Some studies have found PPIs (Proton Pump Inhibitors) are a risk factor for SIBO. And others have found a lack of a statistical difference.
Here are some of the published findings
- This recent study by the Pimentel group found no statistical difference in SIBO between PPI-uses and non-users but did observe some level of dysbiosis. (Also, in this 2016 study).
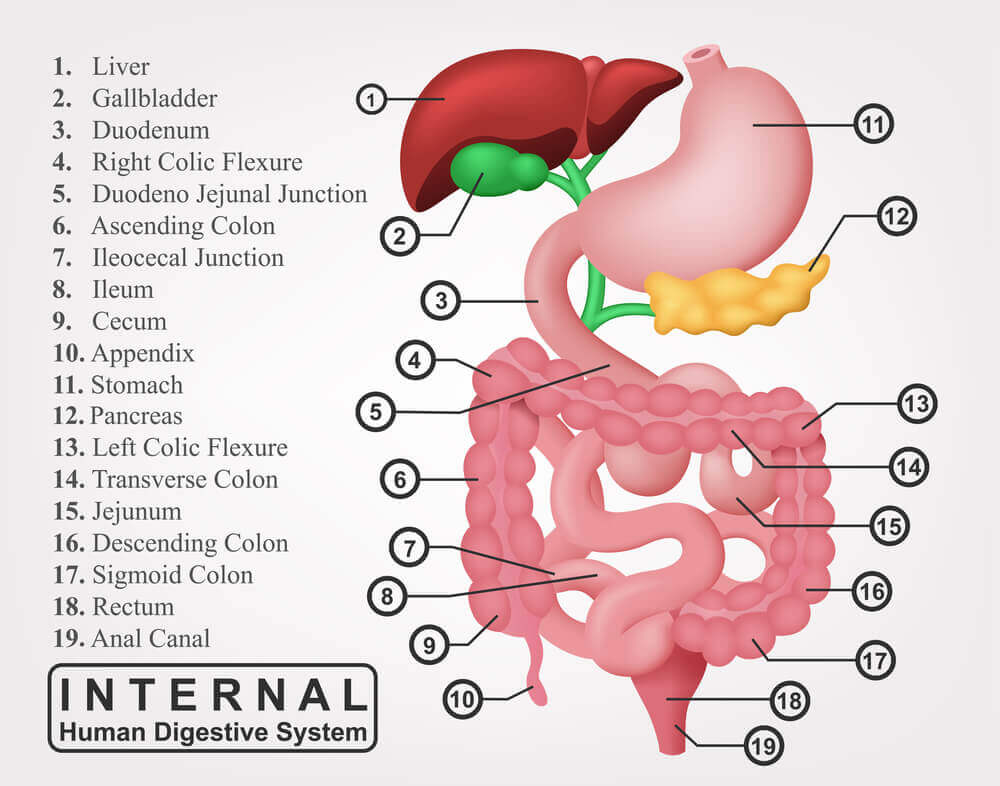
- This 1994 study found that duodenal bacterial overgrowth occurs often in patients treated with omeprazole (PPI).
- This 1996 study showed proton pump inhibitor use significantly increased bacterial colonization of the duodenum.
- In another 1996 study, “Results show that the incidence of gastric and duodenal bacterial overgrowth is considerably higher in patients treated with omeprazole (PPI) compared with cimetidine (H2 blocker).”
- A 2009 study comparing IBS to non-IBS patients identified an increased risk of SIBO in non-IBS patients taking PPIs, but not in IBS patients.
- This 1998 study found that 43% of elderly patients on acid suppression therapy, but not before (either H2 blockers, but especially PPIs) exhibited duodenal bacterial overgrowth.
- This report from 2000 found that proton pump inhibitor therapy in patients with GERD results in a high prevalence of gastric bacterial overgrowth (bacteria growing up into the stomach).
- This 2010 study found that SIBO was detected in 50% of patients using PPIs, 24.5% of patients with IBS, and 6% of healthy control subjects.
- This 2012 meta-analysis concluded that PPI use was associated with SIBO risk, but only when the diagnosis was made by a highly accurate test (duodenal or jejunal aspirate culture).
- This 2018 study concluded that “Long-term PPI use was found to be significantly associated with SIBO (44.8% with PPIs vs 21% control) development as determined by breath H2 and CH4 excretion.”
- A 2018 Meta-analysis showed a statistically significant but moderate increased risk of SIBO in people taking PPIs.
The 2010 study by Lombado et.al reported that “50% of the GERD patients taking PPI therapy, 24.5% of the IBS patients, and 6% of the healthy controls had a positive GHBT (glucose hydrogen breath test).”
I have discussed this paper in the past raising the point that the SIBO positive rate likely would have been higher had lactulose been used in place of rapidly cleared glucose as the breath testing method. The report also makes the point that “most existing studies linking SIBO to IBS have not adjusted for or excluded the use of PPI therapy, which is important since 40% of IBS patients also have GERD and are commonly on PPIs.
Here is my take:
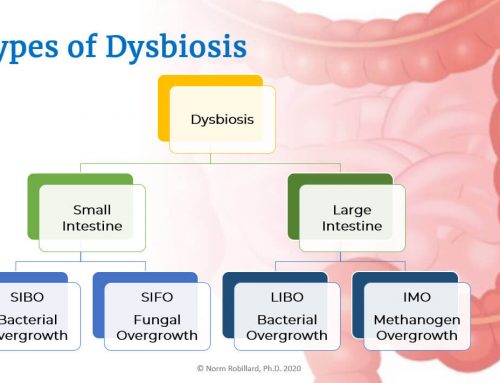
Perhaps the differing findings are because stomach acid is just one of the several control mechanisms (along with motility, proper digestion, brush border integrity, bile level, and composition [PPIs may alter this as well], pancreas function, immunity, etc.) for preventing bacterial overgrowth and dysbiosis in general.
These redundant control mechanisms are protective. Less controversial is that PPI use results in profound overall microbiome changes.
Further, though not relating directly to PPIs, earlier studies in the 80’s linked achlorhydria to gastric bacterial overgrowth (in the stomach) indicating the importance of the acid barrier in preventing bacterial overgrowth.
Bottom line:
Preventing SIBO and other forms of dysbiosis depends on our overall health and keeping our control mechanisms intact. Stomach acid is an important part. To assess your own risk, check out this article and video.
Bonus reading – Here is an excellent review entitled The impact of proton pump inhibitors on the human gastrointestinal microbiome. And this alarming quote “Over half of all inpatients who receive PPIs do not have an appropriate indication for the drugs and, among these patients, over one third are discharged on PPIs”.





Leave A Comment
You must be logged in to post a comment.