Dear President Obama,
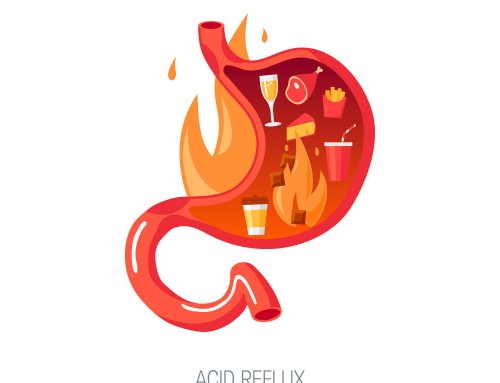
I’m hoping your recent diagnosis of acid reflux might be a teachable moment for you, your team of doctors, and for some of the 60 million Americans who suffer from reflux. The symptoms include heartburn, abdominal pain, cough, sore throat, hoarseness, laryngitis and sinus irritation. Persistent damaging reflux is referred to as gastroesophageal reflux disease (GERD).
I am a Boston-based microbiologist who also struggled with acid reflux, in my case for 20 years. It all changed when I accidentally made a connection between acid reflux and carbohydrates. I decided one day to go on a low-carb diet to lose weight — and my reflux symptoms vanished in a matter of days without drugs of any kind. That was ten years ago.
Since then, I’ve promoted these findings and a modified carbohydrate diet — no drugs, no gimmicks — wherever I can, including at the Digestive Disease Week (2013) annual meeting for gastroenterologists. Doctors habitually prescribe drugs for this condition, and a diet that has little in common with my own, and may not be effective in treating reflux. The drugs they promote are proton pump inhibitors (PPIs), such as Nexium or Prilosec. PPIs can reduce the absorption of vitamins and minerals including vitamin B12 and iron (anemia risk), calcium (bone fracture risk) and magnesium (cardiovascular, neurological and bone health risk). PPIs have also been linked to Clostridium difficile infections and pneumonia.
Why do PPIs work on this problem – at least for certain periods of time? The drugs eliminate stomach acid, even though stomach acid is essential for health and digestion. While they literally shut down acid production and may improve symptoms, they are not recommended for long term use because of side effects and health risks. And they allow us to evade answering the important question: how to keep acid in the stomach where it belongs?
The standard dietary advice for acid reflux includes avoiding fatty or fried dishes, coffee, tea, alcohol, spicy foods, oranges and other citrus fruits, tomatoes, onions, carbonated beverages, chocolate and mint. Unfortunately, according to the American Medical Association’s Continuing Medical Education (CME) program for doctors and gastroenterologists, “Routine global elimination of food that can trigger reflux is not recommended in the treatment of GERD.”
In other words, after reviewing the research, they concluded that trigger food diets are not effective. The fact that these diets didn’t work doesn’t mean that dietary intervention won’t work, but it does mean that the medical establishment needs to go back to the drawing board. The modified carb diet I have developed and promoted over the last ten years might be a good place for them to start looking.
Let’s start with why cutting carbs can eliminate acid reflux. I believe the answer involves the 100 trillion or so bacteria that live in our intestines.
Did you know that certain types of dietary carbohydrates are difficult to digest and absorb into the bloodstream compared to other carbs, proteins and fats? This is especially true as we get older. As a result, they can build up in the small intestine and over-feed intestinal bacteria. These over-fed bacteria grow and produce excessive amount of gas which, I believe, drives acid reflux as a result of the pressure created in the small intestine and stomach.
As little as 30 grams of unabsorbed carbohydrate can produce more than ten liters of hydrogen gas in the small intestine. It’s like the “Mentos in a coke bottle” effect. The gas pressure forces the lower esophageal sphincter (LES) to open allowing stomach contents to enter the esophagus.
This perspective is new and subject to additional testing in the clinical setting, but there is considerable scientific evidence supporting this explanation. And since this idea is simply a variation on low carb dieting, there’s not much harm giving it a try before reaching for the purple pill bottle.
Here’s the diet: Limit foods containing the most difficult to digest carbohydrates, such as lactose, fructose, fiber, resistant starch, and sugar alcohols. These include some dairy, sugar, honey, most starches, whole grain products and fruits. There are no limits on proteins and fats.
Jasmine rice and white bread in moderation are easier to digest and less likely to provoke symptoms. For fruits, watermelon, cantaloupe and strawberries are good choices. If you are eating pizza, enjoy the toppings but not the dough. Most cheeses are ok because most of the lactose sugar is already fermented. If you are preparing a fried food, fry it without the flour-based batter. Yogurt is OK as long as it’s plain (you can use stevia). Coffee is fine as long as you don’t add sugar and milk, instead use cream and stevia. Fruit juices are problematic because of their sugar content. Alcoholic drinks are OK as long as they don’t contain much sugar.
When you do consume carbs, select fully ripened vegetables and fruits, cook starchy foods well and consume them fresh (not cooled and reheated), employ pro-digestion strategies for starches, such as eating slowly and chewing well to allow amylase enzyme in your saliva time to digest starches.
It’s also important to identify and address any additional underlying causes of small intestinal bacterial overgrowth (SIBO) or dysbiosis: motility issues, lactose intolerance, low stomach acid, antibiotics, etc., on a case by case basis. You can be tested for SIBO with a breath test.
In addition, you may also want to examine any medications and/or supplements you are taking for side effects and/or symptom-causing ingredients. Many medications and supplements can exacerbate acid reflux. Taking digestive enzymes such as lactase or amylase can also help.
Feel free to give me a holler if you want to know more. We can talk over a light beer — regular beer has too much resistant starch. Dry, not sweet wine is another option. How does that sound?
Most respectfully,
Norm Robillard, Ph.D.
Norman Robillard, Ph.D. is the founder of Digestive Health Institute and author of the Fast Tract Digestion book series, including heartburn and IBS. A former research scientist who devoted his career to developing new drugs for 20 years, Dr. Robillard made a career change after he discovered the power of diet for his own digestive health. He now works with those seeking science-based alternatives for their digestive health issues, instead of drugs or antibiotics. He serves as a scientific board member for the Nutrition & Metabolism Society. Dr. Robillard received his Ph.D. from the University of Massachusetts, Amherst and completed his post-doctoral training at Tufts University.



I almost immediately made changes in my life after reading Fast Track Digestion and have found that my energy level increased once I halted consumption of processed foods/sugar in my diet and halted heartburn issues. A must read… sharing the information with others will create a much less drug dependent society.
Wonderful news Paula. Thanks! Hear that Mr. President?
Dear Mr. President Obama
Chewing a piece of fresh ginger or drinking fresh ginger juice daily or after each meal will take care of the problem. Conventional medicine is not the best treatment for acid reflux.
Thank you, and wish you the best.
I also came to exactly these conclusions , from an Engineering background, never having seen any of this Medical/Biological study.
Quite an emotional moment to read this article.
I’ve made it into the 13% that survive Esophageal Cancer.
Caused by Barrettt’s Syndrome.
Caused by Acid Reflux
My feeling, when being prescribed PPIs in the past was, that the words “Proton Pump Inhibitor” sounded solid and powerful and almost understandable. Perhaps in a world of esoteric, polysyllabic medicines, they were like a comfort blanket, to both the Doctor and the Patient?
The mention of Hydrogen was very interesting, would that lead to Hydrogen Sulphide production? Is the process Fermentation?
New life problem is Acid entering my lungs, from a smaller, much higher stomach.
No prizes for guessing which class of drugs are being pressed upon me!
I’m solving it myself via dietary changes.
Tricky, bedause the Acid fumes have also cost me all my teeth.
Thank you for this Article.
Hi Ivor, I commend you on researching your condition with life-saving results.
The biochemistry of intestinal gases is indeed interesting. Gut microbiota are quite diverse, but can be broken down into fermentative bacteria and hydrogenotrophs. Fermentative bacteria predominate and produce short-chain fatty acids (SCFAs), H2 and CO2. Hydrogenotrophs consume the hydrogen produced by fermentative bacteria. Archaea organisms, the most predominant one being M. smithii (look like bacteria, but they’re not) use the hydrogen to produce methane (linked to constipation), while sulfate-reducing-bacteria (SRB) including Desulfobacter, Desulomonas, Desulfotomaculum, Desulfovibrio and Desulobulbus use hydrogen and sulfate to produce hydrogen sulfide (toxic and detoxified by other microbes), while acetogen type bacteria use hydrogen to produce acetate.
All of these anaerobic microbes (hate oxygen) compete for the hydrogen.
TMI? If not, here are a couple of good references:
https://microbewiki.kenyon.edu/index.php/Gut_hydrogenotrophs
https://www.nature.com/ajgsup/journal/v1/n1/full/ajgsup20126a.html
Great post! Hopefully Mr.Obama’s doctors will pay attention to this.
Hi Alexandra,
I hope so too. We did send a book to his doctor.
Well, Norm, you made my day :) One of your best blog posts yet. (And, hardly stream of consciousness ;) This is an excellent post to send to ANY lay person. Thanks for writing it!
P.S. Did you find the burp screen clip?
Thanks Bearsmom. Thanks! Yes, I did find the burp clip, but it was somewhat subtle. None-the-less, consistent with, but not 100% specific to acid reflux.
Loved this concise and informative letter!! Am reading your book now, feeling hopeful about starting diet, but worried I will lose weight. Main symptom is throat mucous.
In letter you wrote about how some supplements can cause symptoms. Can taking vitamins cause symptoms (specifically multivitamins and Vitamin D)? Also, how do you check for low stomach acid? And what kind of doctor performs the breath test for SIBO?
Thanks!
Hi Patience,
Vitamins should not be a problem with the possible exception of high dose vitamin D. Taking moderate doses with food should be fine. Low stomach acid can be diagnosed with the Heidelberg acid test. Any doctor can order a lactulose hydrogen / methane breath test. The test can be done at home – companies that offer the test can send you a kit. You do the test at home, send in the breath samples (collected in tubes) and the company measures the hydrogen and or methane and provides the results to your doctor.
I really appreciate your response, thank you.
Would any internist also be able to do the Heidelberg acid test? If so, I will make an appointment for that test and also the lactulose hydrogen/methane breath test.
Thanks again!
The Heidelberg acid test requires a pH capsule and other equipment. You might ask your GI or call the closest teaching hospital to find our where you can get the test performed.
I don’t have a GI doctor yet, want to double check, can an internist order the breath test for SIBO?
Norm,
What do you consider high vs moderate vitamin d? Also, how does high vitamin d manifest symptoms – GERD, LPR, gas, bloating, all of the above?
I’m not sure on either of your questions, but here is a link where people report heartburn issues with Vit D and some report the actual doses they experienced problems with:
https://www.peoplespharmacy.com/2013/05/06/vitamin-d-pills-triggered-acid-reflux/
Thanks for that link. Very helpful!
Hi Norm, many thanks for your work. My issues are more mental fogginess that goes in tandem with bloating. The trouble is when I chew my food thoroughly I actually get more bloating, so much so that I cant stand to continue more than a week. I cant think how this can be, any ideas?
Thanks,
Colin
I don’t hear that a lot Colin (more chewing and more bloating). But there is a rational involving advanced SIBO in the early part of the small intestine, where even simple carbs can drive overgrowth and symptoms. I would need more info and you would have to enroll in our consultation program to pursue this further.
Thanks Norm!
Hi Colin
I suggest you come over to the forum you can get lots of help from other forum participants and post all your diet and symptom questions. It is highly likely that something you are eating is driving your bloating, rather than the act of chewing well. Without knowing specifically what you are eating every day it would be hard to help. Feel free to post your daily diet (here, or over in the forum).
All the best!
Ok, thanks bearsmom!
Hi norm
Greetings from South Africa. I’m a 32 year old minister in the Cape and was diagnosed with laryngopharyngeal reflux early jan. I was quite flabbergasted actually because I’ve never experienced heart burn symptoms. The only symptom I have is the lump in throat sensation and voice fatigue. Obviously being a speaker for living this is super concerning. I was elated to hear there was no voice damage, but somehow this LPR thing sounds horrific. I was given ppi’s but after week I felt terrible. I mean I’m 32 and top fit and my only issue is a bit of constipation every now and then. After scouring the net for some answers across some diets but somehow your advice makes sense and I bought your book.
So I’ve dropped the ppi’s and changed the diet. Here in South Africa The tim noakes banting diet is big. Other than some obvious differences there area lot of similarities. So I’ve merged his ideas with your FP indicators. Been on the diet for 2 days. Still have the lump in the throat sensation at times. I’ve got suspicion that diary might be one of my issues. How long does it usually take to see real progress with this issue. I also think my body needs to readjust after a week of ppi’s.
Thanks for your work. Hope to hear from you.
Regards
Ruan Serfontein
Hi Ruan,
Sounds like you’re on top of things. The Fast Tract Diet with Tim’s input should do the trick. LPR-related symptoms do take longer to respond to diet changes compared to simple heartburn. Give the diet a month or two and you will see big changes. Just be diligent with the diet keeping FP levels as low as possible. Once you are better, you can experiment a little more – but not before.
Hi Nirm thanks di much for your work. I have has gerd for almost 2 years! Ppis worked at the beginning but not any longer . Carafate and Zantac work but not always. I am beyond frustrated. I will start the diet tomorrow! I have a question. The book says in the chart that brown sugar and sugar have a low index. But this article says otherwise. I am a bit confused. Can u please shed some light? Thanks so much!!
Hi Carla,
I can appreciate your question. One teaspoon of brown or white sugar (about 5 grams) only has 2 grams of FP. Not too bad, but it can add up throughout the day. For instance, one Coke has 39 grams of sugar – about 14 grams FP. Good luck on the diet! Please do report your progress and consider sharing your experience on the forum.
Hi Dr. Norm! Now I understand!! Thanks so much for getting back to me so quickly! I am excited about the diet since I may be able to have my cup of coffee with light cream and maybe 1 teaspoon of sugar. I used to drink my coffee with bread or pastry and I wonder if it was the carbs and no the coffee that created the issues. Anyways, thanks again I will definitely report my progress!
Regards
Dear Doc
Great post. I’m following Tim Noakes way of eating – have been for years.
On top of chronic acid reflux, I get migraines from tannin. Had them for 30 years since 8 years old. Is there a link between acid reflux and tannin? Funnily enough, tannin rich foods give me acid reflux too!
Nicole
Hi Nicole. Tim is awesome! Very interesting comment about tannin. I have not heard of tannins exacerbating acid reflux, but let us know if you dig up any good info on this.
Hey I just brought your book for IBS. My problem is as soon as I eat something my stomach bloats stays for couple of hours and mild constipation and I can’t digest meat. It just stays in my stomach. As per your book it says start with high protein food. Is there any alertnative suggestion for me. I have been antibiotics for hpylori which caused me this indigestion problem. having hard time literally digesting any thing else than plain white rice which is high carb causes more bloating . Please suggest me where can I start the diet from.
Hi Rajpal, The effects of antibiotics are hard to predict, but one thing we do know is that the microbes in your gut are impacted and it will take some time for them to recover. Typically plant-based foods are the most problematic for people with unbalanced gut microbes, but it certainly is possible that your situation is unique. I can’t give you further individual advice outside our consultation program as I don’t know the details behind your situation.
Hi Dr. Norm,
What is the best and safest way to treat chronic indigestion and now GERD?
Read Fast Tract Digestion Heartburn and get the Fast Tract Diet Mobile App. That’s why I created this diet.
I don’t have a smart phone or a tablet for the App. Is there any chance it will work on my computer?. I have your book with the lists of foods, but it’s pretty limited. How can I get updates of your food lists? It would be really helpful.
Thanks.
Hi Susan, The app is the only way to get the expanded list. The app works on android or apple phones and tablets, but I don’t believe it will work on any PCs. Might be time to treat you self to a new device!
Hi Norm,
Thanks for the Fast Tract App. I have been working with a Functional Medicine practitioner for a few months now to help get my energy back, get better blood pressure regulation, and get a handle on GERD/Barrett’s. I have been doing pretty well, but finding that the reflux comes up at 4 or 5 in the morning. Not as intense as before, but still there. So far, my blood pressure is much better and less reactive, I have lost 10 lbs of fat, and my energy is slowly coming back. I have been using the App for about 3 weeks and find it does help me keep symptoms down. Really makes sense to me! A couple more weeks on Anti-Microbial/Anti-Yeast Diet and I will begin to transition off of some supplements. I eat lots of veggies and protein right now – oh – and good fats, too. The App really does help with choosing foods! Will all this help with reflux, even though I have a small Hiatal Hernia?
Thanks!
Hi Denise, Great to hear from you and happy you like the app. Hiatal hernia can make reflux worse, much the same way wearing tight clothes does. But regardless, reducing gas pressure from gut microbes still makes sense. The diet will help despite having the hernia.
HI Norm.
i found your website by chance, earlier this year i was diagnosed of having GERD. the doctors did an endoscopy and found everything seems to be normal. currently i am on nexium, gnanton and progutt twice daily..i am from asia, ,spicy and oily food has been our staple food and i have tried to reduce it. after reading your articles, i am convinced that it is the carbs that i should be avoiding. i have already bought your app and should i stop my medication and try the low carb ? thanks norm
Hi Norm,
Thanks for your quick and helpful reply. I am finding the diet very helpful and look forward to meeting with a GI doc in a month or so to discuss natural GERD remedies. Should be interesting! I will share the Fast Tract Info with him. He does do a program here every once in a while called that talks about “You are what you eat” and covers whole foods etc. He might find this all very intriguing!
Hi Norm,
Here’s an update: Have lost 20 pounds and have more energy. I am thinking the protein smoothie prescribed by my functional medicine practitioner may have too many carbs in it for me, since I still get some heartburn at 4 or 5 in the morning. The GI doc I saw, of course thinks I should do Zantac, Protonix or maybe get the hernia repaired with surgery, especially since I have Barrett’s already. He seemed really concerned that I was not weighing the side effects of the drugs against the possible effects of having Barretts, cancer etc.
Thanks for your research and common sense approach,