Are you familiar with the term, Functional Gastrointestinal Disorders (FGIDs)? Don’t let this five-letter acronym intimidate you. It simply refers to conditions or symptoms affecting the digestive tract for which no structural problem or biochemical cause is observed by standard testing such as endoscopy, imaging or blood tests.
These are some examples of FGIDs:
- Irritable bowel syndrome (IBS)
- Idiopathic or functional diarrhea
- Idiopathic or functional constipation
- Functional bloating or distention
- Functional dyspepsia (indigestion, full feeling in upper abdomen)
- Functional heartburn and other symptoms of acid reflux and laryngopharangeal reflux (LPR) including globus (feeling a lump or something stuck in your throat)
The “functional” means that “everything seems to be working or functioning” through routine testing. The term “idiopathic” is also common in describing FGIDs, indicating that the cause is “unknown.”
There are many more, but you get the idea. These conditions are painful, debilitating and often chronic lasting for years or even decades. FGIDs affect millions of people resulting in almost half of our trips to the doctor’s office [i] and an estimated cost of 25 billion dollars annually.
What are the common treatments for these conditions?
By definition, mainstream medicine is telling us that:
- There is nothing wrong with you according to the tests
- The cause of these ailments is unknown
- Here is some medicine for your symptoms
A cynic might conclude that there is a financial incentive in the status quo. But the problem goes beyond money. These medications are aimed at the symptoms and don’t address the underlying causes for the most part. Also, most of them carry potential serious side effects and health risks.
These are common examples:
| Indication | Medication | Side Effects and Health Risks |
| Abdominal pain and diarrhea | Antispasmotics (hyoscyamine, dicyclomine) | Dry mouth, confusion, dizziness, headache, forgetfulness, hallucinations, unsteadiness, coma, anxiety, tiredness, insomnia, excitement, mood disorders, blurred vision, constipation, difficulty breathing or swallowing |
| Diarrhea | Anti-diarrheal medications containing loperamide | Abdominal pain, bloating, nausea, vomiting and constipation |
| Diarrhea | Alosetron (Lotronex) | Removed from market, then reintroduced for women with sever IBSD. Severe constipation |
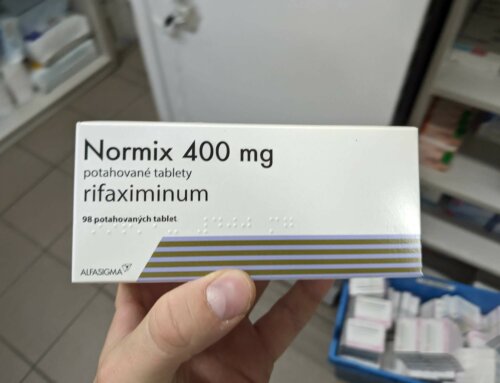
| Diarrhea predominant IBSD | Antibiotics | Bacterial resistance, dysbiosis (unbalanced microbiota), C. diff infection, allergic reactions |
| Constipation | Osmotic, lubricating and stimulant laxatives | Nausea, bloating, abdominal pain, cramping, flatulence, diarrhea, vitamin malabsorption, dependence |
| Constipation | Tegaserod (Zelnorm) | Removed from market, then reintroduced for women under 55. Heart attack and stroke |
| Constipation predominant IBSC | Lubiprostone (Amitiza) | Nausea, diarrhea, headache, abdominal distension, flatulence, vomiting, difficulty breathing |
| Constipation predominant IBSC | Linaclotide (Linzess) | Diarrhea, heartburn, vomiting, gas, bloating, headache |
| IBS | Antidepressants including tricyclic and selective serotonin reuptake inhibitors (The side effects are worse for the tricyclic medications) | Constipation, cramps, nausea, vomiting fatigue, headaches, difficulty urinating and more. |
| Heartburn, acid reflux and LPR | PPIs, H2 Blockers, Antacids (the side effects mostly relate to PPIs and H2 blockers but excessive use of antacids can pose similar risks) | C diff infection, pneumonia, bone fractures, heart and kidney problems, anemia, malabsorption of: calcium, magnesium, vitamin B12 and other vitamins and minerals |
| Nausea, vomiting, heartburn | Metoclopramide (Reglan) | Diarrhea, dizziness, drowsiness, headache, nausea, vomiting, and more. |
The whole FGID concept is faulty in my view because people would not be sick if things were working or “functioning” properly. It’s about time to take a fresh look at what we already know about the underlying causes of these conditions. Perhaps, this will lead to a more sensible way to treat them at a fundamental level.
In fact we know a lot more than what we think. It’s a little like an episode of X-Files, “the answers are out there.” But they are lost in medical journals and even medical text books.
It’s all about the gas
Here is one powerful statement I found on page 1192 in “The Textbook of Primary and Acute Care Medicine,” one of the books used to train doctors:
“Dietary alterations to reduce (intestinal) gas require the elimination of most of the foods in Table 1 (which includes lactose, fructose, resistant starch, fiber and sugar alcohols)”
The connection between intestinal gas and basic FGIDs symptoms such as bloating, cramps, distention and abdominal pain is pretty straightforward. You can easily imagine lots of trapped gas causing these symptoms.
Now, if we can fully understand the connection between intestinal gas, FGIDs and these carbohydrate types (lactose, fructose, resistant starch, fiber and sugar alcohols), we should be able to translate this knowledge into an effective dietary treatment.
What are intestinal gasses and how are they produced?
Intestinal gases include hydrogen, carbon dioxide and methane. They come from bacteria fermenting carbohydrates and Archaea organisms in the case of methane. The carbohydrate types listed above have been flagged as the source of intestinal gas because they are the hardest to digest and absorb into our bloodstream. As a result, they persist in the intestine potentially fueling bacteria or Archaea organisms to produce excessive gases in our intestine – makes sense, doesn’t it?
IBS, Diarrhea and Constipation
There’s more. Hydrogen and methane also affect motility, which is how fast food moves through our digestive tract.
Most people are aware of common causes of diarrhea including: food poisoning, bacterial, viral or parasital gastrointestinal infections (gastritis) which tend to come on suddenly and resolve naturally over the course of one to several days. Most often, staying hydrated with electrolyte rich liquids is the only treatment required for these conditions.
But chronic diarrhea (after other causes such as C. diff are ruled out) may be caused by SIBO (Small Intestinal Bacterial Overgrowth) specifically involving bacteria which produce excessive amounts of hydrogen. A number of researchers including Dr. Mark Pimentel’s group at Cedar Sinai in Los Angeles have shown that IBSd patients whose gut microbes produce excessive hydrogen frequently suffer with diarrhea. [ii],[iii]
Constipation, defined as hard or lumpy stools, straining or a feeling of incomplete defecation also has many potential underlying causes including: constipating medications (i.e. especially painkillers and laxative abuse), dehydration, bowel obstruction, colon cancer, hypothyroidism or neurological problems. But newer research indicates that idiopathic constipation experienced by IBSc patients is linked to an excess of methane-producing gut microbes known as Archea. [iv],[v]
Testing via the lactulose breath test including both methane and hydrogen detection can help you determine if your symptoms are due to hydrogen or methane producing microbes.
Heartburn, LPR and Acid Reflux
I personally suffered severely from acid reflux for 20 years taking PPIs, H2 blockers and antacids without adequate relief. One day I went on a low-carb and high fat diet for weight loss, and my acid reflux symptoms vanished within a day. Astonished? Yes! And I got so CURIOUS and had to find out WHY.
As I investigated how each food type (carbohydrates, fats and proteins) was digested, a light bulb went off. Being a microbiologist, I knew that most gut bacteria prefer carbohydrates for fuel and they produce lots of the gases mentioned above. Sound familiar?
My idea was that acid reflux is actually caused by too much gas pressure in the small intestine and stomach due to intestinal bacterial overgrowth of gas-producing strains. Think of it as dropping a Mentos candy into a bottle of coke.
This concept is supported by over 100 scientific journal articles in my books, Fast Tract Digestion Heartburn and Fast Tract Digestion IBS. My theory challenges the antiquated idea that acid reflux is caused by dysfunctional lower esophageal sphincter muscles located at the top of the stomach that is designed to contain stomach contents. But the new idea suggests that gas pressure actually forces this sphincter to open. Again make sense, doesn’t it?
Here is the solution
Consuming too many foods containing the five hard-to-digest carbohydrate types is a big part of the problem. With this information, I created a science-based and drug and antibiotic-free diet to help not only people with acid reflux but also to help people with a variety of other FGIDs and systemic and autoimmune conditions involving SIBO. This diet is called the Fast Tract Diet.
The Fast Tract Diet approach quantitatively limits these hard-to-digest carbohydrates based on a mathematical equation called Fermentation Potential (FP). Think of FP as “symptom potential” in low, medium and high as well as points based on serving sizes of your food items. FP uses the glycemic index to measure the “symptom potential” in virtually any food item. And the beauty is that the math has already been done on many food items for you.
In addition to the FP calculation and food list, the Fast Tract Diet includes pro-digestion strategies to reduce the impact of hard-to-digest carbohydrates along with a process for identifying and addressing other potential underlying and contributing causes that can promote intestinal bacterial overgrowth.
To complement the Fast Tract Digestion books which fully explain the Fast Tract Diet, the Fast Tract Diet mobile app makes it easy to start the diet and to track meals and symptoms based on FP values for over 800 food items.
3 Step Action Plan for FGIDs
If you suspect that you have a FGID, these are three steps you can take:
1. Reduce the hard-to-digest carbohydrates in your diet including:
- Lactose (high lactose dairy)
- Fructose (sucrose, high fructose corn syrup, agave sweetener, and many fruits)
- Fiber (legumes, whole grains, and many fruits)
- Resistant starch (pasta, most bread, most potatoes, most rice)
- Sugar alcohols (dietetic candy and snack bars, etc.)
The Fast Tract Diet recommends several low FP alternatives for each of these food groups.
2. Incorporate Gut Friendly Practices in your daily life including:
- Chewing well to allow amylase in your saliva more time to digest starches
- Taking amylase of lactase supplemental enzymes when appropriate
- Preparing foods, particularly starches in ways to reduce resistant starch
- Selecting only fully ripe fruits and vegetables, etc.
These practices will help you digest the five hard-to-digest carbohydrate types better.
3. Identify and address other potential underlying factors that can promote bacterial (or Archea) overgrowth including:
- Motility issues from GI infections, medications, scarring, surgery, etc.
- Immune deficiencies from medications, viral infections, etc.
- Digestive enzyme deficiencies
- Antibiotics that can disrupt the microbiota
- Low stomach acid from prolonged H. pylori infection or other causes
- Ileocecal valve problems
- Food or water poisoning, gastroenteritis
- Carbohydrate intolerance
[i] Talley NJ1. Functional gastrointestinal disorders as a public health problem. Neurogastroenterol Motil. 2008 May;20 Suppl 1:121-9.
[ii] Pimentel M1, Kong Y, Park S. Breath testing to evaluate lactose intolerance in irritable bowel syndrome correlates with lactulose testing and may not reflect true lactose malabsorption. Am J Gastroenterol. 2003 Dec;98(12):2700-4.
[iii] Jahng J1, Jung IS, Choi EJ, Conklin JL, Park H. The effects of methane and hydrogen gases produced by enteric bacteria on ileal motility and colonic transit time. Neurogastroenterol Motil. 2012 Feb;24(2):185-90, e92.
[iv] Chatterjee S , Park S , Low K et al. The degree of breath methane production in IBS correlates with the severity of constipation . Am J Gastroenterol 2007 ; 102 : 837 – 41.
[v] Jahng J1, Jung IS, Choi EJ, Conklin JL, Park H. The effects of methane and hydrogen gases produced by enteric bacteria on ileal motility and colonic transit time. Neurogastroenterol Motil. 2012 Feb;24(2):185-90, e92
[/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]



How do you suggest dealing with h pylori? Best treatment? Thx!
H. pylori is one situation where antibiotics are important. Long term H. pylori infection can lead to gastritis and loss of stomach acid or excess stomach acid – depending on where in the stomach the infection is focused. With excess stomach acid you can end up with stomach or duodenal ulcers. With low acid you can end up with a variety of other problems including stomach cancer.
I would like more information on how to integrate The anti-SIBO diet and the Anti-Candida diet. I have severe chronic Candida.
I tried one of your salad recipes and felt ill afterwards.
Would I be safe to just eat salad and meat?
Hi Karen, On the Fast Tract Diet, no food is illegal, though some people are more sensitive to certain foods. You might be interested in this article on Candida and diet. https://bit.ly/1JvBrR8
Hey Norm,
Appreciate the post. I was wondering if there are certain prebiotics that are favored by CO2 producing bacteria, or bacteria that don’t produce any gas (if such a thing exists)? Do you think it would be possible to boost those bacteria, which competitively drive out the bad guys, and thereby shift the balance, while maintaining a healthy microbiome. I like the idea of your diet, but I worry it is potentially dangerous microbiome deprivation. IE you may cure acid reflux but create another problem in the process.
Thanks,
Nick
Hi Nick,
A good question! The Fast Tract Diet will not cause potentially dangerous microbiome deprivation. You may be interested in Dr. Norm’s answer for why posted on the Fast Tract Diet Q&A titled “Gut Microbes Feed or Impede?”: https://digestivehealthinstitute.org/fast-tract-diet-qa/
Hope this is helpful :)
Rhea
I read your book and tried the SIBO diet. My bloating went down but constipation got worse because I limited my fruits and vegetable intake which means less fiber. I was also really hungry. I can’t have dairy so the diet plan is hard to switch out plus I am a very busy working mom so it would be so hard to follow and do all of the recipes. Could you suggest just one bfast,lunch and dinner that is dairy free that I could follow for a week and see if that helps? I have been dealing with bloating and constipation for over 20 years and your book makes so my sense to me. I just need to see if I can alter a bit to work for me. Thank you, Brooke.cheeseman@gmail.com
I like the way you think Nick. One general thing you can do is to increase animal-based foods, which are less gas producing than plant-based foods. And when you do have plants, increase low FP over high FP. Since the Fast Tract Diet does not eliminate fermentable carbs compared to no carb or elemental diets, you are still feeding the bacteria. Your body’s mucus is also feeding them, and animal-based foods also feed them, too. My opinion is that for those of us with functional gastrointestinal issues, we are over feeding our gut microbes with too many fermentable carbs. That’s why dietary interventions that limit fermentable carbs are winning in the clinic.
Hi norm I’ve been talking ppi Prilosec for years now and everytime I stop I get horrible heartburn. Right now on it though I’m constantly bloated and have stomach pains and gas. I was wondering if I should finally stop the ppi and how to deal with my gerd. Thank you
Hi Chuck, This is what the Fast Tract Diet is all about – weaning off PPIs after you initiate the diet. I recommend you read Fast Tract Digestion Heartburn and get the mobile app. Share the ideas in the book with your doctor. For help with any part of the process, feel free to contact us via the consultation page. Good luck!
Hi. I think I posted before in the wrong area. Can you give me suggestions on how to monitor myself with the low FP foods? I’m waiting for the book, but from postings it seems after eating low FP a while, you are supposed to try certain foods and see how your body responds. I was told I don’t have LPR, and I never get heartburn, but I ended up with esophagitis and a little gastritis. At that point my chest was hurting, but still none of the typical heartburn that I remember from pregnancies. Anyway, I’ve reluctantly been on omperazole for 3 1/2 months to heal, but am slowly weaning myself off. They will scope me again next week to see if esophagus is healed. I still feel a little something at times, so I’m not sure if it’s healed. Trouble is, no food seems to make it better or worse. I don’t know how to monitor anything. I just get small feelings off and on all day for about 5 seconds at a time. How can I tell if a food is good for me or not??? So frustrating. Any advice would be helpful.
Can migraines be part of this equation? I have IBS and Acid Reflux and Migraine. Could there be a connection?
Hi! I follow the fast-track diet and it really helps my symptoms. I have chronic SIBO and various autoimmune conditions. I keep hearing about the AIP diet as a way to heal from autoimmune conditions, any thoughts. Also, there seems to be lots of discussion about the validity of IgG food sensitivity testing – do you think it’s worth the cost for someone who has autoimmune issues? Love your blog and all the excellent advice.
Hi Cheyenne, Happy to hear FTD is helping. Because SIBO can cause leaky gut and leaky gut is considered the key initial event in autoimmunity, addressing SIBO is the most critical step in recovery. There are many other things to consider – gluten, certain drugs, chemicals, toxins food components which either increase intestinal permeability promote autoimmune reactions may also need to be avoided.
But for many dietary factors, the evidence seems mixed. Many of them are either destroyed by cooking or detoxified by the body. As for IgG food sensitivity testing, I cite a study from over a decade ago for IBS (in the FTD IBS book) by Prof John Hunter Addenbrookes Hospital that found a non-significant change in IBS symptoms by people avoiding foods that generated an IgG response. Perhaps controlling leaky gut by limiting fermentable carbohydrates is the elephant in the room as opposed to eliminating foods that generate an IgG response.