The 3 common questions on SIBO treatment and answers that may surprise you:
Q 1. Don’t we need antibiotics for SIBO as low fermentable carbohydrate diets do not “eradicate” an overgrowth in the small intestine?
Q 2. I am worried about being on low-FODMAP, low-carb diet, Fast Tract Diet, etc. for a long time because I don’t want the bacteria in my large intestine to be negatively impacted. What is your take on this?
Q 3. Since happy and well fed SIBO bacteria are easier to kill with antibiotics, isn’t a diet that starves these bacteria the wrong approach when taking antibiotics? Won’t the bacteria go into hiding and become more difficult to eradicate? Shouldn’t we consume more FODMAPs and carbohydrates during antibiotic treatment?
Answer to Question 1
When it comes to SIBO and dysbiosis, I prefer the term “control” over “eradication”. If you “eradicate” SIBO, you will be also eradicating the commensal bacteria (good bacteria) that are naturally present in the small intestine. Though fewer in number, these protective commensal bacteria should be preserved for healthy digestion. Antibiotics used for SIBO are broad spectrum and kill or inhibit a wide range of bacterial types which will include many innocent bystanders. And while some important commensals will be impacted, some of the symptom-causing bacteria will already be or become resistant and persist.
Regarding SIBO diets, the elemental diet is most effective for SIBO because it is a pre-digested formula that contains no hard-to-digest fermentable carbohydrates (only glucose). The diet also achieved 85% SIBO eradication (if you like the word “eradicate”). This result compares favorably over rifaximin which achieved a success rate of 41% vs 32 % placebo (Target 1 and 2). While the elemental diet was effective, it has several drawbacks including cost, unpleasant taste, absence of whole / solid foods and containing very little fat. Also, the argument could be made that increasing predigested fats (fatty acids) and protein (amino acids) over glucose in an elemental diet formulation might be better for advanced cases of SIBO given that glucose can potentially feed SIBO much more efficiently than amino acids and fatty acids.
My recent blog article also references significant improvements by limiting fiber, fructose and lactose as well as using low FODMAP or low-carb diet for SIBO/IBS-related symptoms.
Except the elemental diet, most dietary approaches do not limit the full range of fermentable carbohydrates described in the Textbook of Primary and Acute Care Medicine. This could hinder their effectiveness for controlling SIBO. However, The Fast Tract Diet (FTD) is designed to quantitatively limit, but not eliminate all five types. The FTD also includes Gut Friendly Practices as well as strategies to identify and address your specific underlying cause(s). Our consultation program uses the same 3 pillar approach to provide customized solutions for your specific SIBO and related conditions.
Question 2
“I am worried about being on low-FODMAP, low-carb diet, Fast Tract Diet, etc. for a long time because I don’t want the bacteria in my large intestine to be negatively impacted. What is your take on this?”
Answer
Clearly you would expect fewer bacteria and less of their end products including short chain fatty acids such as butyrate. This is a natural chain of events because you are reducing bacteria’s primary fuel source, carbohydrates. But that does not mean that bacteria in your large intestine are negatively impacted. And here is why they are not.
Changes in Short Chain Fatty Acid – Butyrate
Butyrate has important functions including anti-inflammatory properties and feeding cells that line the large intestine. But how should we interpret butyrate concentrations in fecal samples?
This study highlighted a drop in certain strains of bacteria and short chain fatty acids (SCFAs) including butyrate in participants on a low carbohydrate diet. But the level of butyrate was measured in fecal samples and was still 8.5 mM. While this represented a 50% reduction compared to the high carb diet, what does this really mean? To me this suggests that butyrate and the other SCFAs are still being produced in excess of what our body needs. Hence they are released in the stool. So I do not see any issue here.
See my response to Jeff Leach’s blog article: “Sorry low carbers, your microbiome is just not that into you”
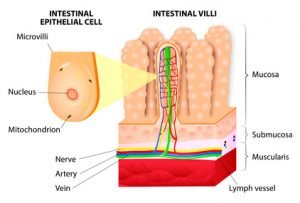
Mucosal Atrophy with Intravenous Feeding
How Your Microbiota Is Being Fed
Unlike the elemental diet, real food diets low in fermentable carbs still provide many species of fermentable carbohydrates. Look at the large number of people who have been on a ketogenic diets for many years. If low carbohydrate diets were causing significant damage to the bacteria in the large or small intestine, you would think we would have heard something about it, at least in some individual case studies.
Even if you eliminated all carbohydrates from your diet, you would not starve your microbiota. This is because:
- Your body continues to produce mucus. Mucus is 80% carbohydrate but also contains sialic acid. Sialic acid is a glycoprotein meaning that mucus provides not only a carbon energy source (carbohydrate), but also a source of nitrogen (protein/amino acid) which is required by bacteria.
- Bacteria can also ferment 20% of dietary protein which escapes digestion thus ensuring its availability for bacteria.
- Consuming animal-based foods also feeds your gut bacteria with “animal fiber”. This is comprised of fermentable elements such as undigested skin, bone, cartilage, collagen and other glycans. Though potentially unsafe in modern times, our ancient ancestors included even more animal fiber by consuming raw meat. For more info, refer to “Duck Dodger’s” comments at the end of my resistant starch article.
In support of the idea that we, and presumably our microbiota can stay healthy with few carbs I found the study of two men who ate nothing but meat for one year with no ill effects to be an interesting read.
Take Home Message
Our bodies and our microbiota are adaptive to capitalize on the nutrients available. After all, our microbiota evolved to help us avoid starvation over many thousands of years. This implies that our microbiota should be fairly robust in the face of dramatic reductions not only in carbohydrates, but in all three food groups. To date, I have found no evidence that low carb diets damage our microbiota or our general health.
The Fast Tract Diet quantitatively reduces, but does NOT eliminate fermentable carbohydrates. The range is from 20 to 45 grams plus per day depending on the severity of your symptoms. Once you get SIBO under control, the damage done to your small intestine should begin to heal. As healing progresses, your carbohydrate tolerance will improve over time and allow for the gradual increase fermentable carbohydrates in your diet.
Question 3
Since happy and well fed SIBO bacteria are easier to kill with antibiotics, isn’t a diet that starves these bacteria the wrong approach when taking antibiotics? Won’t the bacteria go into hiding and become more difficult to eradicate? Shouldn’t we consume more FODMAPs and carbohydrates during antibiotic treatment?
Answer
Here Is Why
The feed to kill concept is interesting. I have read the study about using guar gum with rifaximin for SIBO. The 15% increase in SIBO eradication is certainly something to consider and merits further study. But adding this single species of fiber during treatment is very different from increasing FODMAPs or overall carbohydrates during treatment.
While actively growing (i.e. well fed) bacteria do tend to be more susceptible to the effects of antibiotics, the type of antibiotic matters. For example, ciprofloxacin kills actively growing bacteria better than non-growing bacteria, but daptomycin, a different kind of antibiotic kills bacteria regardless. Also, the specific bacterial species causing your case of SIBO will impact the efficacy of antibiotics. And the type of supplemental fiber may also influence the degree of antibiotic susceptibility.

This is what happened. When researchers gave mice antibiotics, the mice became more susceptible to infection by pathogens. They also measured a dramatic spike in a sugar called “sialic acid”, a normal component of mucus which commensal (good) bacteria use for fuel.
With antibiotics, there were fewer commensals (good bacteria) available to use the sugar because they were killed by antibiotics, and the levels of sugar soared. The pathogens were able to access this fuel source and set up shop. In Sonnenberg’s own words “Pathogens take advantage of a temporary spike in available sugars liberated from intestinal mucus left behind by slain (killed) commensal microbes”.
If you imagine a similar scenario playing out in our bodies – humans have similar sialic acid containing mucus, it seems to me that you would want to be very careful about adding more carbohydrate fuel to the potential fire.
My recommendation is to avoid antibiotics unless absolutely necessary. When they are used, limit overall fermentable carbohydrate levels as recommended by the Fast Tract Diet.
This is the third article on SIBO. If you liked this article, you may want to read:
SIBO Diets and Digestive Health – It’s about Fermentable Carbohydrates






Thank-you for this article giving scientific explanations! I just completed 18 days on an elemental diet for my very resistant SIBO. It was a physicians formula I got through my naturopath (not horrible!) I am now following GAPS Diet guidelines and taking some supplements to encourage healing and restoring of the gut. After only two days I am feeling much better and encouraged. This has been a long road (three years of various attempts to control) I did achieve some success with Fast Tract and appreciate what I learned through it! No matter what, this is not easy! I wish us all Good Luck!
Above in this article it is said “Once you get SIBO under control, the damage done to your small intestine should begin to heal”
I am not sure if I have SIBO but I have gas due to overdose of strong antibiotics. I did not take antibiotics to get rid of these symptoms.
Please can you advise on what I can do to keep it under control to avoid complications?
Hi Joe, While I can’t offer individual advice outside of our consultation program, in most instances diet is the key for getting SIBO under control and healing the gut and also or correcting microbial imbalances after antibiotics. If you have not read Fast Tract Digestion IBS, I suggest you do. Also, there is a section on underlying causes you should also read. Alternatively, the Fast Tract Diet mobile app has an extensive write up as well.
Hi Dr. Robillard,
Thank you so much for your research, as I know many of us are benefiting from this.
On the low FP/low carb diet, I am very quickly starting to see results. As I use to eat tons of fiber enriched cereals, that was part of my issue with SIBO. Wondering in your opinion, how long it might take on average for the small intestine to heal?
Thank you.
If the damage is extensive, for instance with celiac disease, the gut can take many months, even up to a year or more to heal. With typical IBS/SIBO, it should heal much sooner as the damage is typically much less extensive. Of course the SIBO must be addressed by diligent employment of all the FTD principles.
Thanks for your feedback,
Your FTD has helped considerably, and moving forward I will consider it a lifestyle.
As for the discussion on antibiotics, would diet alone be able to kill all the bacteria? I have however read for many people, even after antibiotics their SIBO returns.
The diet is designed to reduce fermentation and the overall growth of intestinal microorganisms, but not kill them. When their numbers are controlled, there is less inflammation and your body’s own immune system along with specific strain feeding via mucus (healthy commensal strains can access the sugars and glycoprotein of the mucus) is better able to sort out the good from the bad bacteria and support the good strains.
Hi Dr Robillard,
You say the overgrowth is not killed and I think it was Mark Pimentel that said you can never really get rid of Sibo without antimicrobials so is your theory once they are reduced the ‘good’ strains compete and push out the ‘bad’ strains? Otherwise how will you ever overcome Sibo? And I’m confused because aren’t they all really ‘good’ strains as Sibo is just healthy bacteria in the wrong place? And what about Mr Pimentel’s suggestion Sibo just go into hiding when their food source is taken away? They’ll just come back out again as soon as more food is available? Don’t get me wrong, your theories have made more sense to me than anything I’ve read in the last year and the FTD is the only thing that makes me feel better but I feel like starving my Sibo isn’t really solving the underlying problem if the Sibo is only in hiding. I’d really appreciate your thoughts – thank you ..and also I have zero Lactobacillus and low Bifidobacteria so taking 900 billion VSL3 no Maltose (I cant have corn as had atrophic gastritis last year) sachets per day (450 billion per sachet) .. am I making things worse taking so much for my Sibo? Shall I cut back to 1 sachet (450 billion cfu’s) and how long would you advise I keep taking? Thank you for helping :)
Hi, in a previous post you spoke about digestibility of amylose and amylopectin. I having been doing SCD for years and it has kept my ulcerative colitis under control. But it leaves me with a lot of side effects from not eating things like rice, potatoes, bread, etc. I’ve recently been experimenting with sticky rice (largely amylopectin), but it hasn’t been working well for me. It causes massive bloating, cramping and activates my UC symptoms again. I’m wondering if high amylose is then the way to go for me, despite its apparent worse digestibility. For examples, most beans are no problem for me, and they usually have arond 40% amylose. Is it possible to find high amylose rice, corn or potato? I know they make a low GI high amylose rice, but it’s still only ~28% amylose.
Hi Bruce, If you find that more RS helps in your case, go for it. Some people do seem to be able to tolerate this more than others. I know food scientists and plant geneticists continue to develop new foods with higher RS. Just not an areas I spend a lot of time on. Good luck.
Thank you for all of this terrific information. My daughter was 8 when we found out she had SIBO. They gave her antibiotics and sent us in our way. No follow up, no diet. We also discovered she has NCGS (celiac test negative). She is incredibly sensitive to gluten in even cross contamination. Her glutening symptoms are not the same as SIBO. Anyway, strict gluten free diet and the SIBO came back but now I know why. We pretty much attacked this beast this time on our own with diet modifications. I followed a modified SCD that turns out is strikingly like the Fast Tract Diet. I have the app and the book should be here by tomorrow. I ordered the book because I needed to know what to do now. How do we continue to manage this condition? I don’t think a gluten free SAD is where we should go.
I am wondering what role the gluten sensitivity plays in all of this? A recent study did show increased intestinal permeability and inflammation in those with NCGS (I don’t have the citation right now). I’m hoping that, by being on top of SIBO and gluten sensitivity now, that we will avoid a future autoimmune condition. I know Fasano cites intestinal permeability as a key in the development of autoimmune disease. My sister, aunt, uncle, and grandmother all have had various autoimmune diseases. No one believes me that diet/gut has anything to do with it.
Anyway, thanks for all of the well-thought out discussions.
Hi Jennifer, Your daughter is lucky to have a mom doing all this research. The cause of NCGS is actively studied and debated. The latest was the idea that it’s the FODMAPs in wheat, rye and barley. That could be a factor and possible a direct role of gluten, but my thought is that it’s is much more likely to the the resistant starch in wheat, rye and barley. And RS is present in plenty of gluten-free foods which would help explain by gluten-free is not enough. Good luck with your daughter and keep our consultation program in mind if we can help.
Thank you Norm. I’m really looking forward to reading your book. I have spent a lot of time on your website and just listened you your interview on the Healthy Gut Podcast. Lots of great information! We will definitely keep consultation in mind. What I like so far about your approach is that it really makes sense to my daughter. She feels like she has some choice and control. Instead of the “illegal” list, she gets data that helps her make an informed decision. And then she can link the effects to the cause should she choose something with a high FP.
I’m sure that resistant starch is a part of things for some folks, especially in the case of SIBO, but I think there really is a response to protein – maybe it’s not guten (there is now some talk of non celiac wheat sensitivity, instead of gluten). When she was diagnosed with SIBO, the antibiotic treatment actually worked for a while. However, when accidentally glutened (we have always been able to confirm the source because it has always been a food prepared by someone else), her symptoms are different from SIBO – the gut reaction with a glutening is intense, terrible stomach pains, she gets diarrhea (her SIBO has constipation with it), headache, fatigue that last for days, and foot pain. We confirmed all of the symptoms when on the gluten challenge for celiac testing. Prior to removing gluten, she could hardly move (she was only 8). Now she plays soccer and tennis. That changes with a glutening. Also, we are Catholic and at church she receives a low gluten host for communion. It is supposedly celiac safe since they test that is below the gluten-free threshold, but is is made from wheat starch (official rule is that the waffer needs to be made from wheat – not going the discuss the hows and whys). No problem at all with that until the SIBO (symptoms of gas, bloating, and constipation) creeps back. Then most starches bother her and the FP reduction has worked wonders. But if it contains gluten, watch out! Simply not the same reaction!
These are just my observations. Not a very exhaustive study :-) Here is the study on NCGS that I referred to above. It was published in July of 2016. I found it very interesting. https://gut.bmj.com/content/early/2016/07/21/gutjnl-2016-311964.full
Here’s another one from 2015 that states that NCGS causes dysbiosis…but I can access the full text so don’t know how they are coming to this statement.
Anyway, thanks again for your work on this. It really is a terrific tool!
Thanks for the links and happy to hear your daughter is data driven Jenn. I ordered the second paper that’s behind the firewall. I can send it to you when I get it if you don’t have it. These are very interesting studies. The one big problem I have with 98 percent of these studies is they say “gluten” but the studies always compare a gluten-free diet to one containing gluten. But there are very big differences besides gluten in these diets. I still believe a big player, if not the holy grail will be resistant starch. If they want to make me happy, they will include a low FP diet arm in these studies : ). And whether its all about the RS or gluten and resistant starch, let’s add a purified gluten arm as well. I can dream can’t I?
Oops…forgot the link:
Non-celiac gluten sensitivity triggers gut dysbiosis, neuroinflammation, gut-brain axis dysfunction, and vulnerability for dementia.
https://www.ncbi.nlm.nih.gov/pubmed/25642988
Have you seen Miracle Noodles? Low carb, all soluble fiber. The packaging shows zeros across all nutritional info. I guess it’s made from a Japanese Yam. I’m trying to figure out if it’s worth a try.
Thanks
Hi Jenn, I believe you are referring to Shirataki noodles from the konjac yam. Yes, very low carb and low FP. The few FP points come from glucomannon a soluble fiber that often is not properly quantified on the label. I have been eating these regularly over the last week during my visit in Japan. I have no problem tolerating these and they are a great addition to any meal.
Hi Dr. Robillard,
I have low stomach acid and have never taken any steps to treat it. Once I start treating, do you know how long it can take to restore stomach acid and the effects of SIBO?
Hi SHB, According to this study, Betaine rapidly restores stomach acidity, but only for a an hour or so, meaning it needs to be taken with each meal/snack. Definitive diagnosis of low stomach acid and addressing the root cause would be important long term as well as identifying and addressing other potential contributing causes of SIBO. If you need support, please check out our consultation page.
Seven years after being diagnosed with Celiac, my wife has now been diagnosed with SIBO. I’ve adapted pretty easily to living a GF lifestyle at home so it is easier on her, but what is the best way to support her now that her diet has even more restrictions? This is all very new to us both, and I want to support her in the way that is best for her. After all, from a married lifestyle standpoint, don’t we both have this?
Hi Karl,
The GF diet is known for restricting all gluten, but this diet also restricts a good bit of fiber, resistant starch and various other FODMAPs. Since almost all GF diet studies do not include an arm that tests the effect of purified gluten, it’s impossible to know if restricting gluten is the only important aspect of the GF diet. Since a high percentage of people with CD on a GF diet do not fully recover, I can’t help wonder if some fermentable carbohydrates in non gluten- containing foods such as corn, certain (high FP) rices, oats, bananas, etc. are part of the problem with symptom persistence. One thing you might try together is a gluten-free version of the FTD. If you need support we can help via our consultation program.
Hi Dr. Robillard,
I have had Sibo and a Leaky Gut (now resolved) after several doses of antibiotics and have been eating mostly Paleo for over a year. I take a Probiotic in the morning and evening and drink Kombucha. I am Gluten Sensitive/Intolerant. Tested Negative for the Celiac Gene and allergy testing. But I reactive severely to gluten or wheat. I have reflux and am trying to back off the meds. My bowels are so much better eating low carb. My question for you is how does the Fast Tract Diet differ from the many variations of Keto Diets? I am trying to figure out the right grams of Protein, Fat and Carbs to ingest a day.
Hi Jesse,
The FTD is based on three pillars – the actual foods and their FP (fermentation potential, based on the glycemic index), – identifying and addressing potential underlying causes, and – pro-digestion behaviors and practices. The FTD is not strictly a LC diet as some higher carbs foods such as certain rices, other grains and potatoes have relatively low FP values because they have a high glycemic index. High GI foods are absorbed more quickly minimizing their impact on fueling excess bacterial fermentation. On the other hand sugar alcohols (except erythritol) and most species or fiber acceptable on a LC diet need to be limited on the FTD.
Thank you
HI Dr Robillard, I am so pleased to find you! Greetings from London England. I am a retired PhD nurse, who has Silent Reflux – probably had it for about 6 months following 2 pretty bad chest infections – lots of coughing – sometimes until I retched. Tested for whooping cough – negative. Symptoms: feeling something in my throat, nausea with or without food, tickle in my throat that makes me cough, sleep very challenging even though bedhead propped up. I have had IBS for over 30 years. Was told only a colostomy could help me, aged 38. Wrong! Diet did. Totally. So I am really hopeful your diet will help my Silent Reflux. I don’t have a Kindle. But I really want to ready your book. Is a printable version available? I have been seen by a chest specialist, ENT specialist, and see a GI consultant next Monday. Are the tests you mention available in UK? Thank you so much! Jane Buckle
Hi Dr Jane, Most tests done in the states are also available in UK, though some are not as easy to find such as hydrogen breath testing. The print book is available on this site and we do ship to UK. But also, the Kindle book is readable on any device/computer with free ebook reader software. You don’t need a Kindle.
Hi Dr. Robillard,
You mention the following in regards to SIBO triggers – Lactose, Fructose, Resistant starch, Fiber, Sugar alcohols. I’ll add that all of these seem to bother me. Where would you categorize process sugar?
Thanks
Hi SH, Processed sugar generally refers to sucrose which is a disaccharide (double sugar) composed of fructose (high symptom potential) and glucose (low symptom potential). As expected, the glycemic index of sucrose (58) is between the two individual sugars. The Fermentation Potential of sucrose is therefore calculated as 2 grams per teaspoon, which is not terrible. But if you have larger amounts (a typical soda has 12 teaspoons of sucrose) the FP points (symptom potential) rapidly increases.
Thanks again Dr. Robillard.
The FTD has been a miracle for me, and I use it as a daily referral.
I tried taking ACV and Betaine HCI to help things along and they made things much worse. I found the ACV just made my symptoms stronger and the Betaine HCI gave me terrible flu like side effects.
Have you heard any of the same reports on these?
Hi SH,
I have not heard of someone reporting flu-like symptoms, but if your stomach acid is not low, more acid is certainly likely to provoke worse reflux symptoms.
Man, Norm, you have blown me away. I have been going down the track of eating and supplementing prebiotic fibres for the last three years and eating ‘healthy’ (fresh, high fiber, non-processed, organic, free-range, good fats – butter etc. gluten free, low dairy) for my large intestine. I have developed GERD, and although I am about to turn 56 and sit in the prevalent range of getting, I am looking for answers.
I am H.Pylori negative. PPI’s worked but I do not, and do not want to, take them anymore.
So I may have brought this on via the pre-biotics foods and supplements. Back to the drawing board stuff.
Plan to get your book and app. Let you know how I go.
Hi Adrian, I’ve been there – many years ago. Let us know how you make out.
Hi Dr. Robillard,
Can you explain what non acid reflux is?
Thanks