Most people have never heard about a protein called vinculin, but a recent study of 165 IBS, 30 IBD and 26 healthy controls found that people with IBS have higher levels of (auto) antibodies to this protein than do healthy controls or people with inflammatory bowel disease.
One possible outcome of this work is a specific diagnostic blood test for IBS that can distinguish this condition from IBD. But the findings from this multicenter study, led by Dr. Mark Pimentel of Cedars-Sinai Medical Center in collaboration with researchers from Beth Israel Deaconess Medical GAS in Boston could shed more light on how IBS develops and lead to alternative treatment approaches for this condition.
Vinculin is what’s called a “cytoskeletal protein”, and is found at junctions between cells as well as junctions between cells and extra cellular matrices. Vinculin appears to help anchor a filamentous protein called F-actin which helps muscles contract, but also helps the immune system fight off pathogenic bacteria.
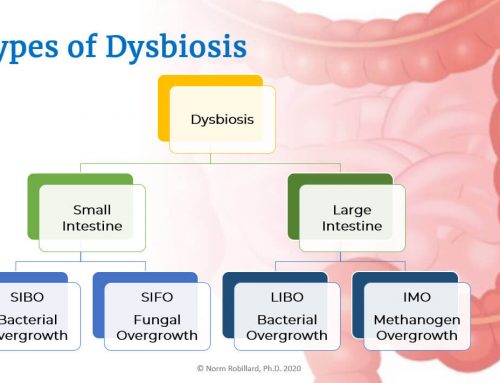
One cause of IBS is having a previous bout of gastroenteritis (a gut infection) which often triggers small intestinal bacterial overgrowth (SIBO). The idea behind this study is that a bacterial toxin called cytolethal distending toxin B (CdtB) produced by gram negative Proteobacteria (such as Shigella dysenteriae, Campylobacter jejuni, Salmonella enterica and E. coli), triggers gastroenteritis, and by molecular mimicry stimulates auto-antibodies to vinculin. This process may be involved eventual development of IBS, though the details of how this happens are far from clear. Studying antibody titers to vinculin in IBS patients can establish the role of gastroenteritis in IBS and help determine the extent to which autoimmune processes are involved.
Clearly vinculin is relevant to gut infections as another study showed that Shigella flexneri (another Proteobacteria pathogen), which causes a form of dysentery, secretes an invasion protein called IpaA which binds to the vinculin to facilitate the bacteria’s entry into cells that line the intestine. How this all ties together will be an interesting story to follow.




Excellent article Dr. Robillard! There is also some evidence that GERD could have autoimmune “root” (i think you saw this article already, but here is the link https://www.newswise.com/articles/reflux-esophagitis-due-to-immune-reaction-not-acute-acid-burn-ut-southwestern-researchers-report )
Maybe this information can help to understand the process of healing for those who don’t respond quickly at low FP diet (as in my case). Maybe such people need some restricion in pro-inflammatory or pro-autoimmune foods? (like it is described in the recent book The Paleo Approach: Reverse Autoimmune Disease, Heal Your Body written by Sarah Ballantyne).
Thanks Alexandra. I had seen that article. While I’m interested in seeing where they go with this research, the triggering event, even in this case, is the insult on the esophagus from reflux involving a combination of damaging ingredients such as acid, bile, enzymes and possibly bacteria or bacterial toxins. So I am convinced that stopping reflux is the key. By the way, was that your review on Amazon this morning? If so, thank you! I enjoyed reading it.
Me too, i think that the most important is to stop gas from bacteria.
It’s just like two paralleling jobs: to work with bacterias (by following low FP) and to work with any linked condition (like maybe some autoimmune process promoting inflammation).
PS Yes, it is my review at Amazon! My writing style is recognisable :) I’m glad that you liked it! I hope that more reviews will appear to promote people to read your great book!
I think the symptoms of SIBO and autoimmune reactions both caused by leaky gut triggered by SIBO and/or dysbiosis, so the diet that best controls this overgrowth should be the best for both problems. Of course any other factors, such as gluten removal in some cases are also important. That’s why I am working on the next Fast Tract book that will address autoimmune conditions.
Thanks again for the review. : )
Great news! Looking forward to see your new book!
Happy to hear that a book on autoimmune disorders is planned for your series. I’m currently reading The Paleo Approach mentioned above, and would love to see what you and Sarah Ballantyne would come up with if you conferred & learned from each other.
For me part of what gets lost in this debate is the fact that the Fast Track Diet alone may clear up the issues for people and is honestly so much less restrictive than Auto-Immune Paleo diet. I tried for 2 years to figure out what my trigger foods were that were causing all my digestive symptoms. My holistic doctor did not really want me on a total elimination diet and I was really stuck. Using the Fast Track approach yeilded quick results and is relatively easy to accomplish if one is used to cooking with whole foods. I am looking forward to further improvements. It would only be after about 3 months on the Fast Track Diet that I would start looking into other immune issues, seek testing, or take out other foods. Given the presentation of my symptoms they are in line with SIBO symptoms (even if there might be some crossover into auto-immune) and so reducing the microbial burden alone to see if this reduces inflammation and enhances nutrient absorbtion, this seems a prudent and also a reasonable way to go and honestly way less restrictive than AIPaleo.
I agree with you Bearsmom in this regard. Inflammation caused by either a GI infection or SIBO itself can lead to leaky gut and autoimmunity. The fist step is stopping the insult leading to leaky gut. The Fast Tract Diet is directed at this most basic problem.
I have been basically trying to apply the principles of SIBO diet to my Auto Immune Ankylosing Spondilitis (AS), since it seems to me that AS is a SIBO by Klebsiella bacteria & there are phenomenal similarities between Croh’s & AS intestinal tissues. Have had dramatic results with the NO starch, no dairy (except with a lactase enzyme tab), including going off all meds, reducing stiffness & pain most of the time. However, the very slightest mini mistake with a food choice (often some hidden starch or hidden lactose when eating away from home), leaves me totally vulnerable, and I am back to square one with the pain, immobility/stiffness in no time flat. Used to take me 10 days to get back to feeling stable again, but I have shortened that period to only 48-72hr by immediately avoiding ALL fiber (no vegies, no fruit, just protein foods and a very low fiber homemade strained juice). Somewhere I read that Klebs does not feed/grow on vegie fiber, however I have a hard time believing that. Perhaps you being a microbiologist researcher can confirm if that is indeed the case or not.
This all leads me to believe that I am only controlling/reducing their (Klebs bacteria ) population, but not eradicating them (even tried Dr Seibecker’s herbal antimicrobial protocol via Biotics Research 2 products, among numerous other things, short of antibiotics, with no apparent results).
I do have your Fast Track IBS ebook, found it quite informative, yet I think I am already more dietary restrictive than in your book.
Can you please shed some light on your experiences/knowledge with treating AS, before I head for the Elemental diet or antibiotics as a last resort?
Thanks so much for your work on Digestive Health !
Dear. Dr. Norm,
I have been dealing with “some sort” of autoimmune for 3 years. I have seen 4 rheumatologists. They have all come up with the same diagnosis. They honestly do not know what I have…. but they have been treating me with steroids, rituximab plaqunil, injectable Methotrexate, Enbrel, and many other biologics. The only medication that works is prednisone. I am at the point now that I have no where to turn. I recently saw a GI doc. he is trying to see if there is any issues with my GI tract that could help me find out what is wrong with me. I read your article and am wondering if you could give me your thoughts?? I am really desperate.