Your guide to COVID-19
This article has the following 9 parts:
- Preventative steps against COVID-19
- Who’s at risk and why?
- Critical Risk Factors for COVID-19
- How to mitigate CoV-2 risk by addressing underlying health issues
- Actions steps for addressing metabolic syndrome
- Digestive health and COVID-19
- How does our microbiota relate to CoV-2?
- Action steps for improving our gut health and avoiding SIBO
- Help is on the way for COVID-19 (therapeutic options under development)
SARS CoV-2, the virus responsible for the COVID-19 pandemic can infect the lower respiratory tract, the digestive tract, and possibly other organs. Most people who become infected have few or even no symptoms. But many people will progress to severe symptoms and become critically ill.
The world has not seen a pandemic of this magnitude since the Spanish flu in 1918. The Spanish flue infected about 500 million people or 1/3 of the world’s population at the time. It left one out of every 10 people infected dead. SARS CoV-2 is less deadly than the Spanish flu and less deadly than SARS CoV. SARS CoV is a related Coronavirus responsible for the 2002/2003 outbreak that killed 800 people.
But SARS CoV-2 spreads more easily than SARS CoV. More people have become and continue to become infected. This is why the overall death toll is so much higher. For more information about the domestic and international stats, click here.
Preventative steps against COVID-19
-
Remember that we are all in this together.
We need to make sure we don’t get infected and don’t infect others. A study in Iceland showed that up to ½ of infected people have no symptoms. The best practice is to assume you are infected and take serious steps not to infect anyone else. There are two major reasons for this. One is to make sure our hospitals, staff and equipment are not overwhelmed. Two, potential life-saving treatments (see the end of this article for more info) and vaccines are under aggressive development but need a bit more time.
-
Stay at home whenever possible.
-
Practice frequent hand washing for 20 seconds or use sanitizer when you can’t wash. (WHO recipe for sanitizer).
-
Assume every public surface is contaminated including groceries. Take appropriate actions based on what you bring into your home.
-
Keep all public and private bathrooms cleaned and sanitized since the virus can be spread by the fecal-oral route as well as exhaled droplets and contaminated surfaces.
-
Practice social distancing of 6 feet outside the home.
-
Wear a mask (preferably N95) and gloves (or sanitize your hands frequently if you don’t have gloves) when you are outside the home.

There are DIY instructions for making your own masks at home. Wearing any mask helps keep you from touching you nose or mouth even if non-N95.
-
Take special precautions when taking supplies to elderly people or people that have underlying health problems.
Who’s at risk and why?
Most people infected with CoV2 will have mild illness with no symptoms or minor symptoms, but many people will experience severe infections with severe symptoms such as:
- Persistent cough
- Fever
- Tiredness
- Respiratory distress
If you believe you may have become infected and have these symptoms, contact your healthcare provider immediately.
Critical Risk Factors for COVID-19
One of the biggest challenges in battling CoV-2 is addressing critical underlying health issues that place you at greater risk. People with the following pre-existing health issues fare much worse when infected and have a greatly elevated risk of succumbing to the infection:
- High blood pressure
- Diabetes
- Severe obesity
- Heart disease
- Asthma or COPD
- Liver or kidney problems
- Immune deficiency or autoimmune disease
Side note: The same health problems also put people at greater risk with influenza viral infections. There were approximately 45 million cases of the flu in the United States during the 2017-2018 influenza season, resulting in an estimated 810,000 flu-associated hospitalizations and an estimated 61,000 flu-associated deaths according to CDC.
Next to avoiding CoV-2 infection, the most important thing we can do right now is to start addressing these underlying health issues.
How to mitigate CoV-2 risk by addressing underlying health issues
Of course, you can look at each of these conditions individually and take actions to address or mitigate them.
For instance, liver problems are more common in alcoholics and people with long term hepatitis C infections. Kidney problems can run in families indicating a genetic link. Obesity is linked to diabetes, etc. This is an obvious approach and makes sense. You may have already had prior discussions with you doctors about these issues.
But there is an “elephant in the room”.
It’s called metabolic syndrome. Understanding what metabolic syndrome is and addressing it will dramatically reduce your risk of a severe outcome from CoV2. It also improves your health against most common chronic diseases in general including diabetes, heart disease and stroke.
What is Metabolic Syndrome?
Metabolic syndrome represents some combination of the following health issues:
- High blood pressure
- High blood sugar
- Excess body fat, especially around the waist
- High triglyceride levels
Having any of these health issues is significant. But having two or more greatly increases the likelihood that you have metabolic syndrome. Metabolic syndrome is endemic in the US and developed countries around the world. Over one third of Americans have metabolic syndrome and over half of Americans over age 60 have metabolic syndrome.
But are we getting the right advice?
Standard advice for addressing metabolic syndrome includes:
- Getting at least 30 minutes of physical activity most days
- Eating plenty of vegetables, fruits, lean protein and whole grains
- Limiting saturated fat and salt in your diet
- Maintaining a healthy weight
- Not smoking
Getting more exercise, losing weight and not smoking makes sense. But these standard dietary recommendations are “off” because the most important underlying causes of metabolic syndrome are:
- High blood sugar
- Hyperinsulinemia (too much insulin)
- Insulin resistance
How does Metabolic Syndrome develop?

But as many of us grow up and continue to consume too much sugar, junk food and overall carbohydrates including starches, the cells in our body start to become less sensitive to insulin from repeated blood sugar and insulin spikes. When this happens, our pancreas makes even more insulin. But over time, insulin resistance increases to the point where our pancreas can’t make enough insulin and blood sugar is no longer controlled.
The result is diabetes, a very dangerous disease that can lead to inflammation, cardiovascular, kidney and liver disease, and much more. Another problem is that high insulin leads to obesity and non-alcoholic fatty liver disease (NAFLD) because the metabolism of fat gets blocked by insulin.
I look at diabetes and even pre-diabetes in its simplest form as a carbohydrate intolerance. And the most important thing to focus on is controlling the amount of carbohydrates we consume.
Unfortunately, the dietary food guidelines published in 1977 promoted reducing fat and increasing carbohydrates, which resulted in significant increases in obesity, diabetes and metabolic syndrome.
Actions steps for addressing metabolic syndrome
If you have high blood pressure, diabetes, severe obesity, heart disease or kidney problems, you may suffer from metabolic syndrome. Take these steps to address metabolic syndrome but be sure to check with your doctor first to make sure these interventions are right for you:
-
Have a look at your last comprehensive blood test to see if you had high fasting blood sugar or high HbA1C results which measures a 3-month average of blood sugar. If your levels are high, you may have diabetes or pre-diabetes.
-
Consider reducing your overall carbohydrates including sugar, sweets, junk food and grains / starches such as bread, rice, potatoes and pasta.
-
To offset the reduction in carbohydrate calories, increase protein, but most importantly increase fats including monounsaturated fats or MUFAs (nuts, seeds, olives and avocados) and saturated fats (eggs, cheese, butter, ghee, coconut oil and meats). Our body also requires small amounts of essential polyunsaturated fats or PUFAs including omega 3 (oily fish, nuts and seeds – we don’t get enough) and omega 6-fatty acids (vegetable oils, nuts, seeds, meat and eggs – oversupplied in our diet).
One caveat concerning polyunsaturated fats is that they are sensitive to oxidation (form inflammatory end products) so limiting highly processed vegetable oils and limiting cooking at high temps makes sense. If you have concerns about including (more) saturated fats in your diet, I recommend reading The Big Fat Surprise: Why Butter, Meat and Cheese Belong in a Healthy Diet and Eat Rich, Live Long: Mastering the Low-Carb & Keto Spectrum for Weight Loss and Longevity.
-
Consider intermittent and extended fasting. Fasting is the ultimate way to reduce your blood sugar, insulin levels and insulin resistance and is quite healthy for most people.
This is not for children or teens, though they should limit sugar intake. I recommend following the work of Jason Fung in this area including his book The Diabetes Code. Importantly, talk to your doctor to be sure you don’t have conditions which preclude fasting or present special challenges with fasting such as pregnancy, nursing, or being on diabetes medications.
Medications such as insulin can result in hypoglycemia or dangerously low blood sugar when fasting. Your doctor may tell you to reduce how much insulin you take as you begin fasting. Also, make sure you have enough fat stores in your body to allow for fasting since this is where your calories will come from. It takes just a bit over one half pound of fat to supply your caloric needs for the day.
Reducing overall carbohydrates is also possible on a plant-based diet though it takes a bit more effort since most carbohydrates come from plants. Luckily, most green leafy vegetables are relatively low in carbohydrates and there are healthy fats in coconut oil, ghee, avocado and other cold pressed nut oils.
Digestive health in COVID-19
Up to half of Covid-19 patients experience gastrointestinal symptoms including diarrhea, loss of appetite, vomiting or abdominal pain. Some people have GI symptoms even before other common symptoms show up. In these cases, the GI symptoms are first sign of illness. People with GI symptoms tend to have worse outcomes and take longer to recover from Covid-19.
The most likely reason for this is due to the cellular receptor in our body called ACE2 that CoV-2 binds to in order to get into our cells. This ACE2 receptor is present on cells in our lung, heart, liver, blood vessels and other organs.
These receptors are upregulated (increased) in liver cells during CoV-2 infection which may explain mild liver damage observed in some patients. ACE2 is also prevalent on cells that line the small intestine. Infection of these cells results in a stomach flu-like illness resulting in viral particles being shed in the fecal stream which allow for fecal oral route of infection.
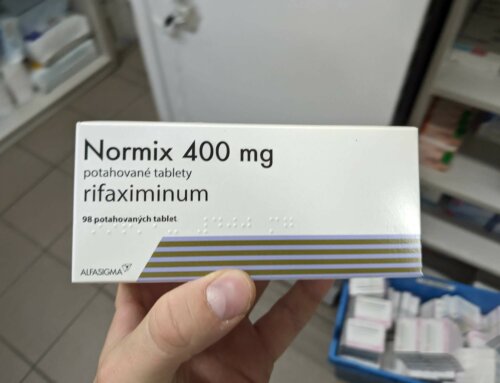
Another important question is how viable viral particles survive passage through the stomach which typically is very acidic. Though CoV-2 can survive at least down to pH 3 (moderately acidic), the healthy stomach can reach a pH 1-2 which might be acidic enough to kill the virus (not known for sure) based on canine coronavirus being inactivated at extreme acidic pH. For this reason, people taking acid reducing medicines particularly PPIs and H2 blockers which raise the pH (less acidic), may very well benefit (reduce their risk of GI infection) from weaning off these medicines. Talk to your doctor about this.
How does our microbiota relate to CoV-2?
Many digestive and general health issues are linked to SIBO (Small Intestinal Bacterial Overgrowth) including IBS, GERD, autoimmune conditions, rosacea, celiac and Crohn’s disease, interstitial cystitis, fibromyalgia, Parkinson’s and more. SIBO is also linked to some of the health conditions listed as risk factors for more severe outcome with CoV-2. These include asthma (also see asthma link via acid and non-acid reflux), coronary artery disease, diabetes, liver disease (NAFLD) and metabolic syndrome.
There is also a connection between ACE2 receptor and the microbiome, potentially highlighting a relationship between our gut microbes, cardiovascular health and CoV-2. ACE2 is also required for amino acid transport helping breakdown of protein digestion get absorbed into the blood stream.
ACE2 has an impact on our microbiota populations. Animals with mutations in their ACE2 receptor genes had lower levels of expression of antimicrobial peptides and altered gut microbial composition. As highlighted in my book Fast Tract Digestion Heartburn, changes in gut microbe populations have the potential to impact respiratory health including asthma (one of the risk factors of CoV-2) via acid and non-acid reflux.
Though it’s too early to fully understand the impact of CoV-2 on our microbiota, a healthy gut microbiota supports a healthy immune system while unbalanced or dysbiotic microbiota can increase inflammation and disrupt intestinal barrier dysfunction, i.e. leaky gut. In the case of CoV2 GI infection, leaky gut may allow more viral particles produced in the intestines to enter the blood stream making the infection worse.
Action steps for improving our gut health and avoiding SIBO
-
Limit overall carbohydrates, particularly “fermentable carbohydrates” which include lactose,
fructose, resistant starch, fiber and sugar alcohols. These fermentable carbohydrates are more difficult to digest and more likely to promote SIBO
-
Practice pro-digestion behaviors and practices such as eating slowly and chewing well, leaving 5 hr breaks between meals, supplementing with digestive enzymes and more.
-
Identify and address underlying causes that are specific to your case. There are 25-30 of these, and this is an active area of research that I am heavily involved in including consultation in this area.
-
Wean off acid reducing PPIs and H2 meds if possible. Talk to your doctor and try the Fast Tract Diet to address GERD, LPR, IBS and SIBO holistically.
For more information on addressing SIBO and related conditions, read one of the Fast Tract Digestion books, get the Fast Tract Diet mobile app and join the Fast Tract Diet FB group. If you need individualized help, contact me.
Help is on the way for COVID-19
While we do our best to practice the preventative measures and work to address the risk factors, incredible therapeutic options are under development:
-
-
The FDA-approved ivermectin, an anti-parasitic agent effective in vitro against SARS CoV-2
-
Convalescent serum-based therapies. When people recover from COVID-19, they gain immunity.
One important component of this immunity is specific antibodies that recognize the virus which block the virus from being infective and direct the immune system against the virus. Using convalescent serum/antibodies can help others who are sick.
-
Vaccine development based on the viral spike protein (more details) other viral proteins, as well as a new RNA-based vaccine called mRNA-1273.
One important difference between the 1918 Spanish flu and this new CoV-2 outbreak is the amazing advancement of molecular biology and genetics and experience from studying the viruses from previous SARS CoV and MERS outbreaks.
-
An Ace2 soluble receptor therapeutic and preventative. Because CoV-2 Spike protein binds to the same ACE2 cellular receptor (to get into our cells) as SARS CoV from 2002, we know a lot about this receptor thanks to a team lead by researcher Josef Penninger.
Now there is evidence that this ACE2 soluble receptor drug blocks the virus in human cells and has already undergone phase 1 and 2 human trials!
-
Other existing drugs such as lopinavir/ritonavir (less promising), favilavir (more promising), remdesivir (more promising, U. Chicago trial update) and hydroxychloroquine (unclear efficacy) are also being tested.
-
Another fascinating possibility in the works is using existing (already approved for autoimmune illnesses) anti-cytokine therapies (such as anti-IL-6 and anti-TNF meds) that block the actions of inflammatory cytokines.
While these cytokines rev up the immune response to help kill bacteria and viruses, if they rev things up too much you get a “cytokine storm” believed to be one of the major events in end-stage COVID-19 infections.
Be sure to discuss with your doctor as these are powerful medicines with several possible side effects and health risks.
-
Here’s a summary of many drugs and vaccines in development
-
Various nutritional supplements (Vit A, Bs, C, D, E, omega 3 PUFA, Selenium, Zinc, Iron, etc.) are also being evaluated based on past viral studies suggesting the possibility that they may help combat the virus.
-
Keep up with the latest info on repurposed drugs to treat Covid-19 based on a team lead by Dr. David Fajgenbaum with a link to their database
-




And insulin has a partner in health and sickness called leptin. Here’s a great discussion between Ivor Cummins and Dr Ron Rosedale on Leptin-resistance (and its connection to inflammatory cytokines), metabolic syndrome and Covid-19. https://thefatemperor.com/ep67-ron-rosedale-md-crucial-explanation-on-how-to-avoid-serious-viral-impacts/
Interesting info on the connection between increased blood glucose levels and inflammatory cytokines during viral infection (influenza in this case). https://bit.ly/34KAKou