SIBO was at its worst. Basically, you get these burps, followed by bloating, nausea, bad diarrhea, then sometimes vomiting. I don’t eat the rest of the day or it comes back. I don’t get this syndrome anymore because I only eat three times a day, no snacks. No gluten as well. Sometimes my meals have too much FP and I get IBS symptoms half-hour to an hour after eating. But this is how I have to live without antibiotics. I never thought eating so bad before I was 30 years old would cause irreversible damage, but that’s what seems like happened. Good luck everyone. I don’t wish the sulfur burps aka rotten egg burps on anyone.
Hi Norm – You haven’t posted since December, 2015. Is there another site to reach you on? A few years ago I had heard you may be writing another book about SIBO – just wondering if it’s still in the works?