Thanks to Bruce Miller, who posts on this site, for bringing this article, “Discovery of virus that ‘eats’ bacteria that causes C.diff could spell the end for hospital superbug“, to my attention. Let’s take a look at this research. Could treatment with viruses really “spell the end” for C. diff?
Dr. Martha Clokie, at Leicester’s Department of Infection, Immunity and Inflammation, citing the emerging resistance to antibiotics, led the preliminary work identifying viruses that were 90 per cent effective against the most dangerous strains of the C diff. In the next stage of development they plan to use a mixture of the most effective viruses in phase I clinical trials in people. with the help of pharmaceutical company AmpliPhi. Though this is very early work (phase I studies examine toxicity, phase II set the dosing and phase III test the effectiveness), there is a lot of history behind this approach.
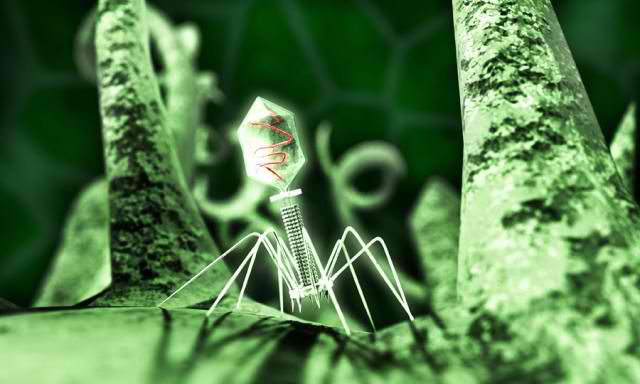
In graduate school, I spent a good bit of time studying these types of viruses, called “phages”, that infect bacteria. By the way, they don’t harm humans. There are many thousands of different stains of these phages, each one is very specific only infecting individual species of bacteria.
They look pretty scary under the electron microscope resembling a hypodermic needle with claws. And that’s essentially what they are. They target and adhere to the surface of susceptible bacteria and inject their DNA (or RNA) it to cell. Once inside, they hijack the cell to reproduce their genes and make more viral particle components. The viral components self assemble with the genes into thousands of new viruses. Their final insult is to produce enzymes which cause the cells to burst open releasing the viruses upon their death. The new viruses then go on to infect even more bacteria. Here’s an animation of what the process looks like. Her’s another.
Phage therapy is not new. Discovery in the late 1800s and early 1900s of the therapeutic promise of phages is shared between several English, Russian and Canadian biologists including Ernest Hankin, Nikolay Gamaleya, Frederick Twort and Felix d’Herelle. d’Herrelle gets a lot of the credit for the therapeutic use of phages because of an observation he made while investigating an outbreak of severe hemorrhagic dysentery among French troops stationed on the outskirts of Paris. Basically, he found that a bacterium-free filtrate made from patient fecal samples could kill the causative Shigella bacterium. He soon went on to test the safety and effectiveness of this new medicine by first drinking it himself to make sure it was safe and then giving it to a 12-year-old boy with severe dysentery. The boy’s symptoms ceased after treatment and he fully recovered within a few days. You can read the whole story along with several more successes using this approach for Staph, Cholera and bubonic plague and references to studies in animals and humans here.
Following the early successes, companies including Eli Lilly began to commercially prepare therapeutic phages for infections caused by staphylococci, streptococci, Escherichia coli, and other bacterial pathogens. Understandably, the early preparations were far from perfect, but instead of continuing to develop phage therapy, the discovery of powerful antibiotics replaced phages as the most commercially viable means to control infections. Luckily Russia and Georgia continued to work on phages and today are able to successfully treat some infections where the bacteria have become resistant to antibiotics. Here’s a great video by Lasha Gogokhia, an expert on this type of therapy. You can contact Dr. Gogokhia here.
As pointed out on Dr. Stephen Abedon’s phage-therapy.org site, there are many potential benefits of using these phages or viruses that infect bacteria as medical therapies. Some that stand out for treating a gut infection such as C diff include:
- Able to kill bacteria that have become resistant to antibiotics.
- More effective against some bacteria than antibiotics.
- Very specific – the phages specific for C diff won’t kill other healthy gut microbes. This is a huge advantage over antibiotics.
- As bacteria (evolve to) become phage resistant, the phages also evolve to overcome the resistance.
- Low toxicity to humans. Phages kill the bacteria but do no harm to our own cells. Also they are not chemicals, just (natural) protein and DNA. To date, numerous studies on phage therapy report virtually no serious complications.
- Lack of cross resistance. Antibiotics cause resistance in all bacteria exposed, but resistance to phage is limited to the target bacteria (also see bullet 2).
- Phages are inexpensive to isolate and produce.
- Phages can kill the targeted bacteria quickly and efficiently. They can even kill bacteria that have formed tough bio-films.
- Phages can be targeted for any type of infectious bacteria. Here’s a great (but graphic) video on treating a Staph infection inside a man’s bone with phages.
- Phages can reach the blood stream and organs and may even be able to cross the blood-brain barrier to treat brain infections.
With all these benefits, why haven’t we developed and implemented this approach across the board not only for C diff, but for a wide variety of other disease causing bacteria? There a several reasons:
- The huge success of antibiotics, discovered in the 20s, developed in the 30s and commercially produced in the 40s, arrived on the scene right as phage therapy was getting off the ground. These drugs were cheaper and had a broad spectrum making it easy to treat infections even when we weren’t sure which type of bacteria caused the infection.
- Lack of placebo-controlled studies to prove the effectiveness of phage therapy.
- Phage can be neutralized human antibodies and cleared by white blood cells essentially removing them from circulation. Much more work is needed here, but based on existing studies, this does not seem to be a show stopper. Some phages have longer 1/2 lives than others and the 1/2 life might be something that can be modified.
- Bacteria can become resistant to the phage. This is a potential problem, but estimates suggest that resistance to antibiotics is ten times higher.
- More work is needed here to fully understand how phage particles can disseminate to and persist in all parts of the human body (pharmacokinetics).
- Lack of broad spectrum. The narrow specificity of phages for particular bacterial strains limits the damage they do to friendly (commensal) bacteria. This is important in treating gut infections such as C diff, but it also makes them useless without matching the infecting bacterium to the specific phage that kills it. Good diagnostics are needed up front before treating an infection.
Given the amazing potential of phage therapy along with the ability of modern molecular, biochemical and genetic techniques available to address the current limitations with phage therapy, it seems like a no brainer that we need to develop these therapies now. Soon we won’t have a choice as we are heading back towards the pre-antibiotic error when the overuse of antibiotics and lack of significant progress developing new antibiotics renders our current arsenal useless against multi-drug-resistant bacterial infections.
C diff is a perfect target for phage therapy for several reasons.
- C diff makes antibiotic resistant spores making it very difficult to kill off completely with antibiotics.
- Broad spectrum antibiotics needed to (hopefully) achieve success with C diff also wipe out a huge number of friendly gut bacteria needed for our health – no such problem exists with phage therapy.
- There are many phages identified (as cited in the original article) that are effective against C diff.
- Phages have proven effectiveness with gastrointestinal infections.
Note: Another extremely promising approach for treating C diff infections know as fecal transplantation has a 98% success rate.
What do you think? Please share your comments.






Dear Dr. Robillard,
I am interested in phage therapy because I have had 7 serious infections in 2014. The current infection I am dealing with now is C. Diff, which was diagnosed when I was a asymptomatic. How can I obtain phages if I want to use then to treat my infections. Also, I have lupus and an a kidney dialysis patient and am wondering if either if these conditions contraindicate the use if phage therapy. Thank you for your response!
Sincerely,
Caroline
Dads dying of c diff/antbotics not working
Hi Tammy and also Caroline,
If antibiotics don’t work the best solution may be a fecal microbiota transplant (FMT). I recommend contacting a teaching hospital that can provide the treatment. Dr. Colleen Kelly for example, is a GI who has a great deal of experience in this procedure. https://www.womensmedicine.org/fecal-transplantation-providers.html. I attended her lecture at Digestive Disease Week 2013. Dr. Kelly is a leader in the field. Her office could likely make a recommendation for where to get treatment.